Research Article
Spondylolisthesis: Types; Classification; Symptoms and Surgical Treatment of a Case
2875
Views & Citations1875
Likes & Shares
Spondylolisthesis is the displacement of one vertebra over another and is numbered up to 5 degrees according to the distance it has slid (Grade I is the minimum and grade 5 the maximum or spondyloptosis).
When the vertebra is displaced forward, it is called anterolisthesis and backwards, retrolisthesis. If it slides too far, the bone can trap the marrow or nerves. It can be unstable and cause canal stenosis and / or low back pain with movement or standing. It occurs more frequently in lumbar segments, especially in the latter (L4-L5-S1). Although it can also occur at the cervical level.
We present the case of a person affected by Gr I-II spondylolisthesis, who after the period of medical treatment and rehabilitation could not carry out his work activity or daily tasks.
Surgical treatment, when necessary, should primarily aim to restore lumbar and lumbosacral lordosis, and not just to reduce slippage itself. To achieve this goal, it is essential to analyze the spinopelvic parameters that govern the sagittal balance of the spine. The spectrum of surgical treatment ranges from spinal fusion in situ to more important lumbosacral lordosis reduction techniques.
Each technique has very specific indications, which are detailed in this article. Most of the surgical techniques recommended by the authors of this article are performed using a posterior approach, which allows better control of lumbosacral lordosis reduction.
Keywords: Isthmic spondylolisthesis, Clinical symptoms, Surgical techniques
INTRODUCTION
The spondylolisthesis comes from Latin and means “slipped vertebral body”. Degenerative spondylolisthesis is diagnosed when a vertebra slides forward over the one below.
Depending on the origin of the spondylolisthesis, it can be divided into:
- Degenerative: By degeneration of the tissues that stabilize the vertebrae (intervertebral disc, ligaments, facet joints etc.
- Isthmic: It is due to a spondylolysis, which are fracture lines or weaknesses in an area of the vertebra called “pars interticularis”, which causes insufficient support and consequent slippage.
- Traumatic: Due to blows, falls or accidents.
- Congenital: Present from birth, causes a bone deformity.
- Pathological: Because of a bone disease, for example, a tumor. Iatrogenic: a surgery that weakens the bone structures that stabilize the vertebrae can cause spondylolisthesis.
below it due to a small fracture in a piece of bone that connects the two joints on the back side of the vertebral segment.
The fracture in this small piece of bone, called pars interarticularis, is caused by tension in the bone. While the fracture tends to occur more frequently when a person is young (about 5 to 7 years old), in most people the symptoms do not appear until adulthood. There is another increase in the appearance of low back pain due to spondylolisthesis in adolescence.
It is estimated that 5 to 7% of the population has a fracture in this small piece of bone (fracture of the pars interarticularis) or a spondylolisthesis (sliding of the vertebral body), but in most cases there are no symptoms.1 He has estimated that 80% of people with spondylolisthesis never have symptoms, and if they do not become symptomatic, only 15 to 20% will ever need surgical correction.
Causes of spondylolisthesis
The pars interarticularis (“bridge between two joints”) connects the facet joint above with the one below. It is a thin piece of bone with little blood supply, which makes it susceptible to stress fractures. There may also be a fracture of the pars interarticularis without vertebral slippage. The fracture itself is known as spondylolysis. Pars interarticularis is also known as isthmus.
When this small bone fractures, it usually does not cause pain or other symptoms. Trauma is not a frequent reason for the fracture. Usually, the fracture is due to the accumulated tension, such as when taking a paper clip and folding it several times. It will finally break after enduring enough tension.
The isthmic spondylolisthesis occurs most commonly at the L5-S1 level of the spine, the lowest level of the lumbar spine. It happens rarely above this level, in L4-L5 or L3-L4. At these levels, trauma (instead of accumulated tension) is one of the most common causes of fracture.
A fracture has never been found in a newborn, so it is not considered a congenital problem. The slippage that results from the fracture is more likely to progress in youth or adolescents. The progression of this slippage in adulthood is very rare.
Usually, there is not much instability at the L5-S1 level associated with the disease because there is a large ligament (the ligament of the sacral wing) that connects the vertebral body L5 with the sacrum, which prevents the progression of the slippage of L5 on the sacrum.
Classification of spondylolisthesis
The severity of the slip is usually measured after taking a lateral view x-ray, and then rated on a scale of 1 to 4. The slip is calculated taking into account the amount that the upper vertebral body slides forward over the vertebral body lower.
- Grade 1: 25% or less of the vertebral body has slid forward
- Grade 2: 26% - 50%
- Grade 3: 51% - 75%
- Grade 4: 76% - 100%
Although it is very rare, a condition called spondyloptosis may occur, in which the L5 vertebral body slides from the sacrum into the pelvis. Fortunately, most of the landslides are grade one or two, and if they become symptomatic they can be treated without surgery.
In patients with symptomatic isthmic spondylolisthesis, the most common symptoms are, among others, the following:
Low back pain, which is often, described as deep pain in the lower back; pain that radiates to the buttocks and back of the thighs (also called root pain). Pain that worsens when standing, walking, or performing any type of activities that involve bending backwards. Pain that relieves a bit when sitting, especially in a reclined position
A feeling of tiredness in the legs and possibly numbness of legs or tingling, especially after walking. Pain that radiates below the knee and possibly to the foot.
In addition to previous pain-related symptoms, most patients with isthmic spondylolisthesis have hamstring contractures (large muscle that runs down the back of the thigh), making it difficult for them to touch their toes.
An isthmic spondylolisthesis can also become symptomatic in adults, usually when people are in their thirties and forties.
How spondylolisthesis causes pain
There are two primary forces that affect isthmic spondylolisthesis in adults.
Disk degeneration
The most common reason for low back pain in this situation is that the disc will begin to wear out. Without a form of posterior support that connects the facet joints, the intervertebral space is forced to withstand the shear forces. Normally the facet joints in the back of the spine protect the disk from friction, as they act as a limit of the shear force. When there is a fracture in the pars interarticularis, the facet joints cannot limit the shear. The discs work well as shock absorbers, but are likely to be damaged if they have to resist shear. The associated accumulated tension leads to rupture of the disc and, finally, the pain appears.
Nerve pinch
As the discs deteriorate, they become flatter and the disc offers less space for the nerve root to exit the spine (e.g., the L5 nerve root at the L5-S1 level) and the patient may present leg pain (radiculopathy or sciatica). The pain in the leg is often related to walking or standing, since in these positions the foramen (hole through which the nerve leaves the spine) is closed. When the patient sits, the foramen is larger and the pressure on the nerve is eliminated. However, the opposite can also happen, since in the sitting position the disc supports a load three times greater than in the standing position, and the loaded disc can protrude towards the foramen, which causes leg pain.
A CASE
We present the case of a 56-year-old patient with pain in the lower limbs and paresthesias in the anterior aspect of the quadriceps for years. After the conservative and rehabilitative treatment, the relevant study was carried out by means of resonance, which revealed the existence of a Gr I-II spondylolisthesis (Figure 1).

Presented with low back pain (LBP) that she rated 7/10 on a scale where 0 is no pain and 10 is maximum pain. The patient also presented with severe cramping in her legs (7/10 pain) and that she needs to custom bracing for chronic right knee issues. The patient reported seeing a physical therapist (PT) previously for these issues. The patient reported the use of pharmaceuticals to help relieve her symptoms. She stated that she was taking Baclofen, a muscle relaxer and antispasmodic agent, to alleviate her leg pain. She stated that she was taking magnesium, potassium, and glucosamine supplements to help address her leg cramps.
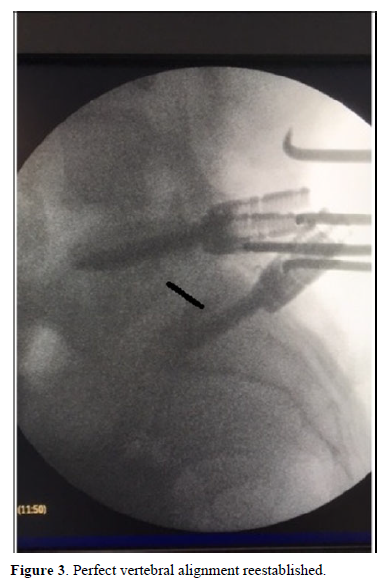
Under general anesthesia, conventional surgery was performed and fixation of the affected segment (Figure 2). Root release bilaterally and vertebral alignment reestablished (Figure 3). The patient was discharged at three days. After the mandatory RHB period that began 2 months after the surgery, the patient was free of symptoms and returned to his job.

DISCUSSION
Spondylolisthesis is called permanent anterior displacement of a vertebral body, almost always of the fifth lumbar vertebra (L5) and much less frequently of the fourth (L4) or of the higher lumbar vertebrae. In the classifications, lytic isthmic spondylolisthesis with fracture of the interarticular part are separated mostly acquired due to repeated microtrauma in childhood, and congenital spondylolisthesis with anomalies of posterior arch formation, which are usually complicated by isthmic fracture. Other causes of low lumbar spondylolisthesis (macrotraumatic, degenerative, tumor or iatrogenic surgical) are not described here.
With regard to etiopathogenesis, the existence of a genetic factor is admitted for isthmic lysis, since the white population suffers from it more than the black population, but clearly less than other populations such as, for example, Eskimo population.
The mechanical factor is evident, because only bipeds with lumbar lordosis can suffer from this disorder after starting to walk and also because the repetition of microtrauma in hyperextension during sports increases their frequency considerably. In the clinical aspect, asymptomatic forms are frequent.
Acute low back pain can manifest itself at the time the fracture occurs. At a later stage, low chronic low back pain and sometimes ciatalgia are observed, usually by compression of the L5 root.
In severe dysplastic forms, lumbosacral kyphosis can be observed with retroversion of the pelvis, hamstring retraction and knee flexion. From the radiological point of view, the diagnosis of fracture of the inter-articular parts is made from lumbar radiographic plates in oblique projection, tomographic slices perpendicular to the isthmus and bone scintigraphy in the early phase.
Spondylolisthesis is observed on lateral plates that assess, for prognostic purposes, the degree of slippage and the lumbosacral kyphosis angle. Magnetic resonance imaging makes it possible to suspect a recent lysis, evaluate the condition of the discs adjacent to the spondylolisthesis and detect a root compression cause. The natural evolution of lytic isthmic spondylolisthesis depends on the damage of the intervertebral disc.
The evolution of dysplastic spondylolisthesis is more serious, because it affects young people in the growth stage in which the deformation responds to the laws of osteocartilaginous growth.
Finally, in the therapeutic aspect, orthopedic treatment with immobilization corset of a thigh to prevent movement of the lumbosacral junction can be proposed in recent forms.
The reconstruction of the isthmus can be indicated in young athletes and unwilling to reduce physical activity. In the spondylolisthesis phase, conservative treatment by simple immobilization with corset, infiltration and physiotherapy can be indicated. In the event of failure or in the presence of a compressive radiculalgia, decompression and arthrodesis surgery is indicated which in most cases is performed posteriorly. In severe dysplastic forms of the adolescent, with a high potential for aggravation in kyphosis, a double access route (anterior and posterior) may be indicated.
In addition to the postero-lateral fusion in situ, with or without associated decompression, several techniques are currently recommended for the treatment of symptomatic luteal lumbosacral spondylolisthesis of adults [1-4]. All with good results in the different reports; however, the risks of morbidity and mortality in the surgical treatment of these cases, although low, are not negligible and increase as the degree of slippage does [5,6]. Historically, the fusion In situ, even without instrumentation, it has been shown to provide about 80% of satisfactory clinical results even in the presence of pseudoarthrosis, the utility of decompression aggregate being discussed by some, but the utility of pedicle screw instrumentation is widely accepted [7,8]. The clinical results of our series compare favorably with those of the literature. In a recent review article Agabegi and Fischgrund [1] confirm that obtaining a solid fusion leads to better functional and pain reduction results. They also note that circumferential arthrodesis is associated with a higher rate of fusion and became more common, especially in high-grade landslides. This evolution was attributed to the fact that the instrumentation used was not with pedicle screws but simply with sublaminar wiring, as previously described [9].
In addition, comparisons in the literature of in situ fusion with prior supplementation techniques from behind, especially PLIF, are not categorical in terms of improving the results in the medium or long term [10,11]. The same can be said of the pure prior artrodes - ALIF. In a prospective randomized study of patients with instrumented posterolateral fusion divided into those with reduction and others only with sagittal modeling showed that successful arthrodesis and neural decompression are the most important parameters that have an impact on clinical outcome regardless of the degree of listhesis and that the reduction had no statistical translation in the improvement of the clinical outcome [12].
CONCLUSIONS
The in situ instrumented posterolateral decompression and fusion allowed more than 90% of good medium-term results in lumbosacral spondylolisthesis of the adult regardless of grade. Found in literature reports with or without reduction.
- Agabegi SS, Fischgrund JS (2010) Contemporary management of isthmic spondylolisthesis: Pediatric and adult. Spine J 10(6): 530-543.
- Kunze KN, Lilly DT, Khan JM, Louie PK, Ferguson J, et al. (2020) High-Grade Spondylolisthesis in Adults: Current Concepts in Evaluation and Management. Int J Spine Surg 14(3): 327-340.
- Bhalla A, Bono CM. (2019) Isthmic Lumbar Spondylolisthesis. Neurosurg Clin N Am 30(3): 283-290.
- Passias PG, Kozanek M, Wood KB (2012) Surgical treatment of low-grade isthmic spondylolis-thesis with transsacral fibular strut grafts. Neurosurgery 70(3): 758-763.
- Štulík J, Nesnídal P, Kozelnická K, Barna M (2018) Surgical Treatment of High-Grade High-Dysplastic Spondylolistheses in Young Patients - Prospective Monocentric Study of 29 Patients. Acta Chir Orthop Traumatol Cech 85(5): 305-318.
- Ghogawala Z, Dunbar MR, Essa I (2019) Lumbar spondylolisthesis: Modern registries and the development of artificial intelligence. J Neurosurg Spine 30(6): 729-735.
- Dunn B (2019) Lumbar spondylolysis and spondylolisthesis. JAAPA 32(12): 50-51.
- Fedorchuk C, Lightstone DF, McRae C, Kaczor D (2017) Correction of Grade 2 Spondylolisthesis Following a Non-Surgical Structural Spinal Rehabilitation Protocol Using Lumbar Traction: A Case Study and Selective Review of Literature. J Radiol Case Rep 11(5): 13-26.
- Bydon M, Alvi MA, Goyal A (2019) Degenerative Lumbar Spondylolisthesis: Definition, Natural History, Conservative Management, and Surgical Treatment. Neurosurg Clin N Am 30(3): 299-304.
- Tumialán LM (2019) Future Studies and Directions for the Optimization of Outcomes for Lumbar Spondylolisthesis. Neurosurg Clin N Am 30(3): 373-381.
- Tamburrelli FC, Meluzio MC, Burrofato A, Perna A, Proietti L (2018) Minimally invasive surgery procedure in isthmic spondylolisthesis. Eur Spine J 27(Suppl 2): 237-243.
- Kim JS, Kim DH, Lee SH, Park CK, Hwang JH, et al. (2010) Comparison study of the instrumented circumferential fusion with instrumented anterior lumbar interbody fusion as a surgical procedure for adult low-grade isthmic spondylolisthesis. World Neurosurg 73(5):565-571.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Diabetes (ISSN: 2644-3031)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)




