Case Report
Dual Causes of Dysphagia in a Single Person: Achalasia Cardia and Dysphagia Lusoria
5143
Views & Citations4143
Likes & Shares
Achalasia cardia (AC) is characterized by aperistalsis and impaired lower esophageal sphincter (LES) relaxation whereas dysphagia lusoria occurs due to compression of esophagus by aberrant right subclavian artery causing characteristic pencil-like indentation on esophagus in barium esophagogram. We described a case of dysphagia that had both of the above and treated with peroral endoscopic myotomy (POEM) and dietary modification.
Keywords: Esophageal achalasia, Dysphagia lusoria, Peroral endoscopic myotomy
CASE PRESENTATION
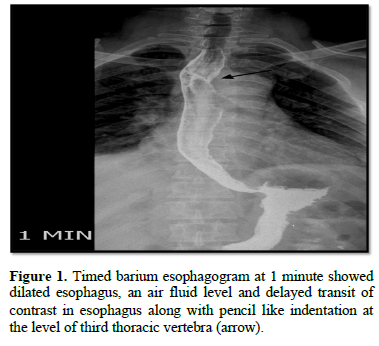
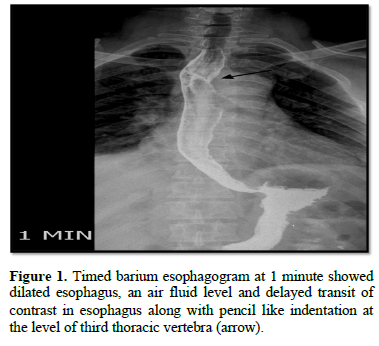
A 47-year-old male from middle east presented with complain of dysphagia to solids and liquids, occasional regurgitation without chest pain and weight loss. Esophago-gastro- duodenoscopy (EGD) showed resistance at LES with dilated esophagus. Timed barium esophagogram showed dilated esophagus, air fluid level and delayed transit of contrast in esophagus along with pencil like indentation at the level of third thoracic vertebra (Figure 1).
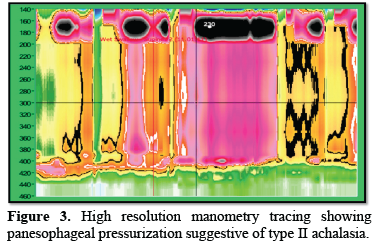
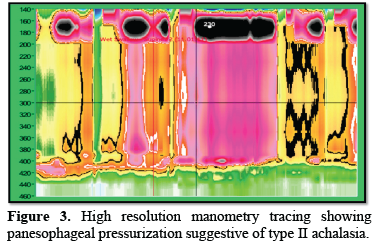
High resolution esophageal manometry (HRM) was consistent with achalasia cardia type II characterized by pan esophageal pressurization. (Figure 2).
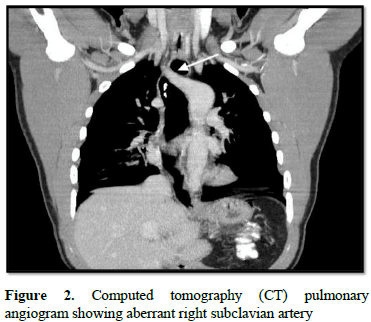
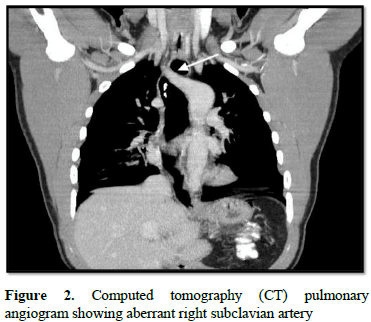
compressing upper esophagus (arrow).
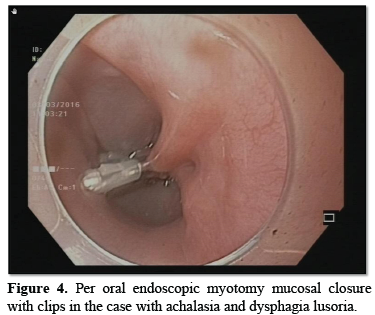
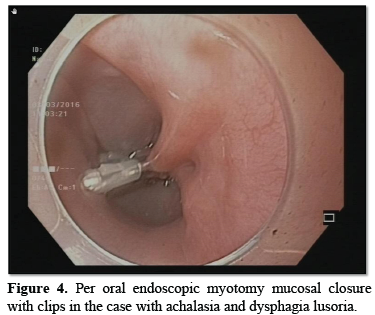
Contrast tomography (CT) angiography showed aberrant right subclavian artery compressing the esophagus confirming dysphagia lusoria (Figure 3). He was treated with POEM for AC (Figure 4).
On follow up he had intermittent episodes of dysphagia which was managed with simple diet modification to soft, small quantity diet. He is asymptomatic on follow up.
DISCUSSION
Achalasia cardia (AC) is the best characterized primary esophageal motility disorder which is characterized by progressive degeneration of ganglion cells in esophageal myenteric plexus. It results in impaired relaxation of lower esophageal sphincter (LES) on swallowing and aperistalsis in distal smooth muscle segment of the esophagus [1]. Based on high resolution manometry (HRM), AC has three main subtypes, namely type I, II and III. AC subtypes based on HRM is important for deciding management strategies [2]. Treatment modalities in AC acts by causing either mechanical disruption of LES: per oral endoscopic myotomy (POEM), Laparoscopic Heeler’s Myotomy (LHM) and pneumatic dilatation (PD) (mainstays of treatment) or Biochemical reduction in LES pressure: pharmacological therapy (e.g. nitrates) and botulinum toxin [3,4]. Dysphagia lusoria is used to describe any vascular anomaly causing extrinsic compression of esophageal lumen which is most common caused by aberrant right subclavian artery (ARSA). Majority of the cases (nearly two third) are asymptomatic. Most of the clinically symptomatic cases present at 45- 50 years of age as non-progressive mechanical dysphagia but can also present in infancy and childhood who can have respiratory symptoms as well [5-7]. Diagnosis is done by barium esophagogram followed by computed tomography (CT) angiogram [8]. Treatment is highly variable based on severity of clinical symptoms and co-existing vascular anomalies. A major proportion of cases respond to dietary modification alone. Some cases respond to proton pump inhibitors and prokinetics mostly due to relief of coexisting gastroesophageal relax disease (GERD) [8]. Rest of the cases may require surgical ligation of aberrant artery and connection to ascending aorta [9]. Hybrid endovascular technique using subclavian carotid transposition (SCT) and embolization of ARSA origin obviate need for thoracotomy as described in a series of two cases [10]. Various techniques of ARSA revascularization and thoracic endovascular aortic repair (TEVAR) are being used as contemporary management of lusoria as described in a recent single center experience of 8 cases [11]. Association of achalasia have been described with other disorders of motility like Hirschsprung’s disease or infantile pyloric stenosis [12]. Moreover, obesity is associated with disorders of esophageal motility like achalasia [13]. However, no cases of co-existent achalasia and dysphagia lusoria have been described in the literature. We describe such as case with dual cause of dysphagia treated with poem and dietary modification. No coexisting vascular anomaly or respiratory symptoms were noted in the present case.
CONCLUSION
In cases of AC having persistent dysphagia after POEM, alternate cause of dysphagia like dysphagia lusoria should be sought. Although dysphagia lusoria rarely causes symptoms, when symptomatic, it can be treated usually by simple dietary modification obviating the need for surgery.
- Reynolds JC, Parkman HP (1989) Achalasia. Gastroenterol Clin North Am 18: 223.
- Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, et al. (2015) International High Resolution Manometry Working Group. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27(2): 160-74.3.
- Gulati S, Emmanuel A, Inoue H, Hayee B, Haji A (2017) Peroral endoscopic myotomy: a literature review and the first UK case series. Clin Med (Lond) 17(1): 22-28.
- Spiess AE, Kahrilas PJ (1998) Treating achalasia: from whalebone to laparoscope. JAMA 280(7): 638-642.
- Levitt B, Richter JE (2007) Dysphagia lusoria: a comprehensive review. Dis Esophagus 20: 455-460.
- Jan SL, Lin MC, Chan SC (2018) Mid-term follow-up study of neonatal isolated && aberrant right subclavian artery. Cardiol Young 28: 1024-1030.
- Epperson MV, Howell R (2019) Dysphagia lusoria: problem or incidentaloma? Curr Opin Otolaryngol Head Neck Surg 27(6): 448-452.
- Anssen M, Baggen MG, Veen HF, Smout AJ, Bekkers JA, et al. (2000) Dysphagia lusoria: clinical aspects, manometric findings, diagnosis, and therapy. Am J Gastroenterol 95(6): 1411-1416.
- Thompson JL, Burkhart HM (2016) Translocation of an aberrant right subclavian artery with resolution of dysphagia lusoria. Ann Thorac Surg 102: e65-e67.
- Dueppers P, Floros N, Schelzig H, Wagenhäuser M, Duran M (2021) Contemporary Surgical Management of Aberrant Right Subclavian Arteries (Arteria Lusoria). Ann Vasc Surg 72: 356-364.
- Sigdel A, Wayne EJ, Dwivedi AJ (2020) Hybrid Endovascular Treatment of Dysphagia Lusoria: Report of 2 Cases. Vasc Endovascular Surg 54(8): 747-751.
- Mayberry JF, Atkinson M (1986) Achalasia and other diseases associated with disorders of gastrointestinal motility. Hepatogastroenterology 33(5): 206-207.
- Zheng E, Gideon RM, Sloan J, Katz PO (2017) Esophagogastric junction outflow obstruction is often associated with coexistent abnormal esophageal body motility and abnormal bolus transit. Dis Esophagus 30(10): 1-4.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Pathology and Toxicology Research
- Journal of Rheumatology Research (ISSN:2641-6999)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)






