Research Article
Healthcare of Patients with Inflammatory Bowel Disease During the COVID-19 Pandemic
1301
Views & Citations301
Likes & Shares
With the pandemic of the new coronavirus, IBD specialists were challenged to address specific questions of their patients, particularly regarding the risk of infection and immunosuppressive treatment. Despite the predominance of flu-like symptoms, the emergence of gastrointestinal manifestations was observed, and information on the characteristics of the infection in inflammatory bowel disease is of special interest.
Objective: To carry out a research on the epidemiological characteristics of patients with IBD in Minas Gerais, to characterize the behavior towards COVID-19, preventive measures, management of IBD and emotional states during the pandemic.
Results: 111 people were interviewed, 80% of them women, most of them married. The sample had a mean age of 37 years and almost eight years of diagnosis of inflammatory bowel disease (mostly Crohn's Disease). A high rate of anxiety and stress was identified, which worsened after the onset of the pandemic and its consequences, such as social isolation, care with hygiene, dietary changes and in the level of physical activity, in addition to the lack of medication and the postponement of appointments and exams.
INTRODUCTION
In late 2019, an acute respiratory syndrome caused by the SARS-CoV-2 coronavirus, later called COVID-19, began in China. The COVID-19 pandemic emerged as a public health emergency and challenged health systems around the world. It has spread rapidly throughout the world, regardless of borders, manifesting itself as an acute respiratory disease that varies widely in severity, from asymptomatic carriers to mild and non-specific symptoms to severe pneumonia, sepsis and death [1]. Currently, with numbers exceeding 176 million confirmed cases and almost four million deaths, the pandemic is showing a devastating effect [2]. This effect is due to the high contagiousness of COVID-19 and, although mild forms predominate, severe cases and mortality in absolute values are very high [3]. Despite the predominance of flu-like symptoms, gastrointestinal manifestations such as loss of appetite, diarrhea, vomiting and abdominal pain were observed4. The emergence of these gastrointestinal findings has raised serious concerns about the management of patients with a history of digestive problems. This has led to the implementation of gastrointestinal care recommendations by the Chinese IBD Society, China Crohn's & Colitis Foundation, Crohn's Colitis of Foundation America and Crohn's & Colitis UK [4]. In addition, information about the characteristics of the infection in inflammatory bowel disease is of special interest, due to the fact that these patients receive greater care at health centers, which can increase the risk of contagion [3]. IBD is a recurrent and remitting inflammatory bowel condition. A significant proportion of these patients are treated with long-term immunomodulatory/immunosuppressive therapy, which potentially puts them at increased risk for infections and associated complications [1]. As the COVID-19 outbreak is rapidly evolving, IBD specialists around the world have been challenged to face the pandemic and address the specific issues of their patients, particularly regarding the risk of infection and immunosuppressive treatment. The current study aimed to research the epidemiological characteristics of patients with IBD in Minas Gerais, characterize the behavior towards COVID-19, prevention measures, IBD management and emotional states during the pandemic.
METHODS
Design
This is a descriptive, cross-sectional survey, carried out through a questionnaire. Participants Patients with inflammatory bowel diseases, residents of the state of Minas Gerais, over 16 years old. Exclusion criteria: hospitalized or institutionalized people.
Data collect
The objectives of the study were disclosed on social networks related to inflammatory bowel diseases, containing the researchers' email addresses and telephone numbers. The patient interested in participating contacted us by email and filled out an online questionnaire. Data collection questionnaire was created by the researchers using Google Forms. It consists of open and multiple-choice questions, totaling 34 questions. The average expected time to respond is 10 min.
RESULTS AND DISCUSSION
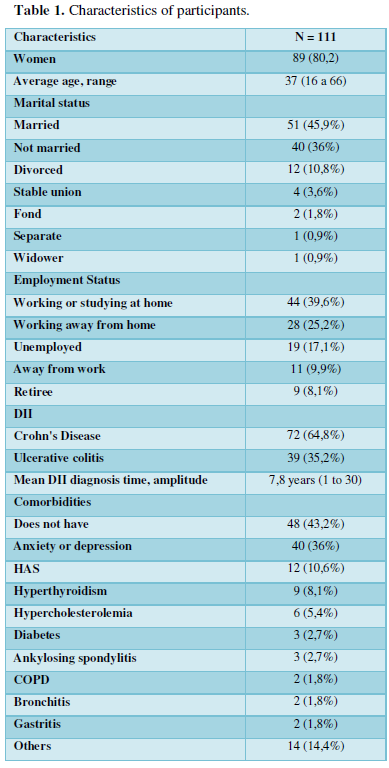
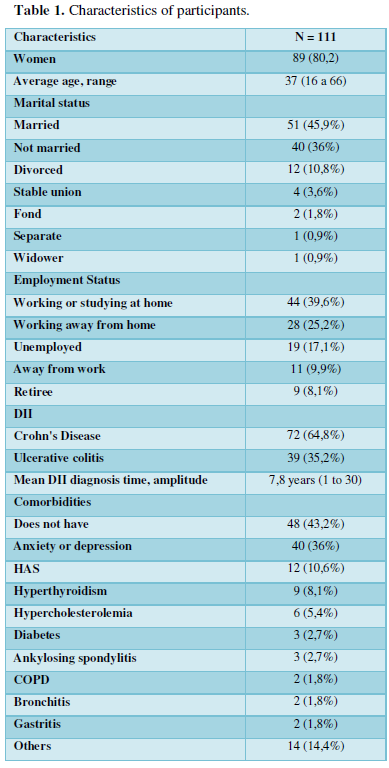
From January to April 2021, 111 people from 26 cities in Brazil completed the questionnaire. The majority (80.2%) are female, with a mean age of 37 years (ranging between 16 and 66). According to epidemiological studies, IBDs preferentially affect young people, being the most susceptible age group from ten to forty years old [5]. There is no gender predominance, but a possible association with specific ethnic groups. IBDs affect both men and women in similar proportions, with CD being more prevalent in women [6]. However, in different surveys, there is greater participation of the female audience [7]. The other characteristics of the sample are represented in the Table 1 below.
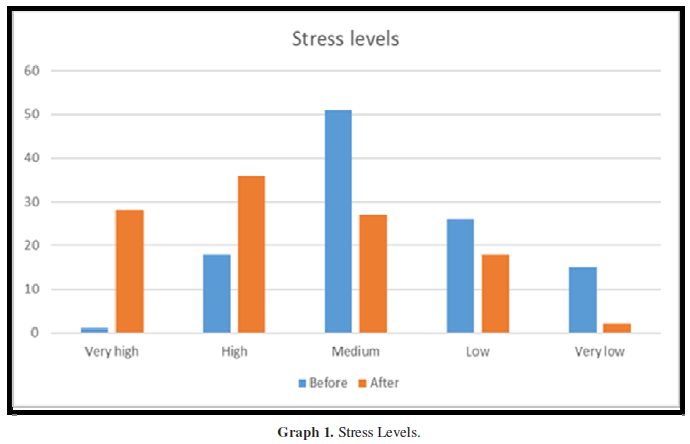
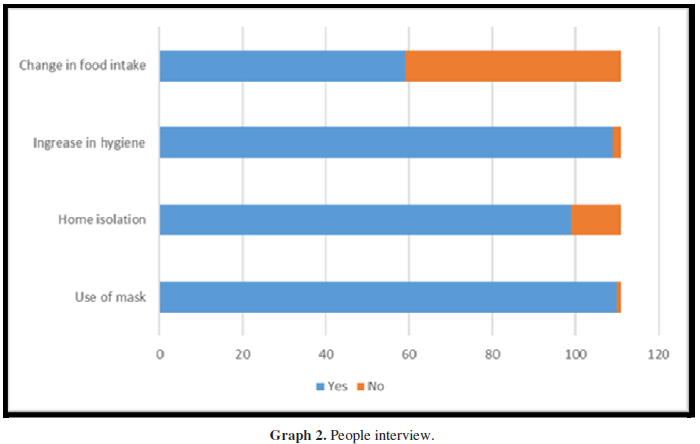
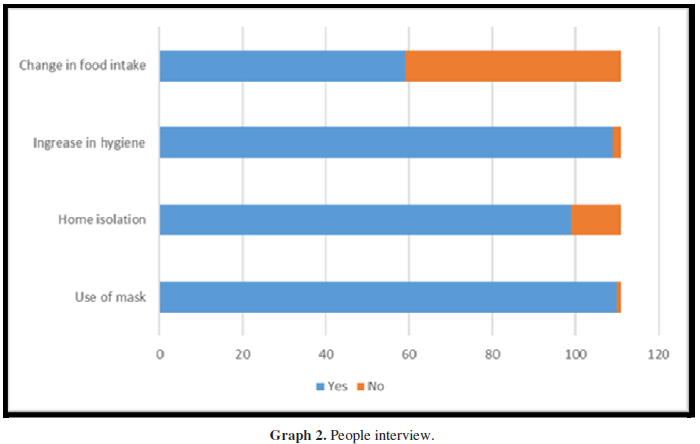
Regarding comorbidities, the high rate of hypertensive patients surpassed that mentioned in other studies [8]. However, the cardiovascular risk is higher in patients with inflammatory bowel disease. Some authors associate this with the increase in inflammatory cytokines [9] and others [10] to prescription drugs. The control of medications is of paramount importance, due to the patient's strong exposure to the risk of developing arterial hypertension, diabetes, osteoporosis and other associated pathologies. Regarding the medication prescribed for IBD, 88 (79.3%) reported that there was no change during the pandemic. In the study by Podolsky [10] with regard to the characteristics of drug treatment specifically prescribed for chronic digestive disease, there was a predominance of the use of only one drug: amino salicylates (sulfasalazine and mesalazine). Another issue raised was the difficulty in acquiring these medications, stated by 21.6% (24) of the interviewees. The most cited reasons were the lack of medication at the pharmacies (scored by 12 people) and the long lines at the pharmacies (5 people). Some people also complained about the high value of the medication. Due to such problems, nine patients ended up without any medication(s) during this period. A cross-sectional study [11] included 110 patients, of whom 72.6% had the medication provided by the SUS. The interview identified 15 (13.7%) patients with a low degree of adherence to treatment. In patients with chronic digestive diseases, low adherence to drug treatment is frequent, with a predominance of unintentional behavior of low adherence (carelessness or forgetfulness) [11]. The low level of adherence behavior seems to be independent of individual characteristics, the nature of the disease (diagnosis) or the free provision of medication, and it may be a common trait among service users. Adding this characteristic to the circulation difficulties of the pandemic, the degree of adherence becomes even worse. This shows the need for educational measures to increase adherence to treatment, which implies greater attention from health professionals to the use of medications by patients. Almost half of the interviewees (44.1%) failed to attend any appointment or test during the pandemic and the most cited reasons were: “appointment unmarked by the doctor” and “I unmarked for fear of contaminating myself”. Only one respondent reported having forgotten the appointment and another was hospitalized. In this matter, some patients claimed to have gone through remote consultations, which is justified by the orientation of social restriction and authorization of the Medical Councils for the teleconsultation. The rate of social restriction of interviewed patients was above 85%, higher than the general average for Brazilians of 75% [12]. About dietary changes, more hygiene care, compliance with home isolation and use of masks, the answers are represented in the Graph 1 and Graph 2 below.
Its immunopathogenesis includes genetic factors (mutations linked to poor regulation of the intestinal immune system), intestinal microbiota and environmental factors [13]. IBD is characterized by a chronic inflammatory state of the intestinal mucosa and, as such, the vast majority of patients may present with iron deficiency anemia. The consumption of iron-rich foods, especially iron of animal origin, should be encouraged in patients with IBD. Unfortunately, the vast majority of patients, especially those with disease activity, experience exacerbation of gastrointestinal symptoms when they increase the consumption of iron-rich foods, both animal and vegetable. Conversely, the consumption of vitamin C associated with iron increases its absorption by the intestine. Currently, the increase in vegetarian or vegan individuals makes it even more difficult to correct dietary iron deficiency in patients with IBD [13]. Of the participants, 13 had Covid and, of these, two needed hospitalizations. The symptoms mentioned by those who tested positive were: headache, diarrhea, body pain, fever, cough, runny nose, loss of taste, anosmia, dyspnea and nausea. A minority of patients (11.7%) had Covid, however, most (76; 68.5%) know a family member, friend or neighbor who had the disease. In a survey conducted in January 2020,14, 28.1% of patients with IBD reported having had some flu symptom, but only 5.9% had tested for COVID-19. In patients with chronic disease, and especially in those who use medication, the risk of opportunistic infections is higher [13]. This risk is not exclusive to this therapeutic class, and may occur in patients using other immunomodulating drugs such as corticosteroids, azathioprine, methotrexate and cyclosporine, which are part of the therapeutic arsenal of IBDs. Among the opportunistic infections in patients using immunosuppressants, viral infections stand out. With the emergence of new endemic viral diseases, there is a real concern with patients using biological therapy when acquiring these diseases. Dengue, Chikungunya, Zika and COVID-19 have caused epidemics of large proportions in Brazil in recent years, with the emergence of complications and severe forms of the disease. Understanding the behavior and impact of this disease on biological therapy users is an urgent need in a national scenario of triple epidemic [14]. The high infectivity of SARS-CoV-2, in the absence of previous immunity in the human population, makes non-pharmacological interventions indicated, aiming to inhibit transmission between humans, slow down the spread of the disease, and consequently reduce and delay the peak of occurrence in the epidemic curve16. Individual measures include hand washing, respiratory etiquette and social distance. Social distancing, in turn, encompasses the isolation of cases, the quarantine applied to contacts, and the voluntary practice of not going to places with agglomerations of people [17]. Another individual measure is the use of masks, recommended for individuals with confirmed or suspected coronavirus infection, and their caregivers. Measures of social restriction impacted the routine of many people, including the practice of physical activity. In this research sample, during the pandemic, 45 patients reported that they did not change their habits (32 remained sedentary and 13 remained active). The other 66 changed, and 33 stopped the activity, 13 kept it, but in a reduced way, and 20 patients started the practice of some physical exercise. It is estimated that 30% to 60% of people with Crohn's disease or ulcerative colitis have below average bone density [16]. This happens because the symptoms and treatment of inflammatory bowel diseases cause changes in the body mass index (BMI), which triggers a reduction in bone mineral density - osteoporosis - and in muscle mass, which negatively influences the quality of life of those who presents the disease [17]. Physical exercise plays an important role in the quality of life of patients with inflammatory bowel diseases and can be considered one of the complementary treatments. In addition to being beneficial for the treatment and prevention of osteoporosis, low- and moderate-intensity physical exercise promotes an improvement in quality of life and helps the gastrointestinal tract, which are associated with the prevention of colon cancer, inflammatory bowel diseases, diverticular disease, reduction of constipation, cholelithiasis and gastrointestinal bleeding [17]. 20 to 60 minutes of aerobic exercise are recommended, 2 to 5 days a week, and strength training, at least twice a week, as a complement, in order to minimize or reverse muscle loss and improve bone mineral density [17].
Anxiety and stress levels before and during the pandemic were investigated and the data are shown in the Graphs 3 and 4 below.
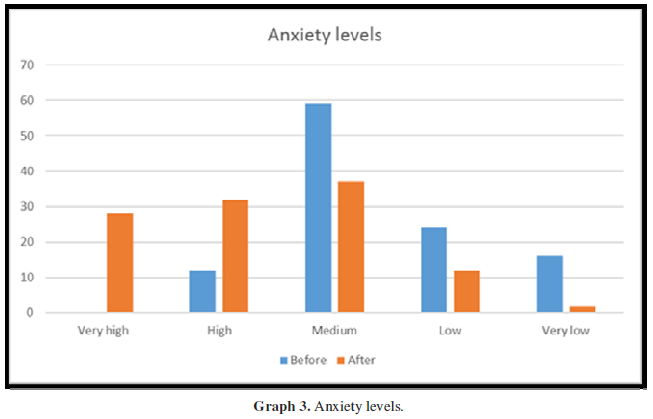
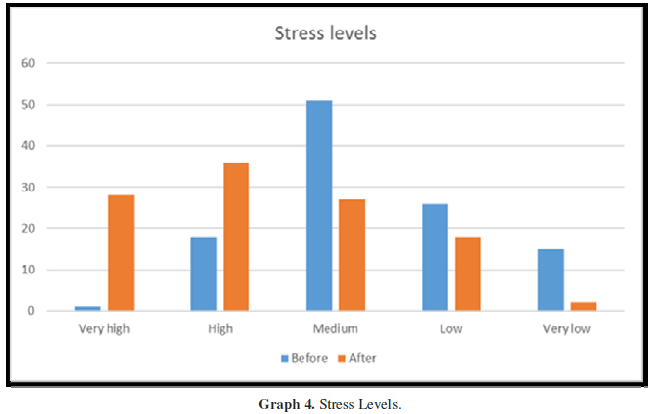
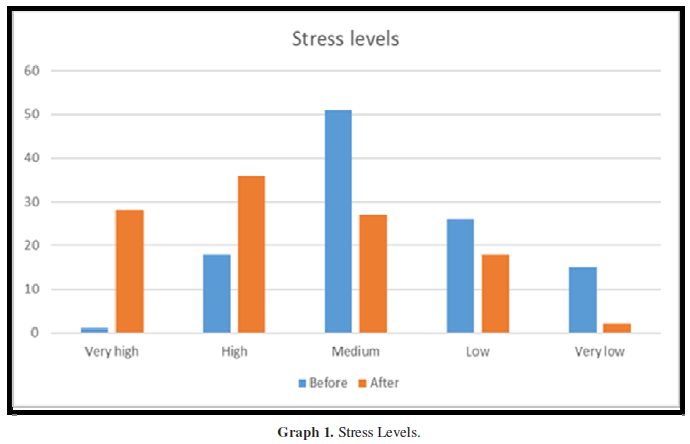
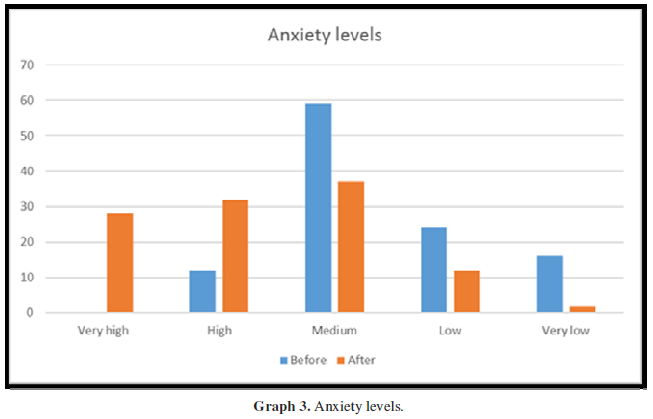
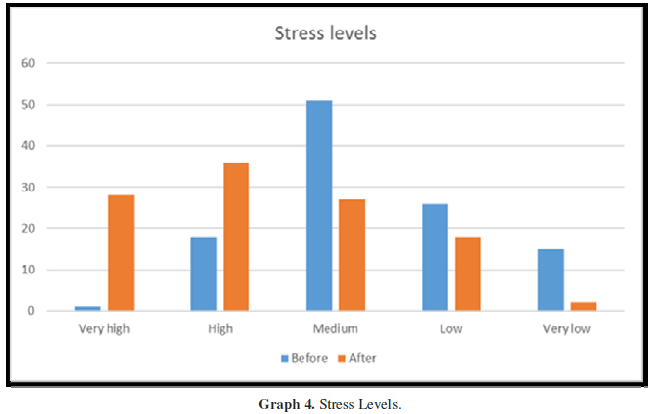
Like any other chronic illness, IBDs cause a degree of pain, dietary limitation and psychological stress. Thus, greater are the risks in the quality of life of patients with a chronic disease, which starts to add changes in their lifestyle, representing for them an uncertain future, a barrier, a challenge, loss of physical capacity, beauty and activities social [18]. Thus, it becomes necessary to identify psychological problems in patients with IBD, so that a better treatment project can be followed, and above all, better well-being for these individuals. The QoL, usually negatively affected in these patients, can have repercussions on their personal and professional relationships, with the need for greater psychological support and treatment for anxiety and depression [19]. Non-Infectious Chronic Diseases (NCDs) play an important role in the current health profile of human populations and the discussion on this topic has been gaining more space in the sense of being able to maintain the integrity, independence and autonomy of affected individuals. Estimates from the World Health Organization (WHO) indicate that NCDs are already responsible for 58.5% of all deaths in the world and for 45.9% of the global disease burden [20]. The health system is focused on acute illness rather than chronic illness, which culminates in uninformed and unprepared patients to perform self-care. Visit planning is brief and there are no certainty that acute and chronic needs will be efficiently met [21]. The pandemic evidences a series of mental health problems that in the past would have been postponed and ignored, but in the absence of recreational activities, they end up increasing. In IBD patients, the situation can become even more complicated, as the obstacles encountered in accessing appointments and medications contribute to higher levels of anxiety caused by economic issues, loneliness, insecurity and the growing fear of being infected. In the research by Almeida and Silva [22] 14, 55.1% of Brazilians reported a decrease in family income, and 7% had no income; 25.8% of individuals did not work, with the group of informal workers being the most affected (50.6%). Even after more than 1 year of diagnosis, 35 people interviewed (31.5%) stated that they did not know any association of IBD patients. Of the 76 who know, 48 participate in some of them and cited AMDII, ATRIMDII, ABCD, DII BRASIL, ALEMDII, ADIIZOM. Group meetings are extremely important25, as they can support people to better understand their living and health conditions and to carry out self-care actions; motivate and implement desirable behavior changes; facilitate communication between professionals and users; promote access to resources and actions of health services; equate the needs of changing lifestyle habits and ways to better deal with the illness; share experiences in handling everyday situations related to chronic conditions and clarify doubts and curiosities. Group work also makes it possible to help participants to elaborate their affective experiences, feelings and coexistence with their health conditions, recognizing and/or expanding their own potential; agree commitments to improve the health situation; seek greater adherence to treatment; strengthen the participants' self-esteem; expand the responsibility of each participant regarding their own treatment, encouraging their independence and autonomy in decision-making; create integration in the community; favor the creation of care networks; build treatment goals in a participatory way; complement and qualify the assistance activities [23]. Finally, a blank question was left for respondents to express themselves freely. The answers were read and categorized by themes mentioned, the most frequent being “importance of research to improve treatments and quality of life” and “importance of awareness and union of people in the face of the pandemic”. All respondents praised the initiative and thanked the opportunity to participate and contribute.
CONCLUSION
This research sought to identify the changes in healthcare for patients with IBD that occurred during the COVID-19 pandemic. Increasingly common in our society, chronic diseases are more present in health services, requiring increased attention from their professionals. This permanent life experience causes stress due to changes in body image, the need for social and psychological adaptation, in addition to changes in life expectancy. During the pandemic, patients experienced changes in their work routine, social relationships, diet, levels of physical activity, hygiene care, consultations and access to medication. Stress and anxiety levels increased and there was a drop in QoL. The QoL of people with IBD reported in research is considered low, however, in most studies, it was not found which sociodemographic aspects influence the most. Identifying these factors is important, as they can support guidelines for the care of people with IBD. However, the scarcity of literature addressing this issue was noted, especially in studies carried out in Brazil.
- Aysha A, Rentsch C, Prentice R, Johnson D, Bryant RV, et al. (2020) Practical management of inflammatory bowel disease patients during the COVID‐19 pandemic: Expert commentary from the Gastroenterological Society of Australia Inflammatory Bowel Disease faculty. Intern Med J 50(7): 798-804.
- Organização Panamericana da Saúde (OPAS) (2020) Folha informative - COVID-19 (doença causada pelo novo coronavirus) Available online at: https://www.paho.org/pt/brasil
- Marin JI, Zabana Y, Rodriguez LI, Marin L, Esteve M, et al. (2020) COVID-19 and inflammatory bowel disease: questions arising from patient care and follow-up during the initial phase of the pandemic. Gastroenterol Hepatol 43(7): 408-413.
- Tian W, Huang Y, Dai C (2020) The Effect of the COVID-19 Pandemic on the Medical Mode of Patients with Inflammatory Bowel Disease in China. Inflamm Bowel Dis 26(10): e116-e117.
- Pearson C (2004) Inflammatory bowel disease. Clinical Advanced NT 100(9): 86-90.
- Steidler L, Hans W, Schotte L, Neirynck S, Obermeier F, et al. (2000) Treatment of murine colitis by Lactococcus lactis secreting interleukin-10. Science 289(5483): 1352-1355.
- Gasparini RG (2018) Incidence and Prevalence of Inflammatory Bowel Diseases in the State of São Paulo - Brazil. Thesis presented to the Faculty of Medicine, Paulista State University "Júlio de Mesquita Filho", Botucatu Campus, to obtain the title of Doctor in General Bases of Surgery.
- Lopes AM, Moura LNB, Machado RS, Silva GRF (2007) Quality of life of patients with Crohn´s disease. Enfermería Global 47: 353-368.
- Goncalves PD, Nunes CP (2019) The cardiovascular risk in patients with inflammatory bowel disease. Revista de Medicina de Família e Saúde Mental 1(1).
- Podolsky DK (2002) Inflammatory bowel disease. N Engl J Med 6(12): 417-429.
- Dewulf NLS, Monteiro RA, Passos ADC, Vieira EM, Troncon LEA (2006) Compliance to drug therapy in university hospital outpatients with chronic digestive diseases. Arq Gastroenterol 44(4): 289-296.
- Almeida WS, Szwarcwald CL, Malta DC, Barros MBA, Lima MG, et al. (2020) Mudanças nas condições socioeconômicas e de saúde dos brasileiros durante a pandemia de COVID-19. Rev Bras Epidemiol 23: 1-14.
- Zaltman C, Chebli JMF, Teixeira MG, Albuquerque IC, Souza HSP (2018) As Doenças Inflamatórias Intestinais na Atualidade Brasileira. Available online at: https://gediib.org.br/wp-content/uploads/2019/07/Livro_As-Doencas-Inflamatorias-Intestinais-na-Atualidade-Brasileria-GEDIIB-2018.pdf
- Anderson RM, Heesterbeek H, Hollingsworth TD (2020) How will country-based mitigation measures influence the course of the Covid-19 epidemic? Lancet 395(10228): 931-934.
- Qualls N, Levitt A, Kanade N, Wright JN, Dopson S, et al. (2017) Community mitigation guidelines to prevent pandemic influenza - United States, 2017. MMWR Recomm Rep 66(1): 1-32.
- Association Brazilian of Ulcerative Colitis and Crohn's Disease (ABCD) (2018) Bone loss may get higher due to IDI. Rev. of the Brazilian Association of Ulcerative Colitis and Crohn's Disease. 66: 8-11. Available online at: https://www.abcd.org.br/blog/noticias/perda-ossea-pode-ficar-maior-devido-a-dii/
- Briza W, Navarro A, Sanches L, Bastos K (2010) The benefits of physical exercise in patients with inflammatory bowel diseases. Rev Braz Sports Nutrition 4(20).
- Leite, VM, Lopes CM, Vilela MGA, Cardoso MG, Carvalho SO et al. (2020) Impacto dos aspectos psicológicos em portadores de doença inflamatória intestinal. Braz. J. Hea. Rev., Curitiba 3(2): 1363-1367.
- Estima, B (2018) Life quality of patients with inflammatory bowel disease: integrative review. J. Enterostomal Ther., São Paulo 16: e2118.
- Malta DC, Bernal RTI, Lima MG, Araújo SSC, Silva MMA, et al. (2017) Doenças crônicas não transmissíveis e a utilização de serviços de saúde: análise da Pesquisa Nacional de Saúde no Brasil. Rev Saude Publica 51(Supl 1:4s.).
- Silva RM, Jorge MSB, Silva AG (2015) Planning, management and evaluation in health practices [e-book] − Fortaleza: EdUECE.
- Rosa JR, Silva JF, Rosa MI (2014) Epidemiological profile of patients with inflammatory bowel disease. Arq Catarin Med 43(2): 53-58.
- Ministry of Health (2014) Department of Health Care. Department of Primary Care. Strategies for the care of people with chronic disease.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Rheumatology Research (ISSN:2641-6999)





