Research Article
Psychological Impact Among Patient Admitted with Coronavirus Disease (COVID-19) in A Tertiary Care Hospital in Southern Pakistan
1044
Views & Citations44
Likes & Shares
Introduction: On 11th February 2020, WHO named the novel coronavirus as Coronavirus Disease 2019 (COVID-19). The current uncertainty of the prevailing situation of COVID-19 pandemic due to its clinical presentation, infectious cause and underprepared health facilities to address the coronavirus contagion have considerably high potential of psychological impact, more so in developing countries like Pakistan.
Methods: This was an observational study done on the patients admitted in the COVID Isolation wards of Ruth K.M Pfau Civil Hospital, Karachi. It was a self-reported questionnaire administered in Urdu with aid provided as needed. The questionnaire used the DASS-21 scale. SPSS version 22.0 was used to analyze the results. Chi-square test and independent sample T test were then applied with P-value
Results: The study was completed by 201 patients. There were 108 (53.7%) male patients and 93 (46.3%) female patients. DASS-21 scores were categorized according to gender, employment status, financial dependence and family structure. It indicated that depression (p=0.012) and stress (p=0.03) were statistically significant for gender. Depression was significantly related to unemployment (p<0.0001), financial dependence (p<0.0001), and living with nuclear family (p=0.007).
Conclusion: In light of the pandemic, it is evident that the COVID-19 cases are only going to rise and with it so will the incidence of mental health problems. Therefore, it is paramount that medical facilities catering those patients take into account the psychological distress that accompanies the virus and takes necessary steps to manage it. Further, a multidisciplinary approach should be adopted towards dealing with the COVID-19 pandemic.
Keywords: COVID-19, Psychological Impact, Mental Health, Multidisciplinary, Stress, Anxiety, Depression
INTRODUCTION
World Health Organization (WHO) on January 30th 2020, announced the occurrence of novel coronavirus and declared a Public Health Emergency of International Concern (PHEIC). This is the sixth PHEIC under International Health Regulations (IHR) after H1N1 Influenza in 2009, Polio in 2014, Ebola in West Africa in 2014, Zika in 2016, Zika in Democratic Republic of the Congo (DRC) in 2019. On 11th February 2020, WHO named the novel coronavirus as Corona Virus Disease 2019 (COVID-19). The current uncertainty and unpredictability of the prevailing situation of COVID-19 pandemic due to its clinical presentation, infectious cause, epidemiological features, fast transmission both direct and local, seriousness of public health impact in our setup, novelty, scale, implications for international public health and underprepared health facilities to address the coronavirus contagion have considerably high potential of psychological impact [1]. Such, psychological impacts may include fear, anxiety, stigma, marginalization towards the disease and subsequent depression. Not only have these psychological impacts been studied among the positive patients in the global literature but also among their families, their healthcare providers, and the general population living in quarantine. In pandemics, like COVID-19, people in the developed countries have been studied to be more resilient to stress and survive stressful events psychologically unharmed [2]. However, in developing countries, like our own, the fear of pandemic can be felt strongly due to lack of emotional support systems. Hence, the psychological footprint is expected to be larger than the medical footprint [3]. With the advent of novel coronavirus, an unchartered territory in Pakistan on 26th February 2020, the state is on high alert and has implemented partial lockdown. As of 25th April 2020, Pakistan coronavirus tally has risen to 11,940. The worst hit countries like China, United States, Italy, Spain, Iran, France, United Kingdom and Germany are intensifying their efforts to manage the pandemic via collective public health intervention measures [4]. Being a developing nation with a struggling healthcare system and high ratios of poverty and illiteracy; coronavirus also has a huge psychological impact especially on positive patients and their families. Experts have advised people to stay in self-isolation but the necessary restrictions would have short and potentially long-term detrimental impact on mental health. Pakistan being a collectivistic culture highly dependent on socialization (social support and social connectedness) has been critical towards self-isolation, social-distancing and quarantine and are reluctantly dealing with emotional, psychological, behavioral and social impacts of this crisis. In this context, psychiatrists and mental health workers can play pivotal role in supporting the well-being of those affected and their families, the at-risk healthcare staff as well as the public. They are in fact in a unique position to offer a balanced perspective to improve the knowledge, attitude and practices about the illness as well as addressing the generalized anxiety and apprehension. Similar roles have been shown to improve the overall health-care service utilization and efficacy in similar earlier outbreaks like SARS (Severe Acute Respiratory Syndrome) [5]. This study assesses the proportion of COVID patients suffering from concomitant psychological comorbidities including depression, anxiety and stress. This would help to plan adequate psychological interventions to be implemented for a multidisciplinary approach to improve the morbidity, mortality, and psychological status of those affected.
MATERIALS AND METHODS
An observational study was conducted in COVID-19 isolation wards at Dr. Ruth K. M. Pfau Civil Hospital Karachi from 1st June till 31st August 2020. Consecutive non-probability sampling technique was adapted and all patients of age 18 years and above diagnosed as COVID-19 positive by Real Time Polymerase Chain Reaction testing panel for SARS-COV-2, admitted in isolation ward with moderate COVID-19 (symptomatic patients requiring ward admission but not severe enough to indicate ICU admission) were included. Patients with altered level of consciousness / loss of consciousness / on ventilator support / acutely psychotic / or who could not comprehend the interviewer due to any reason were excluded. A semi-structured questionnaire was constructed which included demographic characteristics of the patient and Depression, Anxiety and Stress Scale - 21 Items (DASS-21) [6]. DASS-21 is a set of three self-report scales designed to measure the emotional states of depression, anxiety and stress. Each of the three DASS-21 scales contains 7 items, divided into subscales with similar content. The depression scale assesses dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest / involvement, anhedonia and inertia. The anxiety scale assesses autonomic arousal, skeletal muscle effects, situational anxiety, and subjective experience of anxious affect. The stress scale is sensitive to levels of chronic nonspecific arousal. It assesses difficulty relaxing, nervous arousal, and being easily upset / agitated, irritable / over-reactive and impatient. Scores for depression, anxiety and stress are calculated by summing the scores for the relevant items. The DASS-21 is based on a dimensional rather than a categorical conception of psychological disorder [6]. For the purpose of this study, Urdu version of DASS-21 was utilized. It has been translated and validated by Husain et al. [7]. Data was entered and analyzed through SPSS version 22.0. Mean and standard deviation was calculated for quantitative variables. Frequency and percentage were calculated for qualitative variables like gender. Internal consistency was calculated for DASS-21. Effect modifiers such as age and gender were stratified to see their effect on outcome variables. Chi-square test was applied after stratification for comparison of categorical variables. Independent sample T test was applied for comparison of means. P-value
RESULTS
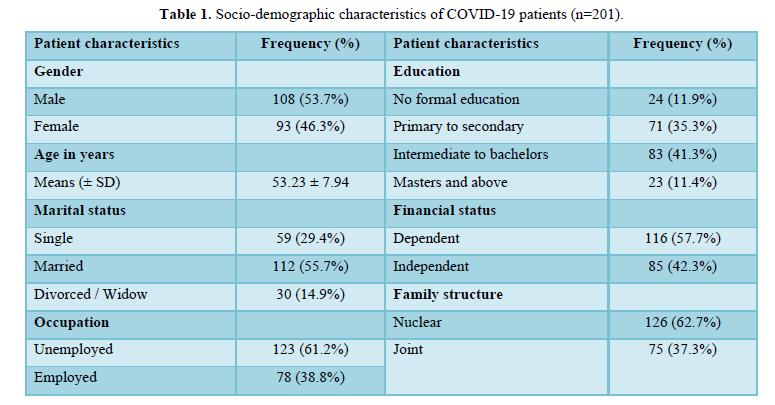
The study was completed by n= 201 patients. There was n=108 (53.7%) male patients and n=93 (46.3%) female patients. Their mean age was 53.23 ± 7.94 years. Most of the sample was married (n=112; 55.7%), unemployed (n=123; 61.2%), educated from intermediate to bachelors (n= 83; 41.3%), financially dependent 116; 57.7%), and living in nuclear family (n=126; 62.7%). All characteristics are summarized in Table 1.
Depression, anxiety, and stress were assessed using DASS-21. There were 70 (34.8%) non-depressed patients, 35 (17.4%) non-anxious patients, and 25 (12.4%) non-stressed patients. One hundred and fourteen (56.7%) patients were mild to moderately depressed; 138 (68.6%) were mild to moderately anxious; and 133 (66.2%) were mild to moderately stressed. Seventeen (8.5%) patients were severe to extremely severely depressed, 28 (13.9%) were severe to extremely severely anxious, 43 (21.4%) were severe to extremely severely stressed.
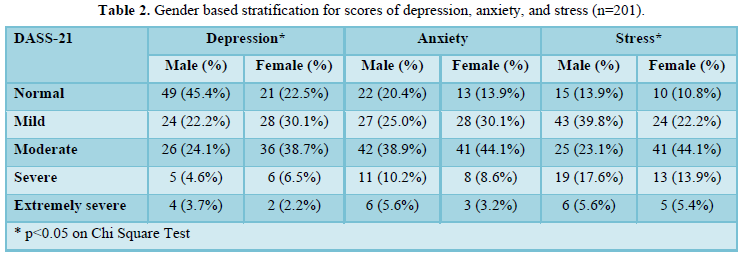
DASS-21 scores were categorized according to gender as shown in table 2. It indicated that depression (p=0.012) and stress (p=0.03) were statistically significant for gender. Most women (n=36; 38.7%) were moderately depressed and most men (n=49; 45.4%) were non-depressed; most men (n=43; 39.8%) were mildly stressed and most women (n=41; 44.1%) were moderately depressed (Table 2).
Scores of depression, anxiety, and stress on DASS-21 were then correlated with employment status, financial dependence, and family structure as shown in table 3. Depression was significantly related to unemployment (p<0.0001), financial dependence (p<0.0001), and living with nuclear family (p=0.007). Stress was significantly related to unemployment (p=0.04) and living with nuclear family (p=0.025) (Table 3).
DISCUSSION
This study assessed the psychological impact on COVID-19 positive patients admitted in a tertiary care hospital. This study showed high depression, anxiety, and stress in hospitalized COVID-19 patients. The available literature demonstrates that there has been a rise in mental health disorders such as anxiety, depression, panic disorder, among other in the general population ever since COVID-19 outbreak mainly due to the general fear and uncertainty associated with the disease [8]. Moreover, studies have also shown that individuals who contracted COVID-19 reported higher levels of anxiety, depression and other psychological symptoms compared to those who weren’t infected [9,10]. The reasons for this could be the prolonged isolation from family and friends, misinformation surrounding the disease, lack of clarity regarding the outcome as well as incessant worry of transmitting the virus to said friends and family prior to hospital admission [11,12]. In our study, we also found that women were more likely to have symptoms of anxiety and depression as is concurrent with other studies [13]. A study by Wang et.al claimed that women were three times more likely to develop an anxiety disorder compared to men in the COVID-19 pandemic [14]. This can be attributed to the fact that women are usually overburdened with numerous responsibilities and are more prone to


developing mental health disorders [15]. A study by Soni [17] also discovered that fluctuations in ovarian hormone levels are responsible for altered sensitivity to emotional stimuli during certain phases in the menstrual-cycle thus forming the basis of a specific vulnerability to psychological disorders in women [17]. Another finding was that the participants who were unemployed and/or financially dependent experienced far greater symptoms of anxiety and depression as compared to those who were employed and/or financially independent. A recent review in Lancet Psychiatry had similar findings whereby showing that populations with social inequality are more susceptible towards mental health problems [18]. This is not a surprising finding considering the exorbitant expenses of COVID-19 patients. In addition, the imposition of the lockdown and the hit that the world economy took in light of COVID-19 pandemic reduced the chances of finding another job thereby further adding to the psychological burden [19]. Furthermore, as Pakistan is a developing country, most people survive on daily wages and are therefore least likely to have sufficient savings. In light of the findings of this study, it is essential for hospitals to create a treatment plan that caters to the mental well-being of COVID-19 patients in adjunct to their physical well-being. It is recommended to maintain an exercise regimen for COVID-19 patients according to their level of fitness and mobility [20] and focus on a healthy lifestyle that ensures nutritious meals to strengthen their immunity and allow for speedy recovery. Furthermore, use of helplines and tele-health to provide psychological support to those diagnosed with COVID-19. Additionally, since women are majorly affected by the pandemic, interventions should target them more. The government should also work towards creating a package that would allow for some financial support for those families that have recently lost their employment due to the losses of the pandemic such as the Ehsaas programme. In addition, free meals being provided by NGOs such as Edhi, Chippa, etc. are also a great way of providing support to the worst hit during the pandemic. As per our knowledge, this study is the first of its kind to be conducted in Karachi, Sindh, Pakistan. However, like all studies, ours too has its limitations. The first one being that our sample size was small. Its cross-sectional design did not allow us to construct any causal relationship. Further investigations, with robust research designs, should be done to highlight the correlations. Identification of the most vulnerable groups may help to tailor psychological interventions to improve the outcome.
CONCLUSION
In conclusion, it is evident that a diagnosis of COVID-19 brings with it a significant mental distress. This shows that it will be beneficial for the patients suffering from mental stress and COVID to receive psychological assessment and management. An awareness about this issue along with provision of counselling services may be able to lessen the psychological burden of the COVID-19 outbreak. Further investigations should take place and a multidisciplinary approach should be adopted towards dealing with the COVID-19 pandemic.
- Rana W, Mukhtar S, Mukhtar S (2020) Mental health of medical workers in Pakistan during the pandemic COVID-19 outbreak. Asian J Psychiatr 51: 102080.
- Schultz WP, Khazian AM, Zaleski AC (2008) Using normative social influence to promote conservation among hotel guests. Soc Influ 3(1): 4-23.
- Kanadiya MK, Sallar AM (2011) Preventive behaviors, beliefs, and anxieties in relation to the swine flu outbreak among college students aged 18-24 years. Z Gesundh Wiss 19(2): 139-145.
- Mukhtar S (2020) Mental Health and Psychosocial Aspects of Coronavirus Outbreak in Pakistan: Psychological Intervention for Public Mental Health Crisis. Asian J Psychiatr 51: 102069.
- Banerjee D (2020) The COVID-19 outbreak: Crucial role the psychiatrists can play. Asian J psychiatry 50: 102014.
- Lovibond SH, Lovibond PF (1995) Manual for the Depression Anxiety & Stress Scales. (2nd Ed.) Sydney: Psychology Foundation.
- Husain W, Gulzar A (2020) Translation, adaptation and validation of Depression, Anxiety and Stress Scale in Urdu. Insights Depress Anxiety 4: 1-4.
- Lei L, Huang X, Zhang S, Min Xu, Jinorng Y, et al. (2020) Comparison of Prevalence and Associated Factors of Anxiety and Depression Among People Affected by versus People Unaffected by Quarantine During the COVID-19 Epidemic in Southwestern China. Med Sci Monit 26: e924609.
- Guo Q, Zheng Y, Shi J, Hua X, Wang Z, et al. (2020) Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: A mixed-method study. Brain Behav Immun 88: 17-27.
- Hossain MM, Tasnim S, Sultana A, Ping Ma, McKyer ELJ (2020) COVID-19 and suicide of an army soldier in India: Perspectives on psychosocial epidemiology of suicidal behavior. SocArXiv.
- Abad C, Fearday A, Safdar N (2010) Adverse effects of isolation in hospitalized patients: A systematic review. J Hosp Infect 76: 97-102.
- Purssell E, Gould D, Chudleigh J (2020) Impact of isolation on hospitalized patients who are infectious: Systematic review with meta-analysis. BMJ Open 10: e030371.
- Alexander JL, Dennerstein L, Kotz K, Richardson G (2007) Women, anxiety and mood: A review of nomenclature, comorbidity and epidemiology. Expert Rev Neurother 7(11 Suppl): S45-S58.
- Wang Y, Di Y, Ye J, Wei W (2020) Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med 26(1): 13-22.
- Özdin S, Bayrak Özdin Ş (2020) Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int J Soc Psychiatry 66(5): 504-511.
- Soni M, Curran VH, Kamboj SK (2013) Identification of a narrow post-ovulatory window of vulnerability to distressing involuntary memories in healthy women. Neurobiol Learn Mem 104: 32-38.
- Simpson R, Holmes EA, Perry VH, Tracey I, Wessely S, et al. (2020) Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatr 7(6): 547-560.
- Ng KH, Agius M, Zaman R (2013) The global economic crisis: Effects on mental health and what can be done. J R Soc Med 106: 211-214.
- Simpson RJ, Katsanis E (2020) The immunological case for staying active during the COVID-19 pandemic. Brain Behav Immun 87: 6-7.
- Butler MJ, Barrintos RM (2020) The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain Behav Immun 87: 53-54.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Chemotherapy Research Journal (ISSN:2642-0236)
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)

