Mini-Review
Anesthetic Challenges for Computerized Tomography Myelography in Operated Cases of Spine - A Case Series
4723
Views & Citations3723
Likes & Shares
Aims and objectives: To study challenges faced by anesthesiologists while performing computerized tomography (CT) Myelography with respect to difficult lumbar puncture, difficult airway, performing procedure in remote location (non-operating room) and day care management.
Materials and Methods: 30 patients who had undergone spine surgery and posted for CT Myelography were included in this study. The lumbar puncture was done in sitting or lateral position with 20/21 gauze spinal needle with median, paramedian or Taylor’s approach as feasible for the patient. Nonionic contrast material (Iohexol) was injected after lumbar puncture and patient was made prone and transferred to CT scan suite. Post-procedure, the patient was observed for two hours and then discharged.
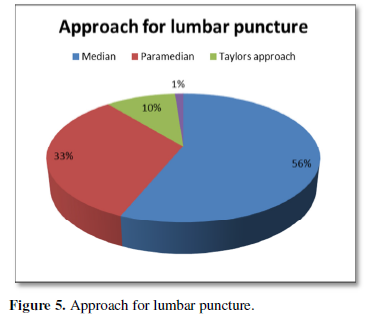
Results: Out of the 30 patients [12 post lumbar spine surgery and 18 post cervical spine surgery] 10required paramedian approach, three Taylor's approach and rest 17 midline approach for lumbar puncture. One patient, a four-year-old child, required TIVA. More than three attempts were required in 13 patients.
Discussion and Conclusion: Lumbar puncture procedure in operated lumbar spine cases is associated with difficulties like patient positioning, anatomical distortion, and presence of implant and use of high viscosity contrast. As the procedure was performed in CT scan suite difficulties of non-operating room anesthesia (NORA) were anticipated. In this case series, we report the difficulties faced and their management while doing CT Myelography procedure in operated cases of spine.
Keywords: Computerized Tomography Myelography, Operated spine
INTRODUCTION
Computerized Tomography (CT) Myelography is a specialized study of spinal region of interest where lumbar puncture is done first and then contrast is injected to study Cerebrospinal fluid (CSF) dynamics and spinal cord pathology [1].
Although Myelography have been largely superseded by the development of high-resolution CT and magnetic resonance imaging, it is performed for the following indications:
- Diagnosis of spinal cord pathologies: tumors and cysts
- Post-operative cases of spine to detect obstruction to CSF flow, spinal stenosis, CSF leak, CSF rhinorrhea and otorrhea.
Since anesthesia services are required for performing lumbar puncture in these patients, we decided to analyze the challenges faced by anesthesiologist while performing this procedure outside the operating room with regards to difficult lumbar puncture, difficult airway, procedure in remote location and day care management.
MATERIALS AND METHODS
The study included 30 patients undergoing CT Myelography, who had undergone either cervical or lumbar spine surgery over a period of one year. Detailed pre-operative assessment with special emphasis on airway assessment, neurological assessment and radiological imaging (antero-posterior and lateral view) of spine was done.
For the procedure difficult intubation trolley and resuscitative equipment were kept ready. After confirming adequate starvation and appropriate consent intravenous cannula was inserted and standard monitors were attached. Premedication with Inj. Ranitidine and Inj. Hydrocortisone was given. The procedure was done either in sitting or lateral position as per the patient's convenience. A 20G or 21G spinal needle was used for lumbar puncture as highly viscous contrast material was to be injected. A median, para-median or Taylor’s approach was chosen as per the palpation findings and nature of surgery done. After sterile skin preparation and infiltration of skin with 2ml of 2% Lignocaine at site of needle puncture, lumbar puncture was done using a 20G or 21G spinal needle. After obtaining clear and free flow of CSF, a nonionic contrast material, Omnipaque (Iohexol) 1mg/kg, was injected. Following this patient were made prone for half an hour to facilitate spread of contrast medium and then transferred to CT scan suite. Vitals were monitored throughout the procedure. The patients were also monitored for contrast reaction and side effects such as nausea, vomiting, rash, Pruritus, erythema, urticaria, bronchospasm and angioedema. After the procedure, patients were observed for two hours and then discharged. Patients were advised to report post dural-puncture headache (PDPH) during follow up.
RESULTS
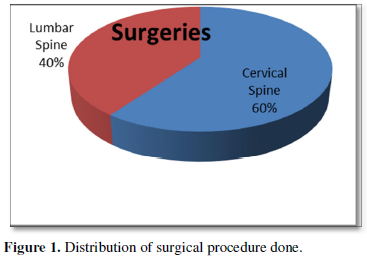
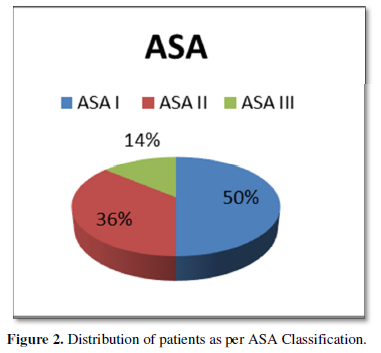
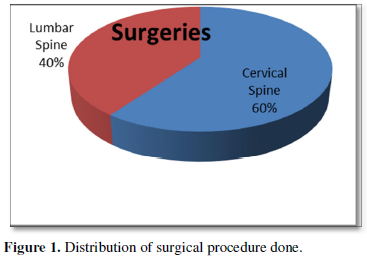
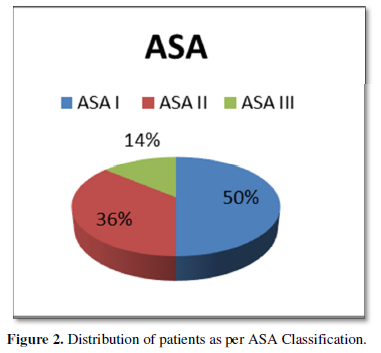
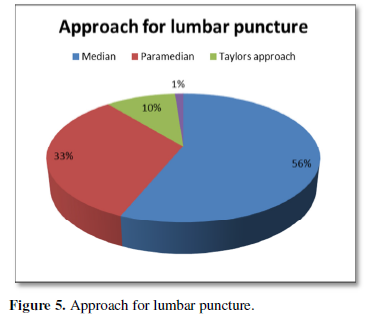
Out of 30 patients, 40% were operated cases of cervical spine and 60% were of lumbar spine (Figure 1). Patient’s age varied between 4 to 75 years with 56% of patients being less than 40 years age and including 46% of female patient. Of the 30 patients, 50% were of ASA I status, 36% were of ASA II and 14% were of ASA III status (Figure 2). Thirty-three percent of previously operated patients were with implant and 66% were without implant (Figure 3). For CT Myelography procedure 76% were given sitting position and remaining 24% were given lateral position (Figure 4). Depending on the comfort to the patient and convenience of the procedure in 57% of patient median approach was used, in 33% paramedian approach and in the remaining 10% Taylor’s approach was required (Figure 5). More than 3 attempts were required in 43% of patients and minor complications like headache; nausea- vomiting or Pruritus was noticed in 40% of patients.




DISCUSSION
Myelography typically involves performance of the lumbar puncture under fluoroscopic guidance followed by fluoroscopically monitored introduction into the subarachnoid space of a nonionic water-soluble iodinated contrast media that is FDA approved for intra-thecal administration. Myelography remains the gold standard investigation in following conditions.
- Demonstration of the site of a cerebrospinal fluid leak (post-lumbar puncture headache, post-spinal surgery headache, rhinorrhoea, or otorrhoea).
- Surgical planning, especially in regard to the nerve roots.
- Radiation therapy planning.
- Diagnostic evaluation of spinal or basal cisternal disease.
- Non-diagnostic MRI studies of the spine or skull base.
- Poor correlation of physical findings with MRI studies.
- Use of MRI precluded because of:
- Claustrophobia
- Technical issues, e.g., patient size
- Safety reasons, e.g., pacemaker
- Surgical hardware.
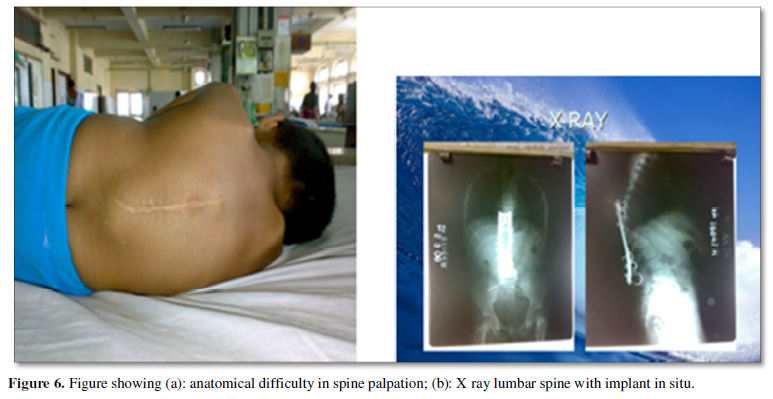
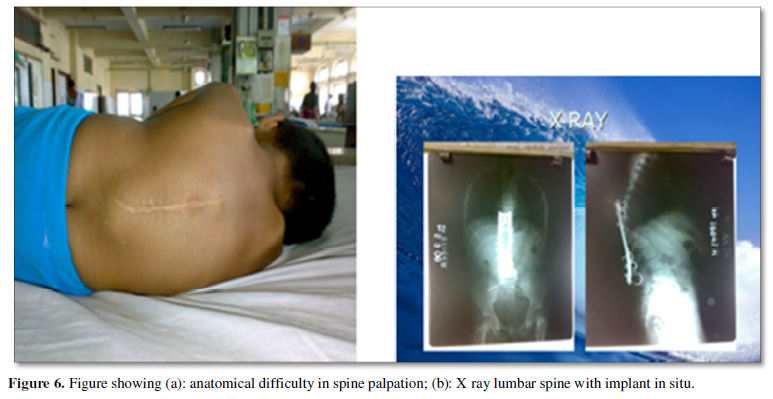
Operated cases of cervical spine may present with difficult airway due to problems such as fixed cervical spine, limited mobility and presence of neurological complication. Lumbar puncture in operated cases of lumbar spine presents technical difficulty. Therefore, x-ray plate’s antero-posterior and lateral views of spine should be obtained to know the number of operated segments, whether laminectomy has been done which would result in absent spinous process and whether there is sparing of L5 S1 interspace for Taylor’s approach. Spinal bony landmarks and radiological characteristics of the lumbar vertebrae are independent predictors of difficulty during spinal anesthesia [2]. Also, the procedure can become difficult due to the presence of implants and if the patient has other pathology like neurofibroma, Kyphoscoliosis.
As lumbar puncture is technically easier in sitting position, in 23 of 30 cases lumbar puncture was done in sitting position. In seven patients the position was lateral as they had difficulty in sitting (Figure 6).
In 17 of 30 patients’ lumbar puncture was done by median approach and in remaining 10 by paramedian approach when there was difficulty with median approach. Taylor’s approach was chosen in three patients in whom the other two methods were not feasible. Though lateral position is commonly preferred because of patient comfort, sitting position becomes a better option as palpation of spaces is easier and it is useful in obese patients and in patients with abnormal spinal curvature. Though the median approach is commonly chosen as first choice para-median approach is preferred in elderly patients and in patient with arthritic and deformed spine. Taylor’s approach is chosen for spine fusion, arthritic spine, opisthotonos etc. The occurrence of PDPH is more after diagnostic LP and Myelography as compared to spinal anesthesia. However, none of the patients reported PDPH as complication.
Anesthesia in remote locations has the following problems [3,4].
- Patients are admitted as day case including all age group.
- For unanticipated difficult airway in remote location, skilled help is not always available
- Unplanned procedure.
- Poor illumination.
- Untrained staff for anesthesia management.
- Equipment problems.
The following contrast reactions have been reported during Myelography.
- Minor contrast reactions: nausea, vomiting, urticaria, Pruritus, diaphoresis.
- Moderate contrast reactions: faintness, facial edema, laryngeal edema, bronchospasm.
- Severe reactions: pulmonary edema, cardio-respiratory arrest, seizures.
Use of low osmolality ionic and nonionic contrast media is associated with a lower overall incidence of adverse effects particularly not life-threatening ones. Serious contrast reactions are rare and occur in 1-2/ 10000 examinations using nonionic contrast media [5]. Also, there is very less data regarding anesthetic management of CT Myelography in operated cases of spine.
CONCLUSION
Anesthetic management for CT Myelography involves thorough pre-operative assessment, clinical and radiological investigations in view of difficult airway, difficult lumbar puncture, and preparedness for managing NORA complications, anesthesia in remote location, contrast reaction and day care procedures.
- Myelogram (2017) Johns Hopkins Medicine website. Accessed on: December 18, 2017. Available online at: https://www.hopkinsmedicine.org/healthlibrary/test%5Fprocedures/orthopaedic/myelogram%5F92,P07670
- Atallah MM, Demian AD, Shorrab AA (2004) Development of a difficulty scores for spinal anesthesia. Br J Anaesth 92: 354-360.
- Melloni C (2007) Anesthesia and sedation outside the operating room: how to prevent risk and maintain good quality. Curr Opin Anesthesiol 20: 513-519.
- Jason D. Walls, Mark S (2019) Weiss. Safety in Non-Operating room Anesthesia (NORA) APSF Newsletter 34(1): 3.
- Cochran ST, Bomyea K, Sayre JW (2001) Trends in adverse events after IV administration of contrast media. AJR Am J Roentgenol 176: 1385-1388.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Journal of Spine Diseases
- Journal of Clinical Trials and Research (ISSN:2637-7373)







