Review Article
Posterior Spinal Anesthesia for Orthopedic, Anorectic and Plastic Surgeries in Prone Position: It Should Be Used More
7604
Views & Citations6604
Likes & Shares
The prone position is used for a variety of procedures ranging from short duration procedures to major surgeries. The most frequently used surgeries are orthopedic, anorectal and plastic surgery. The dorsal (sensory) roots are generally larger than anterior (motor) roots; the dorsal roots are often blocked more easily. The spinal nerve is formed by the junction of the anterior roots (motor) with the posterior roots (sensitive). The baricity of anesthetics is an important factor to correctly indicate the technique for spinal anesthesia. To perform posterior spinal anesthesia, it is essential that the puncture is performed in the prone position, placing a pillow on the abdomen to open the intervertebral spaces. Hypobaric solutions should be indicated for posterior spinal anesthesia when the pneumatic tourniquet is not used, obtaining sensitive spinal anesthesia without motor block. However, in surgeries where the pneumatic tourniquet is essential, we can perform posterior spinal anesthesia with isobaric solution, obtaining sensory and motor blocks. The hypobaric solutions of local anesthetics in surgeries performed in the prone position provide predominantly sensory block after injection in the prone position. Major advantages were hemodynamic stability and patients’ satisfaction, being a good indication for outpatient anesthesia. In conclusion, posterior spinal anesthesia can be performed with hypobaric solutions (predominance of the sensitive part) or local anesthetic pure (blocking both roots).
Keywords: Anesthetics, Hypobaric and isobaric local anesthetic, Anesthetic Techniques, Regional posterior spinal block, Surgery, Orthopedic, Anorectic, Plastic
ABBREVIATIONS
CSF: cerebrospinal fluid; DMA 450: densimeter; S75:R25: Levobupivacaine in enantiomeric excess; POUR: Postoperative urinary retention
KEYPOINTS
Question
What is the reason for using Posterior Spinal Anesthesia very little in orthopedic, anorectal and plastic surgeries?
- Total ignorance of the technique?
- Difficulty performing subarachnoid puncture in prone position?
- Lack of knowledge of the anterior and posterior roots?
- Ignorance of the application of hypobaric solutions in the prone position.
- Ignorance of the application of isobaric solutions in the prone position.
Findings
Searching for articles in the literature, few manuscripts on the subject were found.
- There are some articles using saddle block, which is obtained with a hyperbaric solution, which privileges the motor roots in the ventral position.
- Some articles comparing hypobaric and hyperbaric solutions, showing the increased incidence of sensory block and low incidence of motor block and increased patient satisfaction with hypobaric anesthetic.
- The low incidence of cardiac and respiratory changes in the prone position with hypobaric solutions.
Meaning
- The use of posterior spinal anesthesia is uncommon worldwide and can be considered as ignorance of the benefits of this technique for patients operated in the prone position.
INTRODUCTION
The prone position is used for a variety of procedures ranging from major surgeries to short-term procedures. Some require tracheal intubation and others can be performed without intubation. Anorectal surgery [1,2] and posterior orthopedic surgery [3,4] can perfectly be performed with posterior spinal anesthesia in the prone position. However, the practice of posterior spinal anesthesia with hypobaric solutions remains relatively unknown to most anesthesiologists. Posterior spinal anesthesia with hypobaric solution is a promising alternative to the traditional and widely used technique of spinal anesthesia, severely restricting the anesthetized area, and thus decreasing the risk of adverse events and complications [5].
Studying the effect of spinal anesthesia with 2.5 ml of 5% heavy bupivacaine in lateral or sitting position for orthopedic surgeries of lower limbs and feet and then, the patient was placed in prone position demonstrating the total lack of knowledge of posterior spinal anesthesia [6]. It took the patient about 9 minutes to be placed in the prone position and with 18.3% hypotension. In addition, when placing the patient in the ventral position, the hyperbaric anesthetic will privilege the motor roots, which will result in a longer-lasting motor block than the residual analgesia produced by the local anesthetic. Unfortunately, the authors did not assess the degree of motor block and the duration of motor and sensory blocks.
Because the great majority of anesthesiologists use very little posterior spinal anesthesia with either hypobaric or isobaric solution, this article aims to explain the technique to be used and the main benefits of its performance.
Anatomy
The lumbar spinal canal is the site of numerous anesthetic interventions including injection of solution and the passage of catheters. The arrangement of the nerve roots in the subarachnoid space and their relationship to other tissues has several uncertainties. The dorsal root made of two divisions and a ventral root is unique exiting the dural sac at each level through separate dural perforations, uniting with the dorsal root ganglion. Spinal nerve roots are not uniform in size and structure having been shown that there is great interindividual variability in the size of the nerve root size [7]. Although the dorsal (sensory) roots are generally larger than anterior (motor) roots, the dorsal roots are often blocked more easily; this may explain the difference in the quality of spinal anesthesia in different patients.
In posterior (dorsal) spinal anesthesia with hypobaric solution and the patient in prone position, only the posterior roots are blocked since the solution floats in the cerebrospinal fluid (CSF) because the sensitive roots are in a higher position [8]. Using low doses of hypobaric solution, there is no concentration or quantity of local anesthetic to reach the motor roots below. Thus, it is unreasonable to perform spinal anesthesia with hyperbaric solution on a patient who will be operated on in the jack-knife position.
In the prone position, the hyperbaric solution, gravity takes the solution to the anterior region, even blocking the posterior roots. During recovery, the posterior roots can recover before the previous ones, allowing the patient to feel pain without moving the lower limbs, giving the false idea that the patient would still be anesthetized. Motor block is not a quality of spinal anesthesia. The hyperbaric solution in the prone position can progress in the cephalic direction, depending on the severity, producing motor blockage of the anterior thoracic roots, and preventing the patient from good ventilation. This could lead to hypoxia cardiac arrest [9].
Cerebrospinal Fluid (CSF)
After injection of the local anesthetic into the subarachnoid space, dilution by the CSF occurs before the drug reaches its site of action in the spinal cord. Individual variations in the volume of CSF in the subarachnoid space and the distribution in that volume will affect the result of spinal anesthesia.
A study with magnetic resonance imaging showed a great individual variability in CSF volumes in the lumbosacral region, from 28 to 81 mL [10]. There is a clinical correlation between CSF volume with hyperbaric lidocaine and isobaric bupivacaine solution between the level of block and the regression of sensory and motor blocks [11]. However, no study was found correlating the CSF volume and the hypobaric solutions of lidocaine and bupivacaine.
Spinal Nerves
The spinal nerve is formed by the fusion of two roots, an anterior (motor) and a posterior (sensitive) one. The fusion of the sensory and motor roots results in the spinal nerve, which, when leaving the intervertebral foramen, divides into the primary anterior branch and the primary posterior branch. Both have the function of innervating the chest, abdomen and lower limbs.
A cadaver study showed a large individual variation in the size of the nerve roots. The posterior roots ranged from 2.3 to 7.7 mm2 [12]. Another interesting data is the size of the posterior roots when compared to the previous ones, being enveloped being easily separable [7]. Although the posterior root might seem more impenetrable to the local anesthetic, its separation into bundles provides a greater contact surface for the penetration of the local anesthetic than the small anterior root. This may explain the relative easiness in providing sensory block in relation to the motor block.
Baricity
The relationship between the density of the local anesthetic and the CSF, known as baricity, is one of the most important determinants of the distribution of anesthetic within the subarachnoid space. Using DMA 450 densimeter showed that 0.15% bupivacaine, 0.15% enantiomeric excess levobupivacaine (S75:R25) and 0.6% lidocaine are hypobaric at 20oC, 25oC and 37oC [13].
In order to produce only sensitive spinal anesthesia for the correction of tendons in the leg, a block was performed with 0.10% bupivacaine, instead of commonly used at 0.15%. When comparing the baricity of the two solutions, it showed that 0.10% solution of bupivacaine was significantly more hypobaric than the 0.15% solution of bupivacaine [14]. Unilateral spinal anesthesia with 4 mg of 0.1% hypobaric bupivacaine (0.1%), allowed the movements of the ankle and foot (innervated by the sciatic) with complete analgesia, facilitating the surgeon's job to free the muscles and tendons [14].
The eloquence of the orthopedic specialty is movement. With this new technique, surgical analgesia was obtained, but without any degree of motor blockage.
The eloquence of the orthopedic specialty is movement. With this new technique, surgical analgesia was obtained, but without any degree of motor blockage.
The 5 mg dose of 0.1% hypobaric bupivacaine in posterior spinal anesthesia in anorectal surgeries provided anesthesia of only sensitive fibers in all patients, without any degree of motor block, with the presence of proprioception in 94% of patients [2].
Spinal puncture
Most anesthesiologists are used to saddle spinal anesthesia for anorectal surgery. Spinal anesthesia can be performed in three different ways: 1) with patients in lateral decubitus, 2) with patients in the sitting position and, 3) with the patients in the prone position.
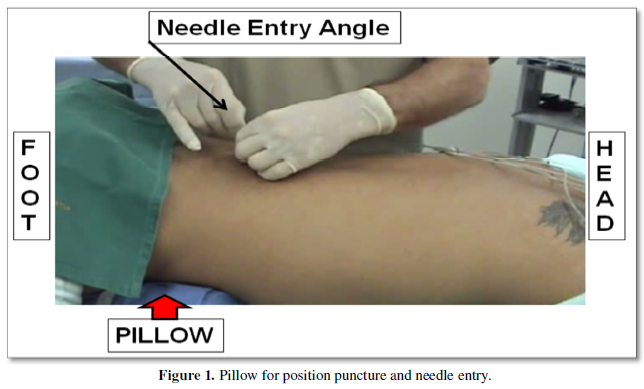
In the vertebral canal there is the dural sac formed by the outer membrane (dura mater), the inner membrane (pia mater) and finally by the arachnoid-mater and inside it are the spinal cord and nerve roots. The posterior radicles form the sensory roots and the anterior ones the motor roots. Therefore, puncture in the prone position with low doses of hypobaric solution (walk upwards) will mainly block the sensitive roots avoiding the blocking of the motor roots. To perform the puncture with prone patients’ position and a pillow should be placed under the abdomen to correct lordosis and increase the intermediate spinal space (Figure 1) [15].
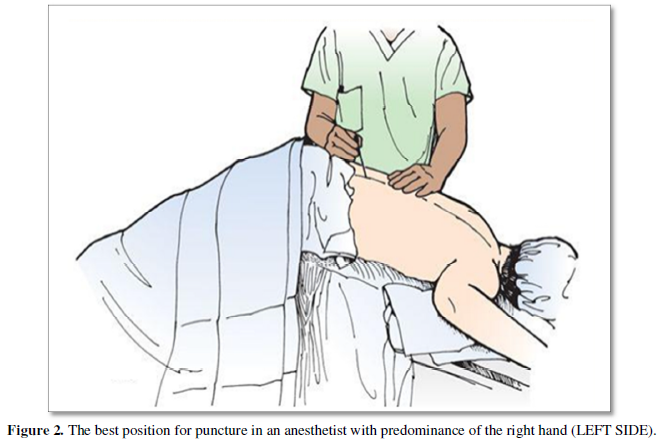
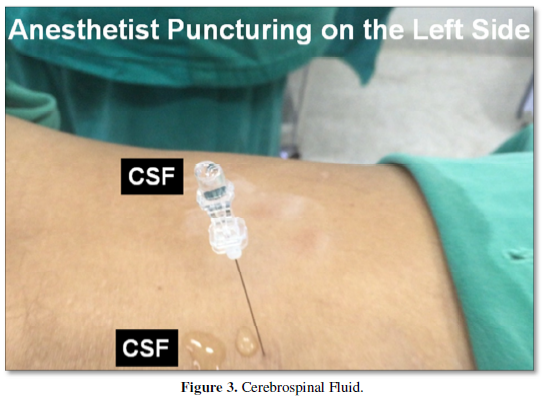
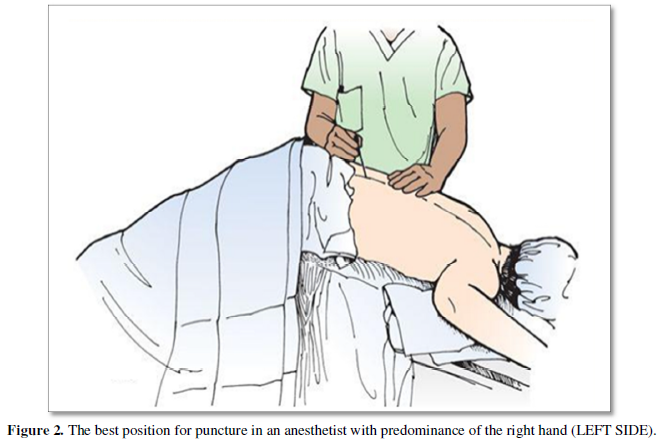
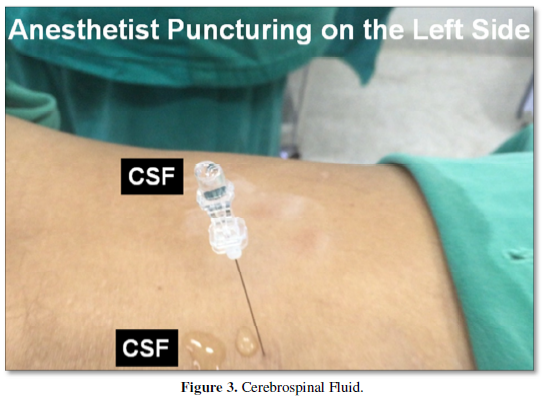
The sharp needles of 27G or 26G caliber provide an easier puncture avoiding the use of an introducer for the puncture with a pencil needle 25G or 27G calibers. The use of the introducer (20G) may cause accidental perforation of the dura mater [16]. Patients should be placed in the Jack-Knife with a pillow position, and the dose and type of anesthetics are injected in this position in order to block only the posterior radicles, thus avoiding the blocking of the anterior radicles. If the anesthesiologist has a predominance of the right hand, he should place himself on the patient's left side, taking advantage of the inclination of the vertebrae (Figure 2). If, however, he has the predominant left hand, he must place himself on the right side. After puncture, the CSF may appear slowly in the needle barrel. However, if there is a delay in the appearance, the patient should be asked to cough and this way the CSF will appear (Figure 3). A final solution is to aspirate the cannula from the spinal anesthesia needle with a 1 ml syringe. The advantage of the minimal motor block observed with this technique is the patient's ability to move from the operating table to the stretcher and also to walk early [1-4]. The main advantages of posterior spinal anesthesia include hemodynamic stability, patient satisfaction, and proprioception of the 1st toe, rapid recovery and no urinary retention [1-4].
Hypobaric Local Anesthetics
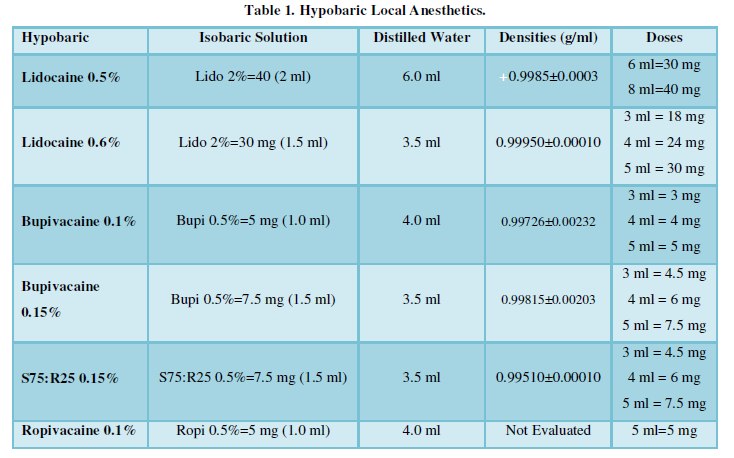
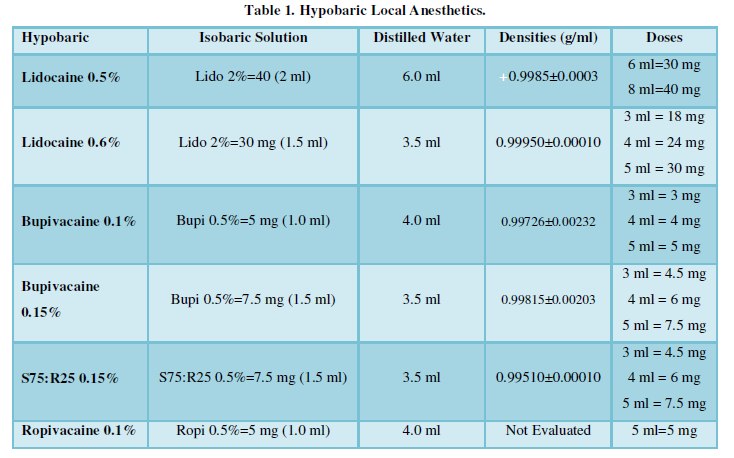
In Brazil, the first report of the use of hypobaric solution was with 0.1% tetracaine [17]. A few months later, the same group reported using 0.15% hypobaric bupivacaine [18]. The onset of action and the duration of posterior spinal anesthesia will depend on the dose and the type of anesthetic used. Low doses of 0.10% or 0.15% hypobaric bupivacaine or levobupivacaine in enantiomeric excess (S75:R25) and 0.6% hypobaric lidocaine can be used for anorectal surgery, gluteal prosthesis or orthopedic surgery in the prone position. The hypobaric solutions of lidocaine, bupivacaine and levobupivacaine in enantiomeric excess (S75:R25) can be obtained from the pure (isobaric) solution, according to dilution (Table I). In posterior spinal anesthesia with hypobaric anesthetic, the injection speed should be 1 ml/15 s, with any kind of local anesthetic (Table 1).
The use of 6 to 8 ml of 0.5% hypobaric lidocaine injected in a prone position produces effective spinal anesthesia for the perirectal surgery in the Jack-Knife position [19]. The patient must remain upside down (Trendelenburg position) or supine for at least one hour after the injection to minimize the cephalic migration of the block.
In order to compare the onset of the block, cephalic dispersion and duration of the motor block after the administration of 5 mg of 0.1% hypobaric ropivacaine alone or associated with adjuvants such as clonidine or fentanyl for spinal anesthesia for anorectal surgery in the pocket knife position [20]. The 0.1% hypobaric ropivacaine provides adequate surgical conditions for anorectal surgeries. The addition of clonidine was better than fentanyl because it improves the quality of the sensory block and provides postoperative analgesia for longer periods. Recovery is faster resulting in shorter duration associated with better hemodynamic profile [21].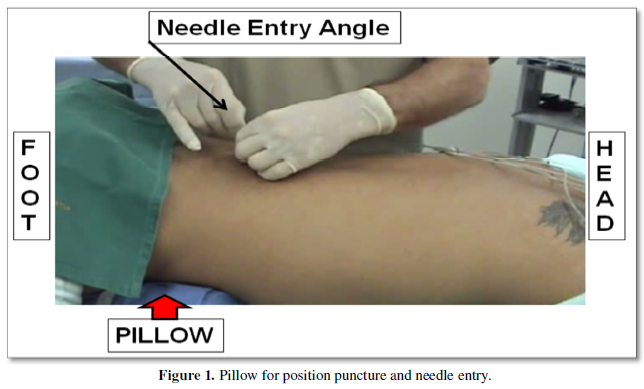
Isobaric Local Anesthetics
In several countries, most authors prefer to name substances considered isobaric as pure. In reality there is not an isobaric solution. The most used pure local anesthetics are: bupivacaine, levobupivacaine in enantiomeric excess (S75:R25), lidocaine and ropivacaine. When using pure local anesthetics, the uniform distribution of the drug in the subarachnoid spaces provides the same amount for both parts: anterior and posterior regions.
Assessing the densities of all anesthetics used in spinal anesthesia in the same way as adjuvants, he showed that the pure solutions of lidocaine, bupivacaine, levobupivacaine in enantiomeric excess (R75:S25) are hypobaric when measured at 37oC [13]. In this study, the temperature of 37oC changed the density of all pure solutions, transforming them into hypobaric solutions, the same result obtained in another article [22]. In this way, puncture in prone position with pure anesthetics that has a density very close to the lowest CSF value, these anesthetics block both anterior and posterior roots. The injection of local anesthetic in the CSF (temperature ±37oC), it has a great chance of blocking the posterior (sensitive) roots more than the anterior (motor) roots. This results in a longer duration of the sensory block than the motor block [23].
Recovery of Block
Recovery from posterior spinal anesthesia depends on the type and dose of anesthetic used. 0.6% lidocaine provides 63 min recovery with 18 mg, 81 min with 24 mg and 89 min with 30 mg [24]. Already at 0.15% hypobaric bupivacaine recovery from blockade was 115 min with 4.5 mg, 135 min with 6 mg and 195 min with 7.5 mg [25]. The duration of pure (isobaric) solutions for posterior spinal anesthesia will depend mainly on the substance and the dose used.
Tourniquet Application
The use of a tourniquet is a common practice in orthopedic and plastic surgery of the lower limbs. They are compressive devices that occlude blood flow to the limbs to create bloodless surgical field and decrease the perioperative blood loss. The use of a tourniquet can cause extreme pain during surgery, depending on the type of anesthesia used. Several techniques and drugs have been used to reduce the pain of using the tourniquet [26]. Among these techniques, the use of spinal anesthesia is indicated.
The use of the tourniquet provides local effects due to the compression and ischemia caused by it. The tourniquet pain is poorly located, tense, in the applied place, causing inconvenience for the anesthesiologist and concern for surgeons. Thus, posterior spinal anesthesia with hypobaric anesthetics tends to provide only blockage of sensitive roots. In this way, as it does not block the motor roots, the use of the pneumatic tourniquet provides an unbearable ischemic pain for the patient, requiring heavier sedation. Thus, when performing surgery with a tourniquet in prone position, the indication is the use of isobaric anesthetics [23].
The 2% isobaric lidocaine at the dose 50 and 60 mg has provided sensory and motor block after injection in the prone position, for ambulatory calcaneous surgeries, provided an effective fast onset and short duration spinal anesthesia, with no incidence of failures, without tourniquet perception and no TNS thus being indicated for orthopedic surgeries lasting less than 100 min [24].
The use of posterior spinal anesthesia in patients who will use a tourniquet should be any isobaric local anesthetic such as bupivacaine, levobupivacaine in enantiomeric excess (S75:R25), ropivacaine and lidocaine.
Orthopedic Sugery
Studying 50 mg of 2% pure lidocaine with 24 mg 0.6 hypobaric lidocaine provided adequate spinal anesthesia for outpatient foot surgeries when operated in prone position [3]. The onset of action was fast with both solutions and the duration was dose dependent. The hypobaric solution blocked only the posterior sensitive roots in all patients, while the pure solution (isobaric) blocked both the sensitive and motor roots. Thus, if there is a need to use a pneumatic tourniquet, the recommended solution should be pure (isobaric). One advantage of minimum motor block observed with hypobaric lidocaine was patients’ ability to go from the operating table to the stretcher and of early ambulating. Isobaric lidocaine induces total motor block with patients’ immobility, allowing for hospital discharge only after total blockade recovery. With 0.15% hypobaric bupivacaine, the duration of analgesia was dose dependent, ranging from 115 to 195 min [25].
Anorectic Surgery
Spinal anesthesia with conventional dose may be undesirable for regimen procedures ambulatory due to prolonged limb motor block with consequent change to the hospitalization regime unplanned hospital. Thus, anesthesiologists need to familiarize themselves with techniques that provide rapid recovery from subarachnoid block, and mainly with techniques that avoid the unpleasant and unnecessary motor block of the lower limbs in anorectal surgeries [1,2,23]. Hypobaric lidocaine at 0.6% concentration predominantly provided a sensory block after injection in the prone Jack-Knife position (ventral decubitus) [24]. The smallest dose (18mg) provides sufficient analgesia with a lesser dispersion and a shorter duration. The major advantages were hemodynamic stability and a high degree of patient satisfaction.
Plastic Surgery
There is a great demand from patients looking for procedures to sculpt the body. Buttock contouring is a complex process that requires individual patient evaluation and desire for the proper choice of the procedure to be performed. Most procedures for gluteal prosthesis or liposuction can be performed with venous sedation and wetting solution, general anesthesia, spinal anesthesia or epidural anesthesia [27]. Normally, the patient is operated in the prone position, raising the pelvis with a pocket knife-shaped pillow (Jack-Knife position), making dissection easier. In this way, the patient will be operated in the ideal position to perform a posterior spinal anesthesia with a hypobaric solution of local anesthetic.
Postoperative analgesia
Pain in the postoperative setting is an unwanted side effect of surgery directed to improve morbidity or mortality. There are several potential benefits of optimal postoperative pain control. Opioids are important for the relief of perioperative pain; however, they present several side effects such as nausea, vomiting, pruritus, paralytic ileo, respiratory depression, and they may also develop opiate-induced hyperalgesia. A recent systematic review conducted in 2017 suggests that 42-71% of all opioid pills prescribed after the operation are not used [28]. Therefore, these opioids are prescribed unnecessarily and may become available for misuse. The prescription of opioids in the treatment of postoperative pain varies widely and is often used in excess, and is not significantly different between minor and major surgical procedures mainly after minor surgical procedures [28]. The continued use of opioids for a long time in the postoperative period represents yet another previously underestimated surgical complication, which justifies greater awareness [28]. The use of adjuvants by anesthesiologists in the same syringe with a local anesthetic alters the baricity of the anesthetic site [13].
Pain in the postoperative setting is an unwanted side effect of surgery directed to improve morbidity or mortality. There are several potential benefits of optimal postoperative pain control. Opioids are important for the relief of perioperative pain; however, they present several side effects such as nausea, vomiting, pruritus, paralytic ileo, respiratory depression, and they may also develop opiate-induced hyperalgesia. A recent systematic review conducted in 2017 suggests that 42-71% of all opioid pills prescribed after the operation are not used [28]. Therefore, these opioids are prescribed unnecessarily and may become available for misuse. The prescription of opioids in the treatment of postoperative pain varies widely and is often used in excess, and is not significantly different between minor and major surgical procedures mainly after minor surgical procedures [28]. The continued use of opioids for a long time in the postoperative period represents yet another previously underestimated surgical complication, which justifies greater awareness [28]. The use of adjuvants by anesthesiologists in the same syringe with a local anesthetic alters the baricity of the anesthetic site [13].
Orthopedic surgery is associated with intense pain and adequate control through peripheral nerve blocks improves the patient's recovery, physical therapy and is associated with greater patient satisfaction. The benefits of peripheral nerve blocks are numerous and include improvement in clinical, economic, and humanistic outcomes. Due to the numerous benefits of peripheral nerve blocks in the treatment of pain in orthopedic patients, their use has expanded in recent decades. Several peripheral nerves blocks can be performed for postoperative analgesia in orthopedic surgeries with neurostimulator or ultrasound such as: fascia iliaca compartment block, lumbar plexus inguinal or compartmental psoas, quadratus lumborum block, erector spine plane block, pericapsular nerve block [29], and all approaches to the sciatic nerve [3,14,23]. Usually, depending on the anesthetic used and the dose, 20-hour analgesia can be obtained.
Another concern is the control of postoperative pain. The pain postoperative after anorectal surgery is very intense and needs parenteral opioids in general that are employed in hospitals. The first postoperative defecation is extremely painful and some patients prefer pain without surgery. The pudendal nerve derives from sacral nerves S2, S3 and S4. In theory, pudendal blockage enables analgesia or anesthesia of perineal region, which is frequently performed by surgeons or obstetricians. Bilateral pudendal nerve block with 20 ml of 0.25 percent bupivacaine oriented by nerve stimulator provided excellent analgesia with low need for opioids and without urinary retention [30]. Bilateral blockade of the pudendal nerve using a neurostimulator with mean 23.4 hours provided better relief of postoperative pain, reducing the need for analgesics and residual analgesia for more than 24 hours in 41% of patients [31]. All patients who received bilateral pudendal block had spontaneous micturition versus 96 in the control group. There was no local or systemic complication. The bilateral pudendal nerve block with the aid of peripheral nerve stimulator or ultrasound for postoperative analgesia with local anesthetic may be a better way to treat pain, with mean 24 h analgesia with the first pain-free evacuation.
Plastic surgeries performed with posterior spinal anesthesia can be: liposuction with gluteal lipoinjection, improvement is desired, liposuction with gluteal implants, and gluteoplasty. Liposuction is one of the most common treatment modalities in cosmetic surgery, and several anesthetic techniques can be used: local, regional (spinal or epidural anesthesia), conscious sedation, and general anesthesia. The choice of anesthesia technique used for liposuction depends on the surgeon and anesthesiologist, patient comorbidities, patient positioning, anatomical areas to be treated, type of liposuction, duration and extent of the procedure and volume of planned liposuction. Using spinal anesthesia, the quality and relaxation are excellent and associating opioids with the local anesthetic provides good analgesia in the first 24 hours after surgery [32].
Urinary Retention
Postoperative urinary retention (POUR) is one of the postoperative complications which is often underestimated and often gets missed and causes lot of discomfort to the patient. Various perioperative factors can potentially influence the occurrence of urinary retention in the postoperative period: age, gender, neurologic abnormality, urinary tract pathology, surgical procedure, anesthetic technique, and intraoperative fluid administration, duration of surgery, postoperative pain and postoperative opioids [33].
Unilateral spinal anesthesia and posterior spinal anesthesia with different solutions of local anesthetics without opioids for orthopedic and anorectal surgery is associated with the absence of POUR in these techniques [1-4,14,23-25]. Analgesia in these studies was performed with peripheral nerve block.
Evaluating articles published in the literature, no study was found comparing the effect of baricity of local anesthetics on bladder function. In several studies of our group with isobaric, hyperbaric and hypobaric solutions in low doses for anorectal and orthopedic surgeries, no case of POUR was observed. In all of these studies, opioids were not associated with local anesthetics. Several studies on humans have consistently shown that spinal opioids influence bladder functions and cause urinary retention [33,34].
In a recent study comparing sciatic nerve block with neurostimulation with two doses of morphine associated with local anesthetic for spinal anesthesia for orthopedic surgery, demonstrated that sciatic nerve block provides longer duration of analgesic, lower incidence of side effects, higher incidence of satisfaction [35]. The incidence of urinary retention was significantly higher with 100 μg compared to 80 μg of morphine. There was no complication with the use of 40 ml of 0.25% bupivacaine for sciatic nerve block. The duration of analgesia was significantly longer with sciatic nerve block (23±3 h) compared with patients who received morphine (15±5 h).
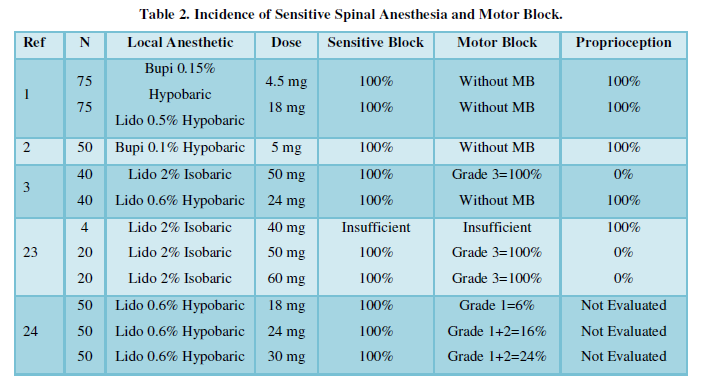
Incidence of Sensitive and Motor Block (Table 2)
In several studies, the lower the dose of the hypobaric solution, regardless of the type of local anesthetic, provides greater selectivity of sensory block with little or no motor block. Likewise, the duration of analgesia is always dose dependent. However, when using the isobaric solution, sensory block occurs in all patients with different degrees of motor block depending on the dose of the local anesthetic. Likewise, the duration of the blocks is dose dependent.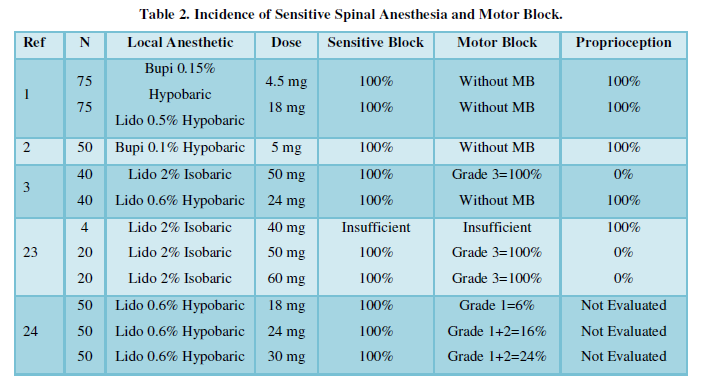
Advantages Posterior Spinal Anesthesia
The practice of prone positioning for performing spinal dorsal anesthesia remains relatively unfamiliar to many anesthetists. Patients orthopedic surgery, anorectal surgery, and plastic surgery when performed in the dorsal position may be anesthetized and remain in this position during the surgical procedure. A slight cephalodeclive during puncture allow hypobaric anesthetic block predominantly posterior roots.
Thus, the block had been restricted lower roots preventing its dispersion to the higher roots. The fact that there is a predominance of sensitive roots at the expense of the motor roots, these patients have an excellent analgesia and motor blockade absent or mild, allowing patients to move from the surgery table to stretcher. Most patients remain with the presence of proprioception evaluated in the 1st pododactyl of both limbs.
In the patient in a pocketknife position used for subarachnoid puncture in the prone position it is recommended to place a cushion or pillow under the abdomen to reduce lordosis and increase the intervertebral space. The switchblade position allows the hypobaric anesthetic to be restricted to the lumbosacral roots, and also prevents motor blocking of the lower limbs, and cephalic dispersion, responsible for the decrease in ventilatory capacity, and with this hypoxemia with cardiac arrest. The use of hyperbaric solutions and the prone position may be responsible for high cephalad dispersion and predominant blockade of motor roots with cardiac arrest [9]. In reality, the total lack of knowledge about the physiology of spinal anesthesia and the proper use of all its modalities of spinal anesthesia will allow these accidents to be avoided [8], since spinal anesthesia will be restricted mainly to sensitive roots.
The distribution of the hypobaric solution depends on the position of the patient and the anatomy of the spinal column. Therefore, a selective sensory block (or predominant in relation to the motor) is produced when a hypobaric solution of lidocaine, bupivacaine, enantiomeric excess bupivacaine or ropivacaine is used in the pocket position, promoting little or no motor block. The latency time is short, being shorter with lidocaine than with bupivacaine or ropivacaine. The duration of the block depends on the anesthetic used and the dose used.
Another important factor for the use of posterior spinal anesthesia is patient satisfaction during surgery, being able to mobilize the legs always under command and finally transfer from the operating table to the transport stretcher.
When the surgery is performed in the prone position, posterior spinal anesthesia has several advantages, such as: the subarachnoid puncture will be performed in the surgical position, the hypobaric anesthetic is restricted to the final thoracic and lumbosacral roots, there will be a predominance of sensory block compared to the motor, the patient will not feel pain and will be able to move the lower limbs, low incidence of cardiac-circulatory changes, the patient will be able to move from the operating table to the transport stretcher and increased satisfaction.
CONCLUSION
Posterior Spinal Anesthesia is little used worldwide mainly due to the total ignorance of its benefits, mainly in cardiac arrests in patients operated in the prone position with hyperbaric solutions. In addition, as few anesthesiologists use it to teach the new generation, it is not routinely used in the various Anesthesia Teaching Centers. Thus, the training of anesthesiologists may change with the study of this article.
- Imbelloni LE, Gouveia MA, Cordeiro JA (2010) Hypobaric 0.15% bupivacaine versus hypobaric 0.6% lidocaine for posterior spinal anesthesia in outpatient anorectal surgery. Rev Bras Anestesiol 60: 113-120.
- Imbelloni LE, Sakamoto JW, Viana EP, Araujo AA, Souza NN, et al. (2020) Morais Filho GB. Hypobaric bupivacaine 0.1% (5 mg) for dorsal anorectal surgery compared with hyperbaric bupivacaine 0.5% (5 mg) for anorectal lithotomy surgery on an outpatient basis. Rea Int J Commun Med Pub Health 1: 023-028.
- Imbelloni LE, Sales MBL, Ventura TB, Camacho L, Filho MGB (2018) Lidocaine for dorsal spinal anesthesia for ambulatory orthopedic foot surgery. A comparative study between isobaric and hypobaric solutions. World J Pharm Pharm Sci 7: 139-149.
- Imbelloni LE, Figueiredo LG, Santos JAC, Galvão AA (2018) Posterior spinal anesthesia for bilateral calcaneous fracture in cardiac patients: A case report. J Anesth Pain Med 3: 1-3.
- Imbelloni LE (2014) Spinal hemianesthesia: Unilateral and posterior. Anesth Essays Res 8: 270-276.
- Alkhayarin M, Shaikh N, Ghouri SI (2018) Vegesna ARR. Standard spinal anaesthesia then turned prone for lower limb orthopaedic surgeries. Int J Anesth Pain Med 4: 4.
- Hogan Q, Toth J (1999) Anatomy of soft tissues of the spinal canal. Reg Anesth Pain Med 24: 303-310.
- Imbelloni LE, Gouveia MA. (2017) Understanding spinal anesthesia. World J Pharm Pharmaceut Sci 6: 38-46.
- Lovstad RZ, Granhus G, Hetland S (2000) Bradycardia and asystolic cardiac arrest during spinal anaesthesia: A report of five cases. Acta Anaesthesiol Scand 44: 48-52.
- Hogan QH, Prost R, Kuller A, Taylor ML, Liu S, et al. (1996) Magnetic resonance imaging of cerebrospinal fluid volume and the influence of body habitus and abdominal pressure. Anesthesiology 84: 1341-1349.
- Carpenter RL, Hogan QH, Liu SS, Crane B, Moore J (1998) Lumbosacral cerebrospinal fluid volume is the primary determinant of sensory block extent and duration during spinal anesthesia. Anesthesiology 89: 24-29.
- Hogan Q (1996) Size of human lower thoracic and lumbosacral nerve roots. Anesthesiology 85: 37-42.
- Imbelloni LE, Moreira AD, Gaspar FC, Gouveia MA, Cordeiro JA (2009) Assessment of the densities of local anesthetics and their combination with adjuvants. An experimental study. Rev Bras Anestesiol 59: 154-165.
- Imbelloni LE, Rava C, Gouveia MA, Barbosa R (2016) Unilateral sensitive spinal anesthesia. Case report. J Anesth Crit Care 6: 00227.
- Kahn CH, Blank JW, Warfield CA (1996) Regional Anesthesia: An Atlas of Anatomy and Techniques. St Louis: Mosby Year Book, Inc. pp: 285‑294.
- Imbelloni LE (2018) Sales MBL. Accidental perforation of subarachnoid space with spinal introducer: Case Report. Int J Anesthet Anesthesiol 5: 074.
- Gouveia MA, Labrunie GM (1985) Raquianestesia hipobárica com tetracaína 0.1%. Rev Bras Anestesiol 35: 232‑233.
- Gouveia MA, Labrunie GM (1985) Raquianestesia hipobárica com bupivacaína 0.15%. Rev Bras Anestesiol 35: 519‑521.
- Bodily MN, Carpenter RL, Owens BD (1992) Lidocaine 0.5% spinal anaesthesia: A hypobaric solution for short-stay perirectal Can J Anaesth 39: 770-773.
- Dhasmana S, Vishwakarma Y, Singh V, Imran M (2015) Hypobaric ropivacaine (0.1%) in spinal anesthesia with or without low-dose clonidine or fentanyl for anorectal surgery. Ain-Shams J Anesthesiol 08: 594-601.
- Mohta M (2015) Ropivacaine: Is it a good choice for spinal anesthesia? J Anaesthesiol Clin Pharmacol 31: 457-458.
- Richardson MG, Wissler RN (1997) Densities of dextrose-free intrathecal local anesthetics, opioids and combinations measured at 37 degrees C. Anesth Analg 84: 95-99.
- Imbelloni LE, Carvalho SM, Anjos D, Camacho L, Morais Filho GB (2018) Lidocaine 2% pure for orthopedic calcaneal surgery in decubitus ventral. Study with different doses. J Clin Anesth Pain Med 2: 019
- Imbelloni LE, Gouveia MA, Vieira EM, Cordeiro JA (2008) Selective sensory spinal anaesthesia with hypobaric lidocaine for anorectal surgery. Acta Anaesthesiol Scand 52: 1327‑1330.
- Imbelloni LE, Gouveia MA, Vieira EM, Cordeiro JA (2009) A randomized, double‑blind comparison of three different volumes of hypobaric intrathecal bupivacaine for orthopaedic surgery. Anaesth Intens Care. 37: 242‑247.
- Saied A, Mousavi AA, Arabnejad F, Heshmati AA (2015) Tourniquet in surgery of the limbs: A Review of history, types and complications. Iran Red Crescent Med J 17(2): e9588.
- Mendieta CG (2003) Gluteoplasty. Aesthet Surg J 23: 441-455.
- Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, et al. (2017) New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg 152: e170504.
- Dangle J, Kukreja P, Kalagara H (2020) Review of current practices of peripheral nerve blocks for hip fracture and surgery. Curr Anesth Rep 10: 259-266.
- Imbelloni LE, Vieira EM, Gouveia MA, Gomes Netinho JG, Spirandelli LD, et al. (2007) Pudendal block with bupivacaine for postoperative pain relief. Dis Colon Rectum 50: 1656-1661.
- Imbelloni LE, Vieira EM, Carneiro AF (2012) Postoperative analgesia for hemorrhoidectomy with bilateral pudendal blockade on an ambulatory patient: A controlled clinical study. J Coloproctol 32: 291-296.
- Regatieri FL, Masquera MS (2006) Liposuction anaesthesia techniques. Clin Plastic Surg 33: 27-37.
- Agrawal K, Majhi S, Garg R (2019) Post-operative urinary retention: Review of literature. World J Anesthesiol 8: 1-12.
- Baldini G, Bagry H, Aprikian A, Carli F (2009) Postoperative urinary retention: Anesthetic and perioperative considerations. Anesthesiology 110: 1139-1157.
- Imbelloni LE, Pistarino MA, Ventura TB, Viana EP, Oliveira Jr AS, et al. (2020) Postoperative analgesia in lower limbs orthopedic surgeries: A comparative study between sciatic nerve block and spinal morphine. EC Emergency Medicine and Critical Care. 4: 64-73.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Alcoholism Clinical Research
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- International Journal of AIDS (ISSN: 2644-3023)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)





