5165
Views & Citations4165
Likes & Shares
Aim: The aim of this study was to clinically evaluate the efficacy of A-PRF membrane when used along with CAF in the treatment of Millers class-II gingival recession defects.
Materials and methods: A total of 40 gingival recession sites were selected from these 20 patients with bilateral gingival recession sites in each patient. They were randomly divided into 2 groups by drawing sealed envelopes containing the clinical procedure to be performed; Control Group - Coronally advanced Flap procedure; Study Group - Coronally advanced procedure with A-PRF membrane. Presurgical procedures, surgical procedures as well as A-PRF preparations were performed by the principal investigator. The clinical parameters that were evaluated are Probing depth (PD), Clinical attachment loss (CAL), Gingival recession height (GRH), Gingival recession width (GRW) and Width of the keratinized gingiva (KGW).
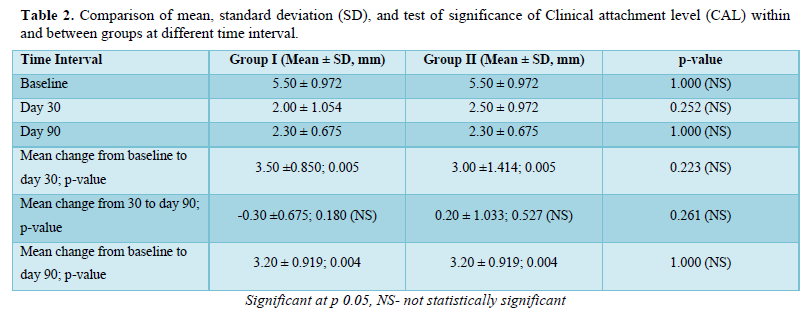
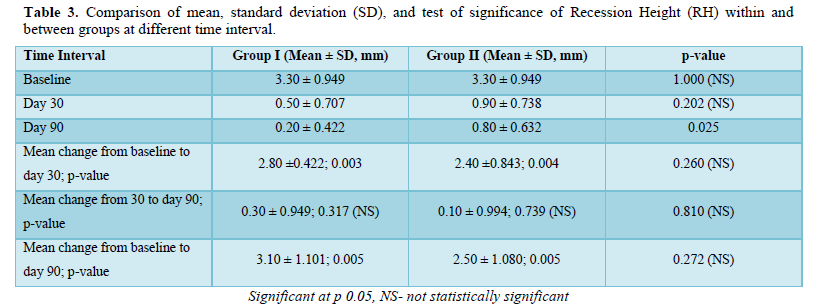
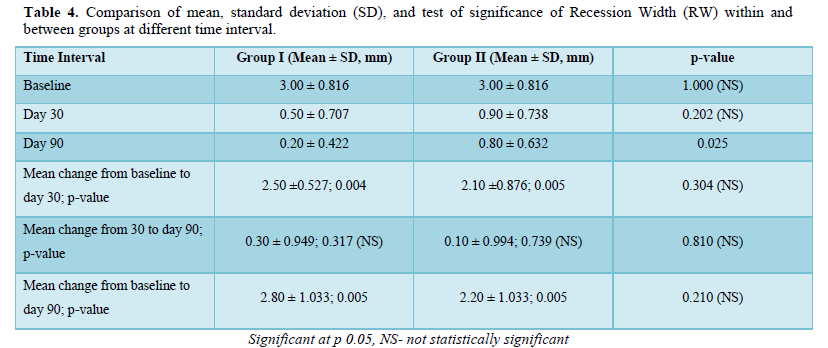
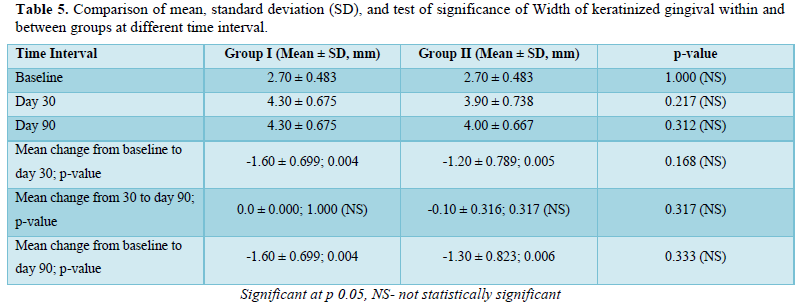
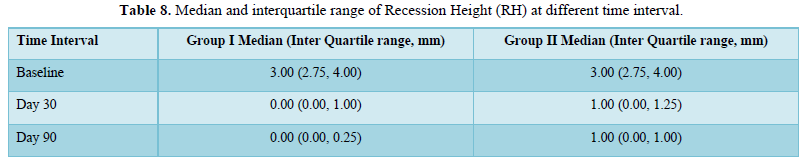
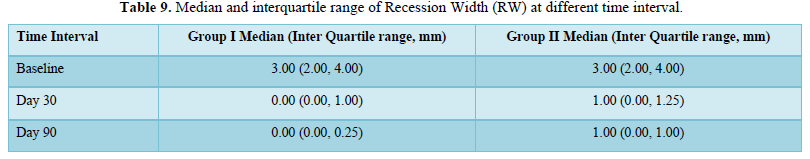
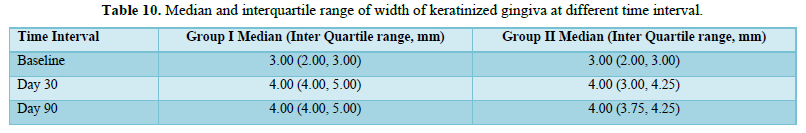
Results: Comparing the mean and standard deviation (SD) of Recession Width (RW) and Recession Height (RH) between the groups were found to be statistically significant at day 90 with the p-value of 0.025 in both the parameters.
Conclusion: Within the limitations of the study, we conclude that additional application of A-PRF with CAF provides advantages of earlier healing and quicker attainment of optimal gingival tissue thickness which was maintained throughout the follow-up period due to enriched platelets and growth factors present in the membrane.
Keywords: Gingival recession, Coronally advanced flap, Platelet rich fibrin, Wound healing
There are three different types of approaches that are commonly performed to achieve root coverage; the free gingival graft, the coronally advanced flap (CAF) and combined procedures involving CAF with tissue/material interposed between the flap and root surface. CAF has been tried with varying degrees of success to cover the recession defects [3]. Histologically, this technique leads to reformation of junctional epithelium and the connective tissue attachment with minimal bone repair [4]. The connective tissue attachment achieved by CAF is not stable over long periods, and various adjunctive agents have been used to promote healing and to further enhance the clinical outcomes. Thus, grafts and biomaterials are used along with coronally advanced flap to promote healing and enhance clinical outcomes over long periods of time. One among them is the A-PRF (Advanced Platelet Rich Fibrin) which is a third-generation platelet concentrate. This biomaterial comprises enormous amounts of platelets and growth factors that are trapped within the membrane and released over a period of time [5]. An added advantage of A-PRF is that it easy to procure as it is prepared from the patient’s own blood and is highly biocompatible with minimal or no patient morbidity. The aim of this study was to clinically evaluate the efficacy of A-PRF membrane when used along with CAF in the treatment of Millers class-11 gingival recession defects.
METHOD AND MATERIALS
Study Design: The study was designed as a randomized clinical study conducted in the Out-patient department, Department of Periodontics, Meenakshi Ammal Dental College and Hospital. Approval was obtained from the Institutional Ethical Committee and all participants read and signed an informed consent form explaining all the study-related procedures before inclusion in the study. A total of 20 patients were recruited into the study. They were randomly divided into 2 groups by drawing sealed envelopes containing the clinical procedure to be performed.
Control Group: Coronally advanced Flap procedure
Study Group: Coronally advanced procedure with A-PRF membrane
Subject Selection
Twenty patients, ranging in age from 20 to 45 years reporting to the Out-patient department, Department of Periodontics, Meenakshi Ammal Dental College and Hospital were recruited into the study. All subjects presented with bilateral gingival recession (Miller’s class - II) in their maxillary canine/premolar region with a complaint of sensitivity and/or unaesthetic appearance.
A total of 40 gingival recession sites were selected from these 20 patients with two gingival recession sites in each patient. The study was performed from November 2019 to February 2020.
Presurgical procedures included oral hygiene instructions, full-mouth scaling, root planning and polishing of the surgical site. Surgical procedures as well as A-PRF preparations were performed by the principal investigator.
Inclusion criteria
- Bilateral Miller's Class II gingival recession in the maxillary canine/premolar region (no loss of interdental hard and soft tissue height)
- Systemically healthy subjects
- Patients willing to comply with all study - related protocols
- Patients capable of maintaining high standards of oral hygiene.
Exclusion criteria
- History of previous surgery in the surgical site
- Use of antibiotics in the past 3 months
- Root surface caries/restoration in the surgical site
- Presence of root caries requiring restoration in the surgical site
- History of smoking or current smokers
- Primary or secondary trauma from occlusion
- Patients taking steroids or medications known to cause gingival enlargement.
Clinical Parameters
All clinical parameters required for the study were recorded by a blinded examiner using a UNC-15 Probe. The parameters were recorded at baseline, 30- and 90-days postsurgical procedure.
Measuring stents for each surgical site were fabricated from self-curing acrylic resin. Clinically reproducible measuring points were marked on the stent at the mesio-buccal, mid-buccal, and disto-buccal aspects as standardized reference points. The stents were stored safely till the last measurement was recorded.
The following parameters were recorded:
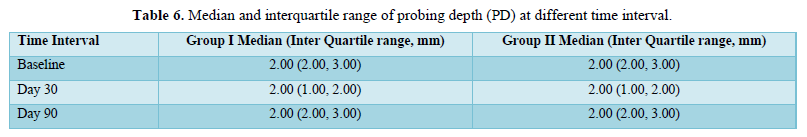
- Probing depth (PD) was measured at three points - mesio-buccal, mid-buccal and disto-buccal. The measurement was made from the free gingival margin to the bottom of the sulcus
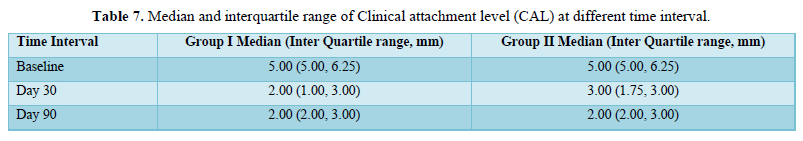
- Clinical attachment loss (CAL) was measured at the same reference points used for PD. The measurement was made from the cement enamel junction (CEJ) to bottom of the sulcus
- Gingival recession height (GRH) was measured at the mid-buccal aspect of the tooth
- Gingival recession width (GRW) was measured 1 mm apical to the CEJ in a mesio-distal direction
- The width of the keratinized gingiva (KGW), by measuring the distance from the external projection of the base of the pocket to the mucogingival junction (MGJ). The MGJ was determined by using the rollover.
Surgical Technique
All patients were taken up for surgical procedure 3 weeks after Phase-I periodontal therapy.
Preparation of the A-PRF
- 10 ml of venous blood of the patient was obtained. It was then centrifuged at 1500 rpm for 14 minutes. At the end of centrifugation cycle the test tube showed 3 layers. Upper layer was the plasma, middle layer was the fibrous A-PRF clot and the 3rd layer at the bottom was RBC’s.
The surgical procedure was performed under local infiltration of 2% lidocaine combined with 1:100,000 adrenaline.
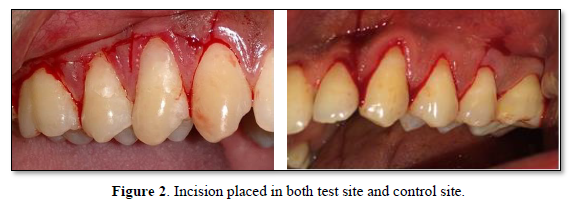
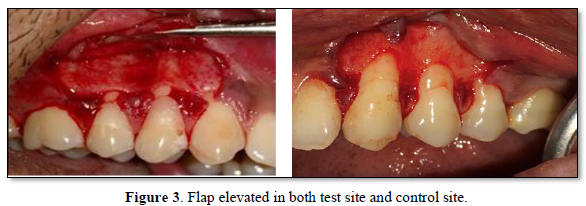
- On the buccal aspect of the tooth involved, intrasulcular incision was made and demarcated by two vertical releasing incisions. A full-thickness flap was reflected using a periosteal elevator till the mucogingival junction. Beyond the mucogingival junction, a split thickness flap was raised. Finally, a full- split thickness flap was elevated which allowed passive coronal positioning of the flap.
- The exposed root surfaces were thoroughly planed using Gracey curettes
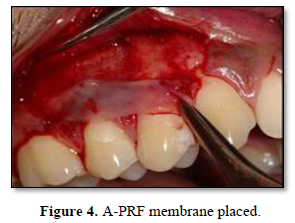
- Patients in the test group received A-PRF over the root surfaces while those in the control group received no further treatment
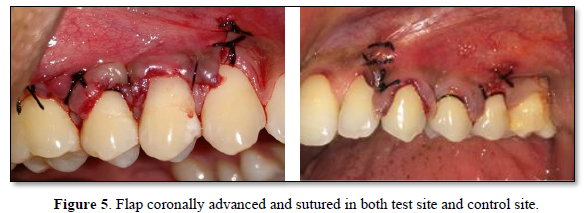
- The elevated flap was coronally advanced to cover the entire root surface
- The flap was stabilized using 4-0 black silk sutures using sling suturing technique
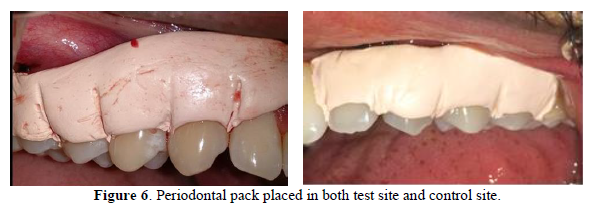
- Periodontal dressing - COE-PACK™ (GC America, Alsip, IL, USA) was placed in the surgical site for a period of 1-week
- All sutures were removed at the time of dressing removal
Post-operative care
The patients of both groups were prescribed analgesics (ibuprofen 400 mg and paracetamol 325 mg combination for 3 days) to control post-operative discomfort. A chlorhexidine mouth rinse was prescribed to the patients and they were instructed to use it twice a day for a period of 14 days. No antibiotics were prescribed to the patients. All patients were put on regular plaque control measures including toothbrushing twice a day with a soft brush.
Routine post-surgical instructions were given. They were instructed to come back to repack the surgical site if a portion of the pack is lost from the operated area. Recall appointments were scheduled after 7 days, 10 days and at 1 and 3 months.
Healing and post-operative follow up
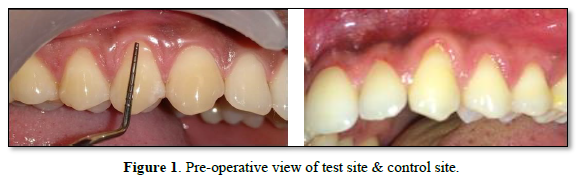
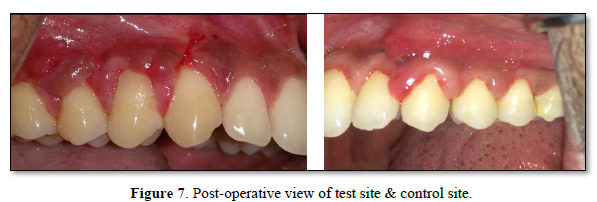
The sutures were removed 7 days after the procedure. The surgical site was examined for uneventful healing. The patients were instructed to continue to use a soft toothbrush for mechanical plaque control in the surgical area by a coronally directed roll technique. Oral hygiene instruction and professional cleaning were provided at each follow-up visit when required (Tables 1-10 & Figures 1-7).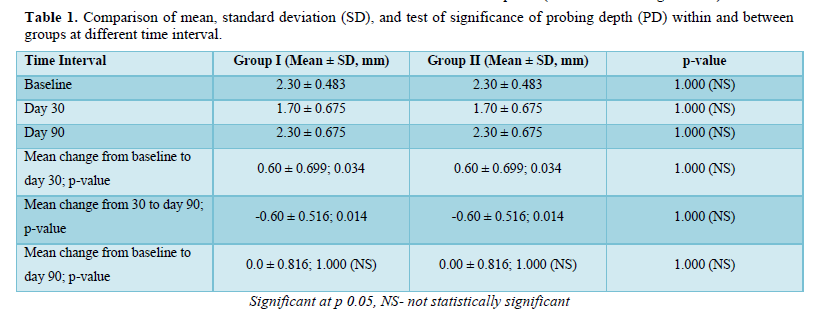
DISCUSSION
This randomized controlled study was performed to evaluate and compare the clinical efficacy of CAF alone and in combination with A-PRF in the treatment of gingival recession defects. Statistically significant results were seen in clinical attachment gain and increase in the width of attached gingiva in the test group (CAF along with A-PRF) when compared to the control group (CAF alone) at the end of 3 months follow-up.
The placement of A-PRF membrane within the recipient site seems to be advantageous. The fibrin matrix possesses mechanical adhesive properties, maintains the flap in a high and stable position, enhances neo angiogenesis, reduces necrosis and shrinkage of the flap thereby bringing about maximal root coverage [6]. The A-PRF membrane also avoids the early invagination of the gingival epithelium, hence serving as a barrier to epithelial migration. There are many advantages of using A-PRF membrane along with CAF. A- PRF does not use bovine thrombin or other exogenous activators in the preparation process. It forms a gel-like matrix that contains high concentrations of non-activated, functional, intact platelets, contained within a fibrin matrix, that release, a relatively constant concentration of growth factors over a period of 7 days [7]. Being autologous in nature, it is relatively inexpensive as no additional cost for synthetic membranes is incurred by the patients. Furthermore, the chair side preparation of A-PRF is quite easy and processing is fast and simple. A recent 6-month study evaluated the use of A-PRF in the treatment of multiple gingival recessions with coronally advanced flap procedure and found significant improvement during the early periodontal healing phase with a thick and stable final remodeled gingiva [8]. However, another randomized clinical trial in the same year reported inferior root coverage of about 80.7% at the test site (CAF+ PRF) as compared to about 91.5% achieved at control site (CAF), but an additional gain in gingival/ mucosal thickness compared to conventional therapy [9]. According to Cairo [10] in his systematic review concluded that the probability of attaining complete root coverage was more when CAF was combined with other adjunctive agents (grafts and biomaterials). Padma [11] in their study found that CAF is a predictable treatment for isolated Miller's class I and II recession defects. The addition of PRF membrane with CAF provides superior root coverage with additional benefits of gain in CAL and WKG at 6 months post-operatively.
This study provides additional data to the growing available evidence demonstrating the efficacy and advantages that A-PRF possesses when used adjunctively to enhance the success of root coverage procedures. This will serve to provide cost effective treatment to patients from all strata of society and ensure that the already successful periodontal therapeutic modalities in management of gingival recession is further enhanced.
CONCLUSION
CAF alone is a highly predictable procedure for the treatment of Miller’s Class II recession defects. However, additional application of A-PRF with CAF provides advantages of earlier healing and quicker attainment of optimal gingival tissue thickness which was maintained throughout the follow-up period due to enriched platelets and growth factors present in the membrane. It can be concluded that the use of A-PRF in conjunction with CAF can prove to be a superior choice for the treatment of Millers class - 11 gingival recession.
- Vinesh K, Pai JBS, Sreedhar A, Malagi S (2017) Amnion allograft in the management of Miller’s Class I gingival recession: A case report. Natl J Integr Res Med 8: 103-105.
- Zucchelli G, Stefanini M, Ganz S, Mazzotti C, Mounssif I, et al. (2016) Coronally advanced flap with different designs in the treatment of gingival recession: A Comparative controlled randomized clinical trial. Int J Periodontics Restorative Dent 36(3): 319-327.
- Allen EP, Miller PD (1989) Jr Coronal positioning of existing gingiva: Short term results in the treatment of shallow marginal tissue recession. J Periodontol 60: 316-319.
- Lee EJ, Meraw SJ, Oh TJ, Giannobile WV, Wang HL (2002) Comparative histologic analysis of coronally advanced flap with and without collagen membrane for root coverage. J Periodontol 73: 779-788.
- Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, et al. (2006) Platelet rich fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101(3): 37-44.
- Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, et al. (2006) Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101: e45-e50.
- Anitua E, Sanchez M, Orive G, Andia I (2007) The potential impact of the preparation rich in growth factors (PRGF) in different medical fields. Biomaterials 28: 4551-4560.
- Corso DM, Sammartino G, Ehrenfest DDM (2009) Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: A 6- month study. J Periodontol 80: 1694-1697.
- Aroca S, Keglevich T, Barbieri B, Gera I, Etienne D (2009) Clinical Evaluation of a Modified Coronally Advanced Flap Alone or in Combination with a Platelet-Rich Fibrin Membrane for the Treatment of Adjacent Multiple Gingival Recessions: A 6-Month Study. J Periodontol 80: 244-252.
- Cairo F, Pagliaro U, Nieri M (2008) Treatment of gingival recession with coronally advanced flap procedures: A systematic review. J Clin Periodontol 35: 136-162.
- Padma R, Shilpa A, Kumar PA, Nagasri M, Kumar C, et al. (2013) A split mouth randomized controlled study to evaluate the adjunctive effect of platelet-rich fibrin to coronally advanced flap in Miller's class-I and II recession defects. J Indian Soc Periodontol 17: 631-6
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Pathology and Toxicology Research
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)










