4000
Views & Citations3000
Likes & Shares
CASE REPORT
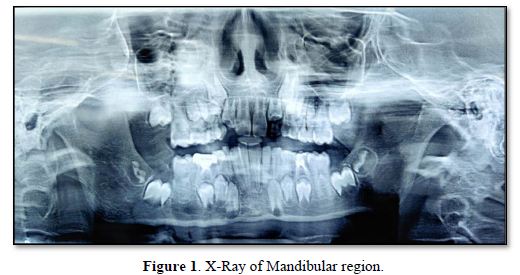
A 8 year old child reported to Bharati Dental College and Hospital with history of painful swelling over right mandibular region since 8 days (Figure 1). On examination an intraoral swelling (2 x 1.5cm) was noted over right mandibular alveolar region extending from distal of permanent first molar to the retromolar area, involving the buccal and lingual cortex & was mixed red and white in color. On palpation, the lesion was soft, smooth surfaced and tender. Incisional biopsy was taken from the lesion under local anesthesia and histopathology report revealed a fibromyxomatous proliferation. Patient was also advised for OPG.
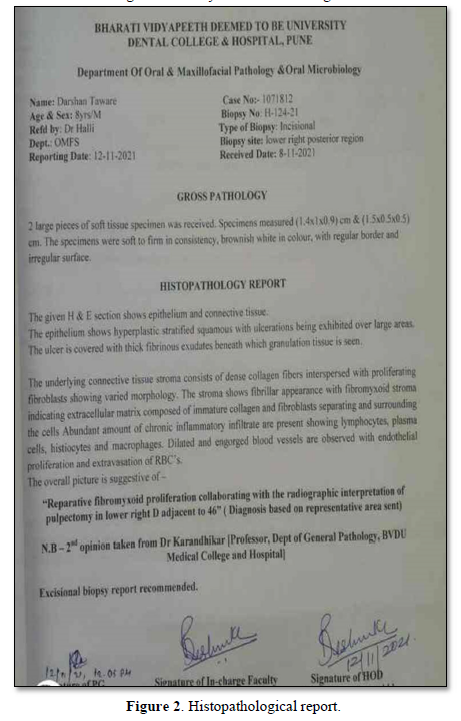
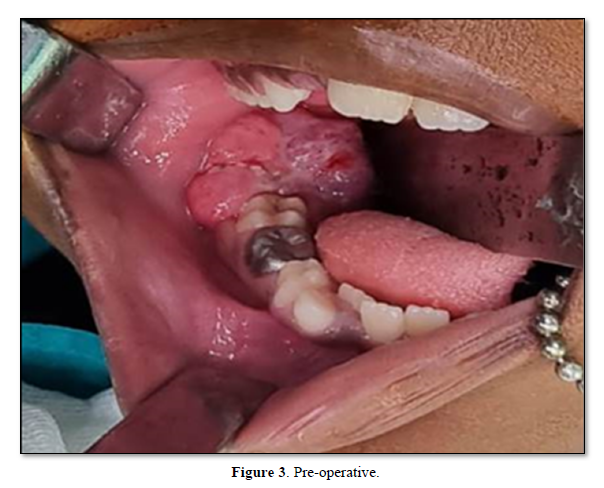
Based on the histopathological report (Figure 2), the patient underwent a wide local excision under general anesthesia and the specimen was subjected to histopathological examination. The size of the lesion had increased to 4x3x2 cm and had become exophytic in nature (Figure 3), meaning that the lesion had undergone some changes after incisional biopsy which prompted to be an aggressive lesion. On histopathological examination of the excisional biopsy specimen, the section showed tissue lined by stratified squamous epithelium, and the subepithelium showed nodules of proliferating cells. Individual cells are spindle shaped with vesicular nuclei, clear to eosinophilic cytoplasm. Background showed fibromyxoid stroma. Mild increase in mitotic activity seen. Few bony spicules & normal salivary gland also noted. The overall picture was suggestive of “reparative fibromyxoid proliferation”.
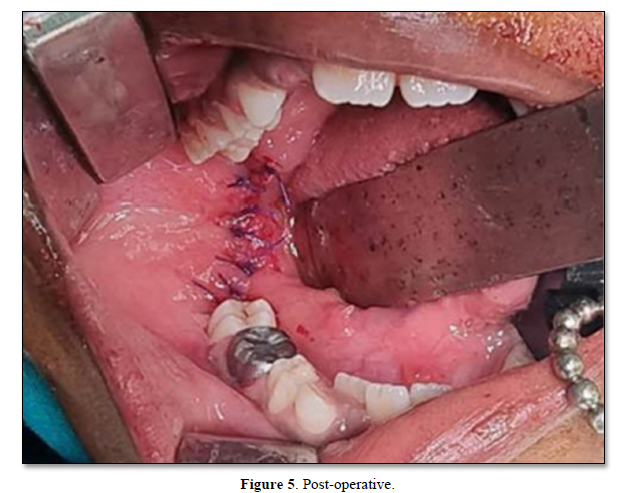
Wide local excision of lesion was done (Figure 4) followed by closure with vicryl 3-0 (Figure 5). The patient showed no signs of recurrence in 10 months follow up.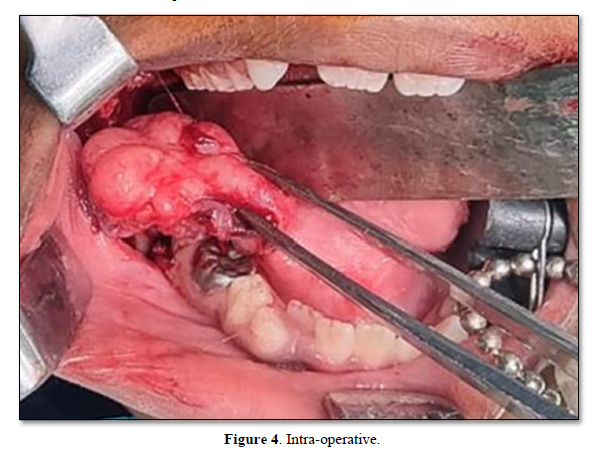
DISCUSSION
While there are no universally accepted treatment recommendations for the management of fibromyxoma, it is important to consider the aggressive nature of this neoplasm in patient management decisions. Although the recommended treatment is usually surgical excision, approaches differ depending on the size of tumor and include conservative surgical excision, enucleation and curettage, curettage with and without electrical or chemical cautery, en bloc resection and wide resection with and without bone grafting. Recurrence rates between 25% and as high as 43% are reported for gnathic fibromyxomas [6]. This is strongly related to the nature of the lesion, presenting without a sheath, thus making the complete removal difficult In some studies, a high rate of recurrence is documented after conservative therapy. This is attributed to the incomplete removal of the lesion rather than the intrinsic biological behavior of the lesion [7]. Due to the tumor’s local aggressive biological behavior and high potential for recurrence, wide surgical resection is recommended. Radiotherapy is generally agreed to be ineffective in the treatment of fibromyxoma [8].
Myxomas/fibromyxomas are usually located intraorally most often in the posterior regions of the mandible, its angle and ramus and rarely extraorally [9]. The maxilla and anterior region of the mandible are rarely affected. The lesion can be diffused or well defined, uni- or multilocular. It is characterized by a mucous or gelatinous grayish-white tissue that replaces the spongy bone and displaces the cortical plates of the jaws. Root displacement and resorption may be present. It may refer to hard and also to soft tissues.
Previous theories stress that the lesion derives from the neural sheath or is the result of degeneration of fibromas, lipomas and so forth, due to the chronic irritation and the degenerative processes following tissue anoxemia. Recent studies advocate that myxomas/fibromyxomas arise from the mesenchymatous tissue of the dental follicle, thus being described as odontogenic with fibroblasts playing the major role in cell dispersal [10]. This explanation fails to describe soft tissue myxomas. They probably arise from supportive structures of the teeth like the gingiva and the periodontal ligament.
CONCLUSION
In conclusion, fibromyxoma is a rare neoplasm. The radiological examination by means of CT and MRI plays an important role in the diagnosis of a fibromyxoma and in the differential diagnosis from other pathological entities such as the ameloblastoma. Its management is surgical and ranges from enucleation and curettage to complete resection and peripheral osteotomy according to its size. Patients must be monitored for at least two years postoperatively in order to diagnose possible recurrence.
CONFLICT OF INTEREST
There is no conflict of interest.
ACKNOWLEDGEMENT
All authors have viewed and agreed to the submission.
PATIENT CONSENT
Patient consent has been obtained for photograph.
- Hajdu SI, Vadmal M (2013) A note from history: Landmarks in history of cancer, Part 6. Cancer. 119(23): 4058-4082.
- Thoma KH, Goldman HM (1947) Central myxoma of the jaw. Am J Orthod Oral Surg 33(7): B532-B540.
- Keszler A, Dominguez FV, Giannunzio G (1995) Myxoma in childhood: an analysis of 10 cases. J Oral Maxillofac Surg 53(5): 518-521.
- Harder F (1978) Myxomas of the jaws. Int J Oral Surg 7(3): 148-155.
- Slootweg PJ, Wittkampf AR (1986) Myxoma of the jaws: an analysis of 15 cases. J Maxillofac Surg 14: 46-52.
- Aquilino RN, Tuji FM, Eid NLM, Molina OF, Joo HY, et al. (2006) Odontogenic myxoma in the maxilla: A case report and characteristics on CT and MR. Oral Oncol Extra 42(4): 133-136.
- Batsakis JG (1987) Myxomas of soft tissues and the facial skeleton. Ann Otol Rhinol Laryngol 96(5): 618-619.
- Ghosh BC, Huvos AG, Gerold FP, Miller TR (1973) Myxoma of the jaw bones. Cancer 31(1): 237-240.
- Simon ENM, Merkx MAW, Vuhahula E, Ngassapa D, Stoelinga PJW (2004) Odontogenicmyxoma: A clinicopathological study of 33 cases. Int J Oral Maxillofac Surg 33(4): 333-337.
- Muzio L, Nocini P, Favia G, Procaccini M, Mignogna MD (1996) Odontogenic myxoma of the jaws: A clinical, radiologic, immunohistochemical, and ultrastructural study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 82(4): 426-433.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)








