4156
Views & Citations3156
Likes & Shares
Abbreviations: BIC: Bone Implant Contact; OD: Osseodensification; CBCT: Cone Beam Computed Tomography
Ridge bone resorption is a typical occurrence in tooth loss areas, and it can occur to varying degrees. Autogenous bone harvesting can greatly increase treatment time and expenses, as well as offer some hazards, such as postoperative discomfort or nerve or artery injury [1-5].
This study will be conducted on 12 patients. Patients having good general health conditions without active periodontal diseases will be considered. Patients having any of the conditions including systemic diseases that influence wound healing like diabetes mellitus and with reduced alveolar bone height less than 4mm will be excluded from the study.
A total number of 12 implants in patients in the above criteria will be included in the study. After clinical and radiographic examinations of maxillary alveolar ridge, alveolar ridge of 6 -8 mm height will be chosen (the minimal accepted height of remaining bone will be 6 mm). Minimum alveolar width should be more than 4 mm. All patients will have preoperative evaluation of alveolar height using Cone Beam Computer Tomography (CBCT) on all four aspects i.e. mesial, distal, buccal and palatal.
Under local anesthesia, a full thickness mucoperiosteal trapezoid flap (with a crestal incision) will be reflected. Full thickness mucoperiosteal flap will be raised on the buccal and palatal aspects of cortical plates with minimal tissue reflection. With a surgical guide (stent), the exact position for the implant will be decided. Pilot drill of 2mm shall be used with length 1mm short than the alveolar height. Densah bur 2mm diameter in Osseodensification mode will be used up to the sinus floor. Densah bur of 3 mm in Osseodensification mode will then be advanced up to 3 mm past sinus floor. Densah burs of 4 mm and 5 mm diameter will then be advanced up to 3 mm past sinus floor, if needed. Then the implant should be placed of desired height of 10mm and adequate diameter according to width of sinus floor. After placing the implant, torque will be measured with torque wrench and values will be noted. Also the changes in the vertical height of the alveolar ridge shall be evaluated using CBCT after 1 day and 4 months.
Inclusion and exclusion criteria
Inclusion criteria:
- Patients with at least one missing tooth in maxillary posterior region.
- Patients having alveolar height of 6 -8 mm and width more than 4mm.
- The recipient bed of the implant should be free from any pathological conditions.
- Patients with no history of diagnosed bone disease or medication known to affect bone metabolism.
- Patients who are cooperative, motivated and hygiene conscious.
- Patient opting for implant placement.
- Patients incapable of undergoing minor oral surgical procedures.
- Patients with insufficient height of alveolar ridge (less than 6mm).
- Patients who have any systemic condition that may contraindicate implant therapy.
- Patients with impractical expectations about the esthetic outcome of implant therapy.
- Patients in the growth stage with mixed dentition.
- Patients with a history of drug abuse.
- Patients with a history of psychiatric disorder.
This study was designed to evaluate the changes in the height of alveolar ridge in 12 implants placed in vertically deficient ridge (H- 6 to 8 mm) performing Indirect Sinus Lift Technique followed by immediate implant placement. Models, orthopantomograph, segmental Cone Beam Computer Tomography (CBCT) were made to estimate the height of remaining bone preoperatively. Indirect Sinus Lift Technique using Osseodensification using Densah Burs was performed and endosteal implants were introduced into the prepared site and evaluated for the primary stability using a torque wrench. The stability of the implant was confirmed by application of 25 Ncm force by the torque wrench. Stability at this value was considered satisfactory for primary stability.
Following implant placement, the patients were directed to a comprehensive CBCT evaluation of the operated area within 24 h. Readings were obtained of the alveolar crestal bone height from the antral floor 4 months after implant placement; similar readings were obtained using the same CBCT machine and maintaining an identical recording methodology. These readings were obtained before exposure for removal of cover screw and placement of the gingival former / healing abutment.
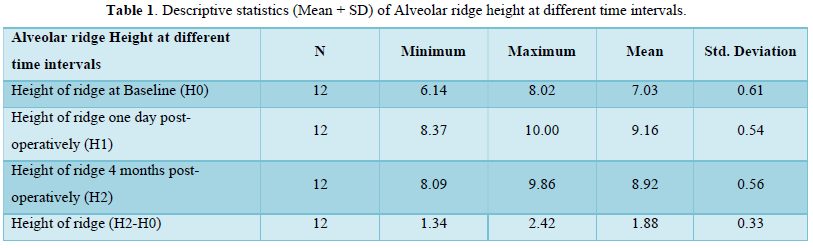
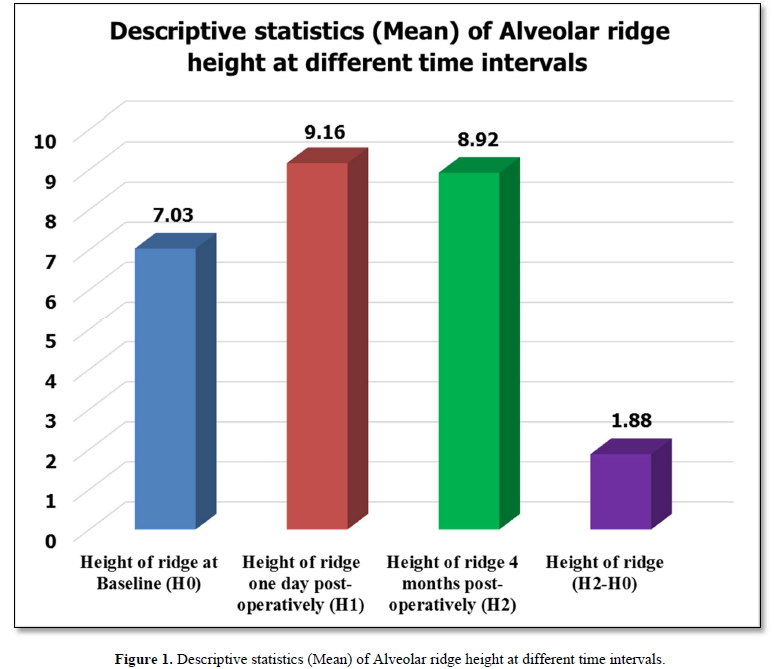
Method of statistical analysis: Data obtained was entered and sorted in Microsoft Excel (v.2013). Statistical analysis was performed using Statistical package for social sciences (SPSS) software (v.21.0). Descriptive statistics was performed for the different parameters assessed in the study. Comparison between different time intervals was performed using Paired t-test. All statistical tests were performed at 95% confidence intervals; keeping p value of less than 0.05 as statistically significant (Table 1, Figure 1 & Table 2).
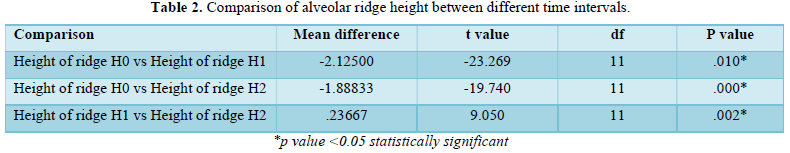
Interpretation: Comparison of alveolar ridge height between different time intervals was done using Paired t-test to assess significant differences. This comparison showed statistically significant differences (p value<0.05) in the alveolar ridge height between the all the time intervals from baseline.
DISCUSSION
By producing a crust of enhanced bone mineral density surrounding the osteotomy site, the osseous densification approach boosts primary stability and the proportion of bone at the implant surface, according to this study. The insertion and removal torques of implants put in osseous densification osteotomies were substantially higher. Despite the fact that osseous densification forces and torques were somewhat higher than drilling, this study showed that this novel osteotomy approach is clinically equivalent to drilling. When irrigation and a bouncing surgical procedure were utilized, there were only minor temperature changes, suggesting that this technique is safe [3].
Compaction of cancellous bone owing to viscoelastic and plastic deformation, as well as compaction autografting of bone particles throughout the length and at the apex of the osteotomy, are two ways that the osseous densification preparation approach retains bone mass. Other osteotomy procedures that compact bone by deformation have been described earlier, and impaction autografting has been utilized to increase the stability of complete hip replacements. The ideology of these approaches contradicts the conclusion of bone drilling, which is that healthy bone should be preserved, especially in areas where density is already low [3].
According to our experience, the formation of osseointegration is influenced by the following factors: 1. the implant material; 2. the implant design; and 3. the implant finish 4. The condition of the bone; 5. Surgical procedure; 6. Implant loading circumstances. The implant should be made of a tissue-tolerant material that can bear the stresses at the insertion site while also being corrosion resistant. Several experts emphasize the need of a precise fit between the bone and the implant. Osseointegration is easier to establish with cylindrical, threaded implants that are implanted such that maximum contact between the implant and the bone is made [4].
Primary stability levels might readily be attained by suitable mechanical engineering and thread design, even if loose instrumentations resulting in healing chambers are used. As a result of this scenario, implants would have excellent primary stability and healing, with little interfacial remodeling early on in the implantation process, while fast bone filling occurs within the healing chambers. This dual stability mechanism should be studied further so that future dental implant systems can achieve temporal stability after implantation, which would be optimal independent of the loading technique used [7].
The osteotome technique, which uses the mechanical action of cylindrical steel tools along the osteotomic walls to compress the bone, is an alternative to implant drilling operations. This treatment resulted in trabecular fractures containing debris, obstructing the osseointegration process. In the case of the osteotome preparation procedure, the healing process is divided into two phases: resorption of broken trabeculae and bone chips followed by new bone growth on the implant surface [8].
The OD approach, which uses specific burs in a noncutting rotation, exhibited the capacity to enhance the percent BV surrounding the implants by roughly 30% and improve secondary implant stability (expressed as removal torque values and micro motion under lateral forces). The histological examination revealed that the healing process is not hampered by the bone condensation, and that bone density is increasing around the implant surface (especially in the upper portion of the implant). Furthermore, the high prevalence of mineralization nuclei bordered by osteoid tissue and osteoblast clearly implies that the bone will continue to grow in density in the long term. The burs studied have a unique shape that allows them to pulverize the bone, resulting in a larger number of mineralization nuclei than the control group. Implants implanted with this innovative OD technique had 30% to 40% greater biomechanical values than implants inserted with traditional drills, according to the study [8].
All volunteers in this study were appropriately evaluated preoperatively using cast models and Cone Beam Computer Tomography. Indirect Sinus Lift Technique using Osseodensification was performed and endosteal implants were introduced into the prepared site. Stability was recorded using a torque wrench. A minimum measurement of 25 Ncm was considered satisfactory for inclusion in the study. Following implant placement, the patients were directed to a second CBCT for evaluation of the operated area 1 day postoperatively. Readings were obtained of the alveolar height from crest to antral floor. Readings of crestal bone changes were obtained once again using the same cone beam computer tomography machine and methodology 4 months after implant placement. All the data obtained was subjected to suitable statistical analysis [15-20].
In this prospective study on twelve patients 12 dental implants were placed in maxillary posterior region. For augmentation of vertically deficient alveolar ridge, we performed Indirect Sinus Lift using Osseodensification Technique using Densah Burs, followed by simultaneous implant placement. No bone grafts were used. For evaluation of increase in height CBCT was taken preoperatively (H0), one day post operatively (H1) and 4 months post operatively (H2) (Table 1). Mean preoperative height was 7.03mm (Range: 6.14 - 8.02 mm), mean alveolar height, from crest to antral floor, one day postoperatively (H1) was 9.16 mm (Range: 8.37 - 10.00 mm) and after 4 months of surgery the height (H2) was 8.92 mm (Range: 8.09 - 9.86 mm). Mean increase in height (H1-H0) was 2.12 mm one day post operatively and mean increase in height (H2-H0) was 1.88 mm after 4 months of surgery. Statistically a highly significant (P value = <0.05) was noted with reference to increase in height of alveolar bone (H0 and H1/H2). This provides evidence of significant increase in alveolar height using Indirect Sinus Lift Technique with help of Osseodensification (Tables 1 & 2) [20-27].
The above data is a sufficient indication of increased height of alveolar bone (measuring from the alveolar crest to the antral floor) using Indirect Sinus Lift Technique with the help of Osseodensification.- Tagliareni JM, Clarkson E (2015) Basic concepts and techniques of dental implants. Dent Clin North Am 59(2): 255-264.
- Beagle JR (2006) The immediate placement of endosseous dental implants in fresh extraction sites. Dent Clin North Am 50(3): 375-376.
- Huwais S, Meyer EG (2017) A Novel Osseous Densification Approach in Implant Osteotomy Preparation to Increase Biomechanical Primary Stability, Bone Mineral Density, and Bone-to-Implant Contact. Int J Oral Maxillofac Implants 32(1): 27-36.
- Albrektsson T, Branemark PI, Hansson HA, Lindstrom J (1981) Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand 52: 155-170.
- Cortes AR, Cortes DN (2010) Non-traumatic bone expansion for immediate dental implant placement: An analysis of 21 cases. Implant Dent 19: 92-97.
- Giro G, Marin C, Granato R, Bonfante EA, Suzuki M, et al. (2011) Effect of drilling technique on the early integration of plateau root form endosteal implants: An experimental study in dogs. J Oral Maxillofac Surg 69: 2158-2163.
- Jimbo R, Tovar N, Anchieta RB, Machado LS, Marin C, et al. (2014) The combined effects of undersized drilling and implant macrogeometry on bone healing around dental implants: An experimental study. Int J Oral Maxillofac Surg 43: 1269-1275.
- Trisi P, Berardini M, Falco A, Vulpiani PM (2016) New osseodensification implant site preparation method to increase bone density in low-density bone. Implant Dent 25: 24-31.
- Laster Z, Rachmiel A, Jensen OT (2005) Alveolar Width Distraction Osteogenesis for Early Implant Placement. J Oral Maxillofac Surg 63: 1724-1730.
- Lahens B, Neiva R, Tovar N, Alifarag AM, Jimbo R, et al. (2016) Biomechanical and histologic basis of osseodensification drilling for endosteal implant placement in low density bone. An experimental study in sheep. J Mech Behav Biomed Mater 63: 56-65.
- de Oliveira PGFP, Bergamo ETP, Neiva R, Bonfante EA, Witek L, et al. (2018) Osseodensification outperforms conventional implant subtractive instrumentation: A study in sheep. Mater Sci Eng C Mater Biol Appl 90: 300-307.
- Pai UY, Rodrigues SJ, Talreja KS, Mundathaje M (2018) Osseodensification - A novel approach in implant dentistry. J Indian Prosthodont Soc 18(3): 196-200.
- Tretto PHW, Fabris V, Cericato GO, Sarkis-Onofre R, Bacchi A (2019) Does the instrument used for the implant site preparation influence the bone-implant interface? A systematic review of clinical and animal studies. Int J Oral Maxillofac Surg 48(1): 97-107.
- Witek L, Neiva R, Alifarag A, Shahraki F, Sayah G, et al. (2019) Absence of Healing Impairment in Osteotomies Prepared via Osseodensification Drilling. Int J Periodontics Restorative Dent 39(1): 65-71.
- Siddiqui AA, Sosovicka M (2006) Lateral bone condensing and expansion for placement of endosseous dental implants: A new technique. J Oral Implantol 32(2): 87-94.
- Tabassum A, Meijer GJ, Walboomers XF, Jansen JA (2014) Evaluation of primary and secondary stability of titanium implants using different surgical techniques. Clin Oral Implants Res 25(4): 487-492.
- Irinakis T, Wiebe C (2009) Initial torque stability of a new bone condensing dental implant. A cohort study of 140 consecutively placed implants. J Oral Implantol 35(6): 277-282.
- Marquezan M, Osório A, Sant'Anna E, Souza MM, Maia L (2012) Does bone mineral density influence the primary stability of dental implants? A systematic review. Clin Oral Implants Res 23(7): 767-774.
- Turkyilmaz I, Aksoy U, McGlumphy EA (2008) Two alternative surgical techniques for enhancing primary implant stability in the posterior maxilla: A clinical study including bone density, insertion torque, and resonance frequency analysis data. Clin Implant Dent Relat Res 10(4): 231-237.
- Inchingolo AD, Inchingolo AM, Bordea IR, Xhajanka E, Romeo DM, et al. (2021) The Effectiveness of Osseodensification Drilling Protocol for Implant Site Osteotomy: A Systematic Review of the Literature and Meta-Analysis. Materials (Basel) 14(5): 1147.
- Padhye NM, Padhye AM, Bhatavadekar NB (2020) Osseodensification - A systematic review and qualitative analysis of published literature. J Oral Biol Craniofac Res 10(1): 375-380.
- Lahens B, Lopez CD, Neiva RF, Bowers MM, Jimbo R, et al. (2019) The effect of osseodensification drilling for endosteal implants with different surface treatments: A study in sheep. J Biomed Mater Res B Appl Biomater 107(3): 615-623.
- Gaikwad AM, Joshi AA, Nadgere JB (2020) Biomechanical and histomorphometric analysis of endosteal implants placed by using the osseodensification technique in animal models: A systematic review and meta-analysis. J Prosthet Dent 127(1): 61-70.
- Tian JH, Neiva R, Coelho PG, Witek L, Tovar NM, et al. (2019) Alveolar Ridge Expansion: Comparison of Osseodensification and Conventional Osteotome Techniques. J Craniofac Surg 30(2): 607-610.
- Bergamo ETP, Zahoui A, Barrera RB, Huwais S, Coelho PG, et al. (2021) Osseodensification effect on implants primary and secondary stability: Multicenter controlled clinical trial. Clin Implant Dent Relat Res 23(3): 317-328.
- Alifarag AM, Lopez CD, Neiva RF, Tovar N, Witek L, et al. (2018) Atemporal osseointegration: Early biomechanical stability through osseodensification. J Orthop Res 36(9): 2516-2523.
- Demetriades N, Il Park J, Laskarides C (2011) Alternative Bone Expansion Technique for Implant Placement in Atrophic Edentulous Maxilla and Mandible. J Oral Implantol 37(4): 463-471.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Journal of Allergy Research (ISSN:2642-326X)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- International Journal of Diabetes (ISSN: 2644-3031)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Pathology and Toxicology Research




