Research Article
Lesser Presence of Negative Emotions in the Elderly During the COVID-19 Outbreak
4549
Views & Citations3549
Likes & Shares
Background: We aimed to assess COVID-19 outbreak-related emotions in older adults, to compare them with those of younger people and, to study the relationship between emotions and practice of regular exercise, loneliness, economic losses and use of anxiolytics within the older adult group.
Methods: We conducted a cross-sectional study starting on March 29 to April 5, 2020 based on a national online survey with a total of 1639 healthy participants.
Results: A lower percentage of people aged ≥60 years experienced any and all negative emotions compared to those 2(1) = 5.09, p= .024, φc = .19), as well as between anxiolytic substance intake and hopelessness (χ2(1) = 4.46, p= .035, φc = .17) and irritability (χ2(1) = 8.19, p= .004, φc = .24). Neither regular exercise nor loneliness have been associated with any of the emotions interviewed (all p> .05).
Conclusion: The knowledge of the lesser presence of negative emotions in older adults might be a starting point to understand the management that this population group has developed during the pandemic to successfully soften the predicted negative emotional impact.
Keywords: COVID-19, Emotions, Exercise, Loneliness, Economic losses, Anxiolytics
INTRODUCTION
The COVID-19 outbreak has become an acute stressor that the whole world's population has been experiencing day by day for more than a year and that has modified our expectations, habits and of course, our emotions.
Emotions constitute individual patterns of expressive behavior, associated with a specific pattern of physiological activation and a specific cognitive-subjective experience or feeling [1]. They communicate intentions, shape behaviors, build mutual trust [2] and also guide thoughts and behaviors [3]. The predominant emotional profile in a large-scale ongoing crisis, such as COVID-19, is associated with the development of coping strategies and psychological management of the event but also tentatively with an exacerbation of mental illness in vulnerable people.
Even though we are all prone to stress in such a pandemic, aging itself has been considered a prominent risk factor for severe disease and death from COVID-19 [4-7], however, research is controversial regarding to the emotional response of older adults with some studies suggesting a risk for the emotional well-being [8] due to fear [9], difficulty in adapting to technologies and isolation [10-11] and, others observing that age was negatively associated with experiencing negative emotions [12] and, positively associated with a better emotional regulation and well-being when compared to younger adults [13]. In line with the above, research has also found that older age is related to less stress reactivity [14-15]. In addition, certain environmental variables have been postulated as risk (isolation, economic losses, use of anxiolytics) and protection factors (regular physical exercise) against emotional distress in older adults [16-20].
Nonetheless, contrary to what was expected, previous studies by our group found that older adults have shown less emotional distress when compared to younger population [21].
Based on this, more emphasis should be given to how older adults are perceiving, internalizing and assimilating the health and social crisis consequences of the pandemic in order to identify what emotions older adults are using to manage the COVID-19 outbreak.
To the best of our knowledge, previous published studies exploring the emotional profile of older adults in the worst moment of the initial outbreak of the pandemic are scarce. Therefore, the aims of the present study are first, to explore the differential presence of emotions among older people during the worst period of COVID-19 outbreak in Spain compared with those experienced by the youngest; and second, to study the relationship between the emotional state of older people and some both protective and risky environmental variables: practicing regular exercise, loneliness, economic losses and use of anxiolytics.
METHODS
Participants and procedure
A total of 150 participants over or equal 60 years old (≥60) (40.7% male) and 1489 under 60 years old (<60) (31.0% male) participants compose this cross-sectional study based on a national online survey (PsyCOVID-SanJuan-imas12) carried out from March 29, 2020, to April 5, 2020, which covers the first peak of the SARS-CoV-2 infection in Spain. The questionnaire was administered applying an exponential non-discriminative snowball sampling. As part of the circulation strategy, the questionnaire was published on the hospital website, advertised in the local media and distributed by social networks to different geographic regions in Spain. For the purposes of the present study, healthcare workers (n = 866) as well as those with current or past mental illness reported (n = 205) were not included as they constitute special vulnerable subgroups [22-25]. Informed consent was provided by all survey participants. The survey was anonymous, and confidentiality of information was assured. The study was approved by the local clinical research ethics committee.
Measures
Sociodemographic information on age, gender and occupation was required in the survey, as well as whether participants presented regular practice of exercise, were experiencing loneliness, understood as the loss of usual accompaniment, were suffering of income loss due to the pandemic situation and/or if they needed to increase consumption of anxiolytic substances.
Following the methodology presented in a previous study by our group [26], participants were presented a list of emotional states (fear, hopelessness, sadness, uncertainty, hypochondria, irritability, intolerance, frustration, anger, and helplessness) and asked to select those that prevailed the most during this phase of the pandemic.
The objective was not to make a list based on a specific instrument, but rather a comprehensive list able to cover the different emotions that could arise in such a unique moment.
The presence/absence of each emotion was compared across groups using the Chi-squared test. P-values below 0.05 were considered statistically significant. The magnitude of the association was measured through Cramer’s phi (φc).
RESULTS
Comparisons of the emotional state between people ≥60 and
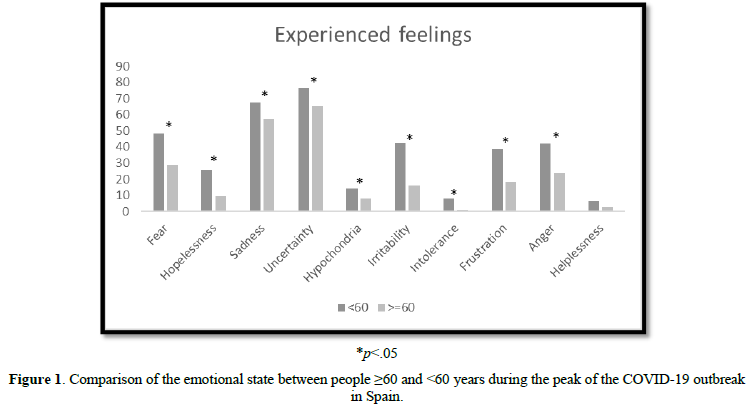
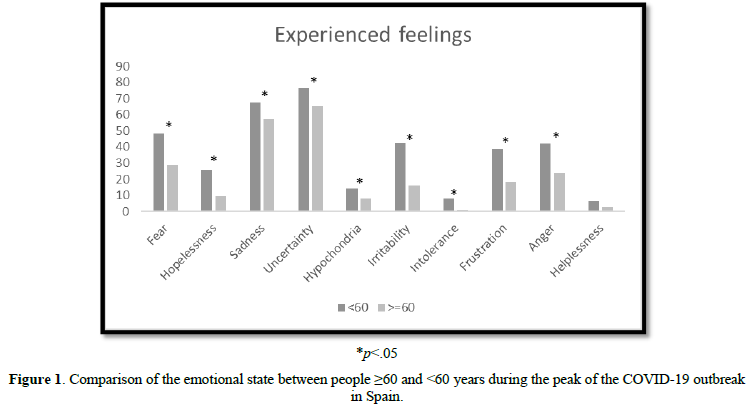
For all negative emotions, percentages were higher in those under 60 years compared to people above 60 years (Figure 1). There was a small but significant association between age and the experience of fear (
Associations between emotional state and physical exercise, loneliness, income loss and anxiolytic substances intake among the older group
The practice of exercise was not associated with the experience of any emotional state within the group of older groups; neither was associated experiencing loneliness with any of the emotions within the older group (all ps> .05). Nonetheless, having suffered of income loss appeared positively associated with anger (χ2(1) = 5.09, p= .024, φc = .19). Specifically, only those who suffer from income loss experienced anger (18%). Lastly, anxiolytic substance intake was associated with hopelessness (χ2(1) = 4.46, p= .035, φc = .17) and irritability (χ2(1) = 8.19, p= .004, φc = .24). Specifically, an increase in anxiolytic intake was observed in all those feeling hopelessness (8%) or irritability (13%).
DISCUSSION
The COVID-19 pandemic has become a unique stressor with a worldwide impact, leading some media to begin to compare it with the devastating 1918 Spanish flu. Research has confirmed that the greatest increase in mortality risk has been observed in patients over 60 years in all affected countries [27], especially in the initial moment. In addition, older adults have shown more severe complications, disruptions in daily routines and access to care and isolation during the pandemic [28]. Notwithstanding, studies from different countries have shown that despite the greater somatic vulnerability, the emotional consequences have not been as severe as expected compared to the younger population, at least during the first and so far, the worst peak of the COVID-19 pandemic [28-29]. Thus, the purpose of this study was to explore the feelings and predominant negative emotions presented at the highest peak of the pandemic in Spain in order to disentangle if those experienced differ between people over and under 60 years old; and if some explored environmental variables could be partly related to these emotions. Overall, the results obtained indicate that a smaller proportion of older adults have experienced negative emotions when compared to the younger during the first peak of COVID-19 in Spain.
These results are consistent with the lower rates of anxiety, depression and acute stress previously reported in older adults by our group [21] and also other research groups [30] in Spain, as well as in other countries [31-32]. Moreover, evidence suggests that older adults as a group may be more resilient to the adverse effects from the pandemic, and it is noteworthy that emotions may have played a fundamental role. Emotions are conceived as responses to appraisals or interpretations of events [33] that elicit and coordinate changes in cognition, behavior and subjective experience [34-35]. Therefore, the lower proportion of all negative emotions experienced by older people reported in this study may partially explain why the emotional impact, contrary to what was expected at the beginning of the pandemic, has been lower in this age group compared to younger people, which could be partially explained by biological factors, such as the lower reactivity to stress previously described [14-15], but could also reflect a greater resilience.
Some external aspects such as low risk perception [36], less exposure to the stressors of COVID-19, financial stability or social status could explain part of this greater resilience observed in old age [37], but there are undoubtedly other internal factors inherent to this population group that might justify why the response to stress generated by COVID-19 has awakened fewer negative emotions. Those over 60 years of age in Spain have grown up in the period of time that follows the Spanish civil war and may have developed strategies for managing adversity. In addition, the greater awareness of risk described in older people might have allowed them to implement proactive precautionary measures [38] that have undoubtedly contributed to increasing the feeling of security. Moreover, wisdom, a complex personality trait including empathy and compassion, emotional regulation, the ability to self-reflect, decisiveness while accepting uncertainty and diversity of perspectives, social advising, and spirituality [28] has been pointed out as a determinant of better response capacity to the pandemic of older compared to younger adults [39].
Our secondary objective was to assess whether the emotions experienced by older people were related to the presence of loneliness, regular practice of exercise, income loss and increased consumption of anxiolytic substances, which are the environmental variables that in a previous study by our group were associated with an increase in acute stress symptoms, anxiety and depression in older adults [21]. No associations have been found between any of the negative emotions explored in this study and regular practice of exercise nor loneliness. The former may be explained by exercise having been found to be a protective factor against the emotional impact of the COVID-19 [40]; and the latter, due to older people seeming to have prioritized quality over quantity of social interactions during the lockdown [41]. On the other hand, anger appeared related to economic losses; and both hopelessness and irritability were associated with an increase in the use of anxiolytics.
Results of this study should be interpreted in the light of some limitations and strengths. First, response bias exists given the voluntary nature of the online self-administered survey applied. Second, the list of selected emotions constitutes a mixture of basic and complex emotions chosen to provide ecological validity to the study; thus, not adhering to previously defined structured interview. Third, the survey was carried out during confinement, when perhaps due to the existing limitations to exercise, the expected negative relationship between physical activity and the emotions collected has been attenuated. And finally, positive feelings of altruism, responsibility and care in the face of COVID-19 regarding social interdependence that might have emerged [42] were not included. Strengths include data collection from a wide population sample, in real time, at the maximum peak of the pandemic avoiding memory-related biases.
The knowledge of the lesser presence of negative emotions in older adults alongside with the identification of some related environmental factors is crucial to figure out why, despite the seriousness and lethality of SARS-CoV-2 in this age group, the emotional consequences have been mild. A better understanding of the emotional response older adults had developed in response to the pandemic could be useful to identify vulnerable groups and to design more efficient preventive therapies or counselling approaches to ameliorate the psychological impact of the pandemic. Additional longitudinal studies are needed to verify if these apparently positive early findings are maintained over time and if they can be applied to older adults from other backgrounds.
AUTHOR CONTRIBUTIONS
LGF and RRJ have taken charge of the conceptualization and methodology. VRF has carried out the data curation and formal analysis. LGF has written the original draft and RRJ, VRF, VR and GL have reviewed the final version.
CONFLICT OF INTEREST
Dr. R. Rodriguez-Jimenez has been a consultant for, spoken in activities of, or received grants from: Instituto de Salud Carlos III, Fondo de Investigación Sanitaria (FIS), Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM), Madrid Regional Government (S2010/ BMD-2422 AGES; S2017/BMD-3740), JanssenCilag, Lundbeck, Otsuka, Pfizer, Ferrer, Juste, Takeda, Exeltis, Angelini, Casen-Recordati. Dr. Lahera has been a consultant to or has received honoraria or grants from Janssen-Cilag, Otsuka-Lundbeck, Lilly, Astra-Zeneca, CIBERSAM and Instituto de Salud Carlos III. All other authors declare that they have no conflict of interest.
FUNDING STATEMENT
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
ACKNOWLEDGEMENT
- We thank all participants who have kindly responded to the survey.
- This study has been carried out in Spain.
- This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
- Piqueras JA, Martínez A, Ramos V (2006) Ansiedad, depresión y salud, in L. Oblitas (Ed.), Psicología de la Salud y Enfermedades Crónicas, Bogotá. PSICOM Editores 15(1): 43-74.
- Chapman GB, Coups EJ (2006) Emotions and preventive health behavior: Worry, regret, and influenza vaccination. Health Psychol 25(1): 82-90.
- Trampe D, Quoidbach J, Taquet, M (2015) Emotions in Everyday Life. PloS One 10: 12.
- Chen Y, Klein SL, Garibaldi BT, Li H, Wu C, et al. (2021) Aging in COVID-19: Vulnerability, immunity and intervention. Ageing Res Rev 65: 101205.
- Perrotta F, Corbi G, Mazzeo G, Boccia M, Aronne L, et al. (2020) COVID-19 and the elderly: Insights into pathogenesis and clinical decision-making. Aging Clin Exp Res 32(8): 1599-1608.
- Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, et al. (2020) Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiat 0366(20): 1-14.
- Zhao W, Jian W, Li H (2020) Preventing and Controlling Measures of 2019 Coronavirus Disease (COVID-19): Practice in Psychogeriatric Ward. Am J Geriatr Psychiatry 28(7): 786-787.
- Mowla A, Ghaedsharaf M, Pani A (2021) Psychopathology in Elderly COVID-19 Survivors and Controls [published online ahead of print, 2021 Mar 22]. J Geriatr Psychiatry Neurol 8919887211002664.
- Gokseven Y, Ozturk GZ, Karadeniz E, Sarı E, Tas BG, et al. (2021) The Fear of COVID-19 Infection in Older People [published online ahead of print, 2021 Mar 22]. J Geriatr Psychiatry Neurol 8919887211002651.
- Gerst-Emerson K, Jayawardhana J (2015) Loneliness as a public health issue: The impact of loneliness on health care utilization among older adults. Am J Public Health 105(5): 1013-1019.
- Santini Z, Jose P, Cornwell E (2020) Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 5: e62-e70.
- Carstensen LL Shavit YZ, Barnes JT (2020) Age Advantages in Emotional Experience Persist Even Under Threat From the COVID-19 Pandemic. Psychol Sci 31(11): 1374-1385.
- Lee, EE, Depp C, Palmer BW, Glorioso D, Daly R, et al. (2019) High prevalence and adverse health effects of loneliness in community-dwelling adults across the lifespan: Role of wisdom as a protective factor. Int Psychogeriatr 31(10): 1447-1462.
- Klaiber P, Wen JH, DeLongis A, Sin NL (2021) The Ups and Downs of Daily Life During COVID-19: Age Differences in Affect, Stress, and Positive Events. J Gerontol B Psychol Sci Soc Sci 76(2): e30-e37.
- Nelson NA, Bergeman CS (2021) Daily Stress Processes in a Pandemic: The Effects of Worry, Age, and Affect. Gerontologist 61(2): 196-204.
- Richard A, Rohrmann S, Vandeleur CL, Schmid M, Barth J, et al. (2017) Loneliness is adversely associated with physical and mental health and lifestyle factors: Results from a Swiss national survey. PLoS One 12(7): e0181442.
- de Oliveira LDSSCB, Souza EC, Rodrigues RAS, Fett CA, Piva AB (2019) The effects of physical activity on anxiety, depression, and quality of life in elderly people living in the community. Trend Psychiat Psychother 41(1): 36-42.
- Flint AJ, Bingham KS, Iaboni A (2020) Effect of COVID-19 on the mental health care of older people in Canada. Int Psychogeriatr 32(10): 1113-1116.
- Robinson J, Sareen J, Cox BJ, Balton J (2009) Self-medication of anxiety disorders with alcohol and drugs: Results from a nationally representative sample. J Anxiety Disord 23(1): 38-45.
- Voyer P, Cappeliez P, Pérodeau G, Préville M (2005) Mental health for older adults and benzodiazpine use. J Community Health Nurs 22(4): 213-229.
- García-Fernández L, Romero-Ferreiro V, López-Roldán PD, Padilla S, Rodriguez-Jimenez R (2020) Mental Health in Elderly Spanish People in Times of COVID-19 Outbreak. Am J Geriatr Psychiatry 28(10): 1040-1045.
- Yao H, Chen J-H, Xu Y-F (2020) Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiat 7: e21.
- García-Fernández L, Romero-Ferreiro V, Padilla S, López-Roldán PD, Monzó-García M, et al. (2021) The impact on mental health patients of COVID-19 outbreak in Spain. J Psychiatr Res 136: 127-131.
- Lai J, Ma S, Wang Y (2019) Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 3: e203976.
- García-Fernández L, Romero-Ferreiro V, López-Roldán PD, Padilla S, Calero-Sierra I, et al. (2020) Mental health impact of COVID-19 pandemic on Spanish healthcare workers. Psychol Med 27: 1-3.
- García-Fernández L, Romero-Ferreiro V, Padilla S, Lahera G, Rodriguez-Jimenez R (2021) Different emotional profile of health care staff and general population during the COVID-19 outbreak [published online ahead of print, 2021 Mar 4]. Psychol Trauma 10.1037/tra0001024.
- Bonanad C, García-Blas S, Tarazona-Santabalbina F, Sanchis J, Bertomeu-González V, et al. (2020) The Effect of Age on Mortality in Patients with COVID-19: A Meta-Analysis With 611,583 Subjects. J Am Med Dir Assoc 21(7): 915-918.
- Vahia IV, Jeste DV, Reynolds CF (2020) Older Adults and the Mental Health Effects of COVID-19. JAMA 324(22): 2253-2254.
- Hophing M, Zimmerman-Winslow KJ, Basu A, Jacob T (2021) The Impact of COVID-19 and Quarantine on Suicidality in Geriatric Inpatients-A Case Report [published online ahead of print, 2021 Jun 10]. J Geriatr Psychiatry Neurol.
- González-Sanguino C, Ausín B, Castellanos MA (2020) Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun 87: 172-176.
- Czeisler ME, Lane RI, Petrosky E, Wiley JF, Christensen A, et al. (2020) Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep 69(32): 1049-1057.
- Klaiber P, Wen JH, DeLongis A, Sin NL (2021) The Ups and Downs of Daily Life During COVID-19: Age Differences in Affect, Stress, and Positive Events. J Gerontol B Psychol Sci Soc Sci 76(2): e30-e37.
- Roseman IJ (2013) Appraisal in the Emotion System: Coherence in Strategies for Coping. Emot Rev 5(2): 141-149.
- Izard CE, Woodburn EM, Finlon KJ, Krauthamer-Ewing ES, Grossman SR, et al. (2011) Emotion Knowledge, Emotion Utilization, and Emotion Regulation. Emot Rev 3(1): 44-52.
- Rowe AD, Fitness J (2018) Understanding the Role of Negative Emotions in Adult Learning and Achievement: A Social Functional Perspective. Behav Sci (Basel) 8(2): 27.
- Bruine de Bruin W (2021) Age Differences in COVID-19 Risk Perceptions and Mental Health: Evidence from a National U.S. Survey Conducted in March 2020. J Gerontol B Psychol Sci Soc Sci 76(2): e24-e29.
- Laird KT, Krause B, Funes C, Lavretsky H (2019) Psychobiological factors of resilience and depression in late life. Transl Psychiatry 9(1): 1-18.
- Pearman A, Hughes ML, Smith EL, Neupert SD (2021) Age Differences in Risk and Resilience Factors in COVID-19-Related Stress. J Gerontol B Psychol Sci Soc Sci 76(2): e38-e44.
- Jeste DV, Di Somma S, Lee EE, Nguyen TT, Scalcione M, et al. (2020) Study of loneliness and wisdom in 482 middle-aged and oldest-old adults: a comparison between people in Cilento, Italy and San Diego, USA. Aging Ment Health 25(11): 2149-2159.
- Zhang Y, Zhang H, Ma X, Di Q (2020) Mental Health Problems during the COVID-19 Pandemics and the Mitigation Effects of Exercise: A Longitudinal Study of College Students in China. Int J Environ Res Public Health 17(10): 3722.
- van Tilburg TG, Steinmetz S, Stolte E, van der Roest H, de Vries DH (2020) Loneliness and mental health during the COVID-19 pandemic: A study among Dutch older adults. J Gerontol B Psychol Sci Soc Sci 76(7): e249-e255.
- Johnson MC, Saletti-Cuesta L, Tumas N (2020) Emociones, preocupaciones y reflexiones frente a la pandemia del COVID-19 en Argentina [Emotions, concerns and reflections regarding the COVID-19 pandemic in Argentina]. Cienc Saude Coletiva 25(suppl 1): 2447-2456.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Pathology and Toxicology Research
- BioMed Research Journal (ISSN:2578-8892)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)



