Research Article
Activities of Daily Living and Perceived Stress of Indian Population during the COVID-19 Pandemic
4636
Views & Citations3636
Likes & Shares
Background: The people were enforced to stay back at home and restricted personal, social and economical activities worldwide after outbreak of COVID-19 pandemic. Restrictions in activities of daily life have impact physical and mental health of the people.
Aim: To explore impact on activities of daily living and perceived stress in Indian population during the COVID-19 Pandemic.
Method and Materials: The present survey was online cross-sectional study among Indian population during the COVID-19 pandemic. We received total of 914 responses in the stipulated time. The participants who agreed for virtual consent were diverted for the further study. Socio-demographic datasheet, a 6-items self-designed questionnaire on Activities of Daily Living, Perceived Stress Scale was included in the Google Form.
Results: Findings of this study revealed 5.3% of perceived stress in Indian population. Activities of daily life influenced such as using mobile for more than 2 hours, decreased desire of shopping 46.4%, incapable of handling money (16%), engaged in food preparation (74.8%), laundry (79.4%), Often perform daily housekeeping (51.9%) during the lockdown of COVID-19 pandemic.
Conclusion: The present study shows the activities of daily life and perceived stress are directly affected to mental health problem in COVID-19 pandemic. Specially, people who work in private sector and daily wages were suffering with low income, job security and require of daily living things, those are led to high level of stress and other health issues.
Keywords: Stress, Activities of Daily Living, Indian population, COVID-19 pandemic
INTRODUCTION
The COVID-19 pandemic has affected on mankind in different ways like health, day to day life, trades, economy, etc. This impact has been observed worldwide in which countries enforced lockdown, social distancing, and strict quarantine to flatten the curve of the corona virus infection. Restriction in the day-to-day movements has affected activities of daily life. People have been facing problems related to healthcare, economy and social life [1-3]. On March 25, 2020, lockdown was declared by the Prime Minister of India in the whole country for next 21 days [4]. In India, lockdown measures similar to other countries included travel bans, stay at home, the mandatory closure of schools, social distancing, nonessential commercial activities and other mass participation events. Other countries in the world have also taken similar or even stricter measures to stop community spread of COVID-19. The total number of confirmed cases worldwide is more than 20439814, with more than 2396637 cases in India alone [5].
The combined effect of changes in lifestyle behaviors; confinement to the home through government restrictions in travel; and elevated depression, anxiety and stress associated with the current COVID-19 pandemic, may have significant negative impacts on sleep [6]. Those people in self-isolation and stay at home, they are restricted of maintaining contact with loved ones, their daily life routines are dramatically changed, and people normally engage in everyday activities impact their health and well-being [7]. In India, the work in an urban areas informal economy is alternating, during COVID-19 pandemic marked by low-skill requirements, low wages, severe struggle, and regular job insecurity [8]. COVID-19 pandemic is especially relevant for those people in self-isolation or quarantine, where facing of income issues, psychological distress, depression, anxiety fear, and anger may manifest [9]. The pandemic threatened the existence of the individuals to a great extent, worry, sleep disturbances and affected their mental status negatively [10]. The public are returning to work after the concern about virus exposure, they worry about delays in work time and subsequent deprivation of their anticipated income explains the high-stress level [11]. The people were facing a pandemic with no vaccination would result in fear of the unknown making them anxious and stressed. Keeping in mind the concerns regarding psychological distress raised in their around [12]. There is need to see the how people are managing their lives during the enforced lockdown after outbreak of COVID-19 pandemic. Our study aimed to study the impact of COVID-19 pandemic on activities of daily living and perceived stress in Indian population.
MATERIALS AND METHODS
The present study was a cross-sectional online survey conducted through Google Forms web survey platform. The Google Forms link of the questionnaire was sent through WhatsApp and other social media to the contacts of the participations. Google Forms offers the advantage of submitting the response when maintaining secrecy. Participants were assured that their responses would be kept confidential and utilized only for the research. The survey started to be applied on April 25, 07:13 h, and ended on May 26, 09:48 h (IST). The survey link clearly stated that the participants can draw their participation back at any time before submission of his/ her response and also, they will be provided an informed consent. The survey could reach up to 24 states of India. A total of 914 Indian subjects have completed this online survey by the predetermined time and sample. The study was approved by the Ethics Review Board of Central India Institute of Mental Health and Neurosciences, Rajnandgoan, Chhattisgarh, before the start of collecting data. Participants of both the genders, aged between 18 to 65 years, able to read and understand Hindi and English language, participants with online informed consent were included.
Tools used
Socio-demographic datasheet: The socio-demographic datasheet was developed for the present study consisted of variables like age, sex, education, occupation, family types, etc.
Activities of daily living: A 6-items self-designed questionnaire was used for the purpose of the study. Activities of daily living included mobile use, shopping, food preparation, housekeeping, laundry, and finance. The questionnaire included questions about on activities of daily living life impact of COVID-19 pandemic on the general population.
Perceived Stress Scale (PSS) [13]: The PSS is the most widely used psychological instrument for measuring the perception of stress during the last month. It is a measure of the degree to which situations in one’s life are appraised as stressful. The scale had 10 items and each item provides five response options: never, almost never, sometimes, fairly often, and very often. Items n. 1, 2, 3, 6, 9 and 10 are scored from 0 to 4; items n. 4, 5, 7 and 8 are scored reversely, from 4 to 0. The scores range between 0 and 40. Higher score indicated that high perceived stress.
DATA ANALYSIS
The statistical analysis was done using Statistical Packages for the Social Science (SPSS)-16 software package for windows. For socio-demographic variables, descriptive statistics were used such as frequency, percentage, mean, and standard deviation (SD).
RESULTS
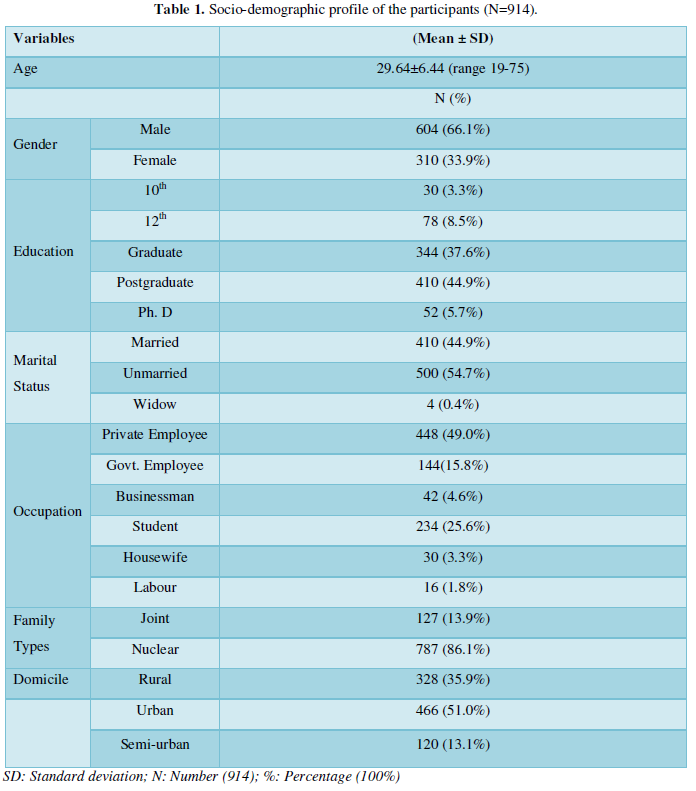
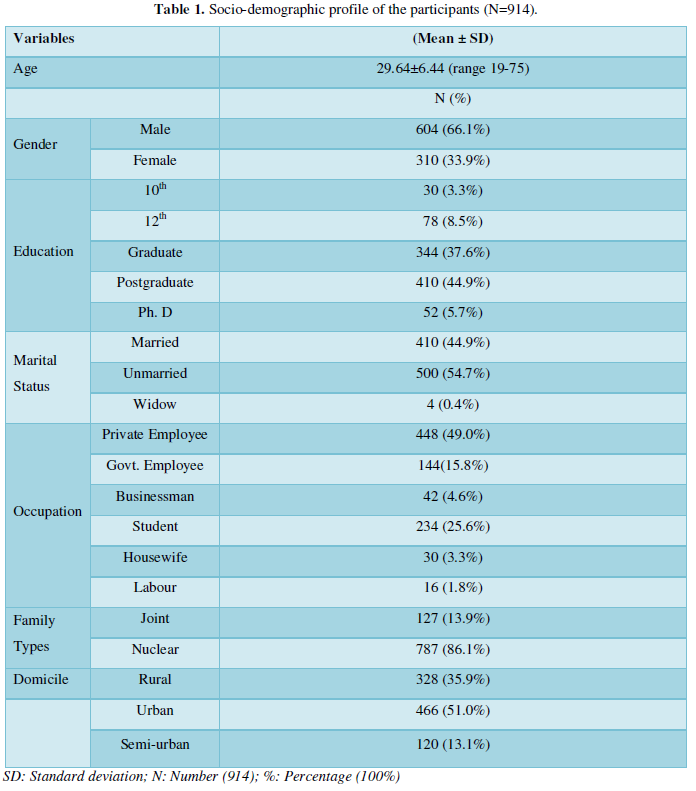
Table 1 reveals the socio-demographic details of the participants. The mean and SD score of hospital staff was 29.64±6.44 with age range between 18-75 years. More than half (66.1%) of the participants were male, majority (44.9%) of the participants had completed post-graduate education, maximum (49.0%) of them were working in private sectors. Most (86.1%) of the participants belonged to nuclear family. More than half (51.0%) of the participants were belonging to urban areas.
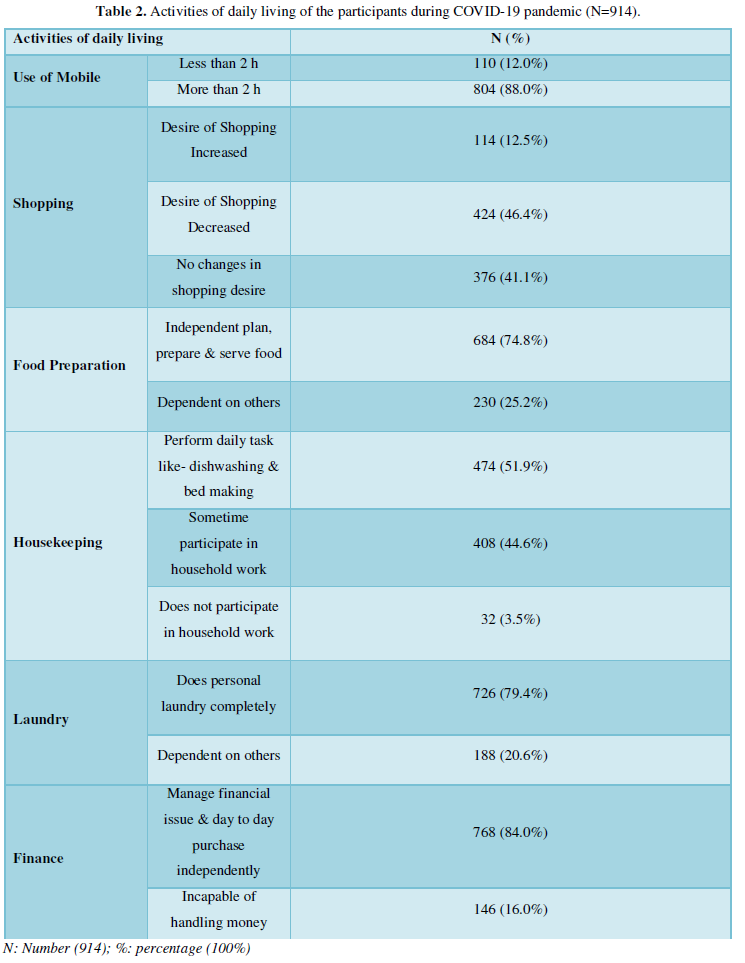
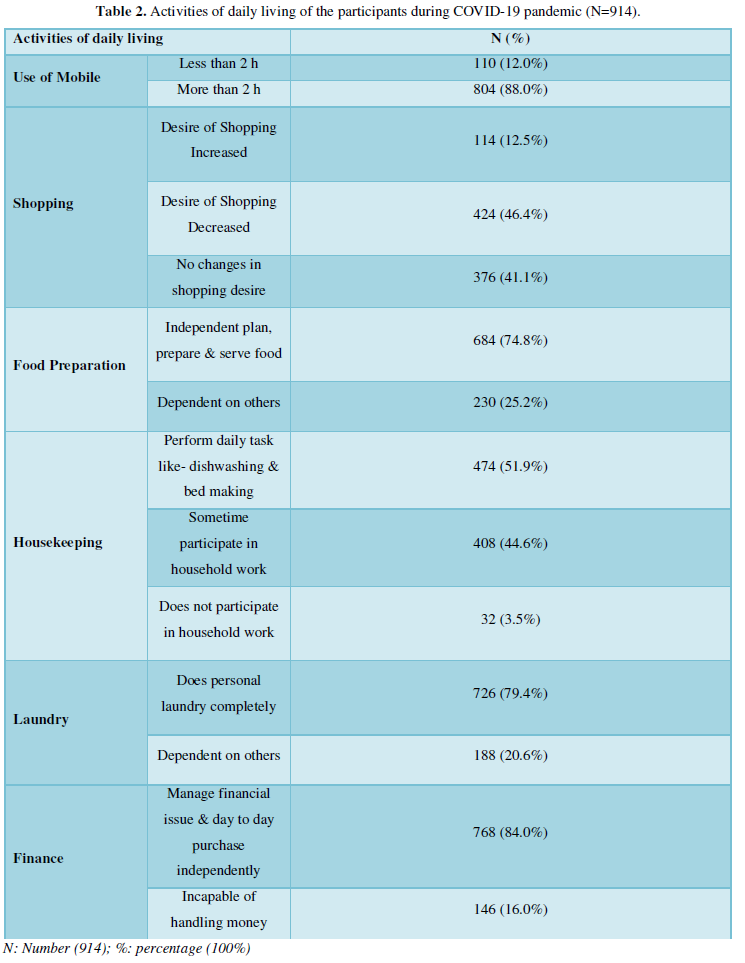
Table 2 shows that activities of daily living of the respondents in during the lockdown of COVID-19 pandemic. The most of 88.0 % participants were used mobile more than one hour. Almost half 46.4% reporting desire of shopping was decreased. Majority of 74.8 % Participants ware independent plan, prepare and serve food at home. Most of half 51.9 % reporting that they were performed daily task like- dishwashing and bed making and other household work. Participants were 79.4 % doing personal laundry work. Participants reported that16.0 % was incapable of handling money and financial issues during the lockdown of COVID-19 pandemic.
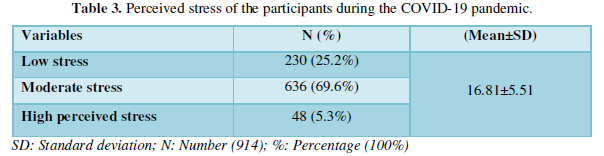
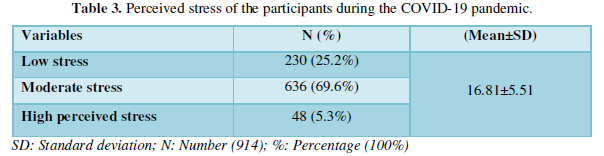
Table 3 reports that the mean and SD score of stress in general population were 16.81±5.51 and this table also reports the prevalence of perceived stress during the lockdown of COVID-19 pandemic in general population based on perceived stress scale scores at high perceived stress level. The results showed 25.2% of low stress, 69.6% of moderate stress and 5.3% of high perceived stress during the lockdown of COVID-19 pandemic in general population.
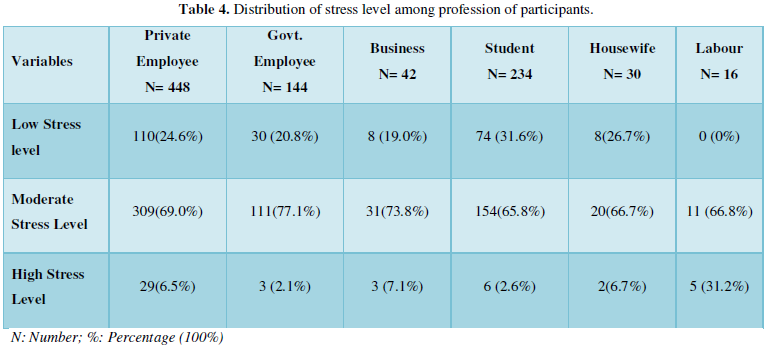
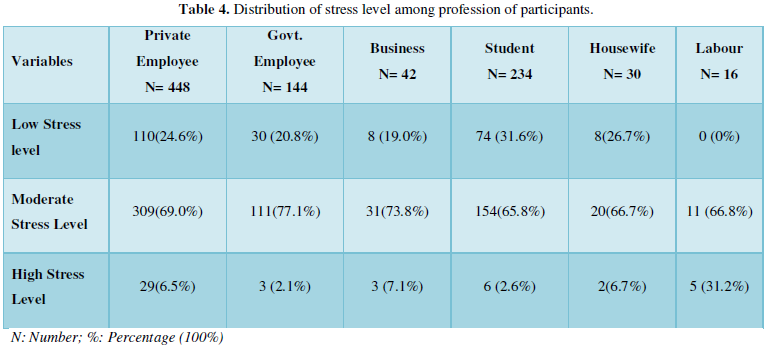
Table 4 shows the prevalence of perceived stress level on the profession. On stress level were found to be 69.0% moderate level and 6.5% high level of stress in private employees, 77.1% moderate level and 2.1% high level of stress in government employees, 73.8% moderate level and 7.1% high level of stress in businessman, 65.8% moderate level and 2.6% high level of stress in student, 66.7% moderate level and 6.7% high level of stress in house wife and 66.8% moderate level and 31.2% high level of stress in labor. The table shows among different professions, labor, private employees, businessman and housewife were found perceived high level of stress.
DISCUSSION
The present study found 88.0 % participants were used mobile more than two-hour, 46.4% reporting desire of shopping was decreased, 74.8% Participants ware independent plan, prepare and serve food at home, 51.9 % reporting that performed daily task like- dishwashing and bed making and other household work, 79.4 % doing personal laundry work, 16.0 % was incapable of handling money and financial issues during the lockdown of COVID-19 pandemic. Some similar study supported it; majority of the people were worried about the financial loss they were incurring during the period of lockdown [10]. The restriction of mobility can act as a difficulty in obtaining daily-life necessary supplies, potential financial losses, and access to conflicting and inadequate information on the Internet [14,15]. The COVID-19 outbreak has led to diversified mental health responses depending on the individual’s strengths and weaknesses [16]. People were affected on physical activity, their work and income during COVID-19 pandemic [17]. People are restricted of maintaining contact with loved ones, their daily routines are dramatically changed, and engage in everyday activities impact their health and well-being [6].
The present study has also found that 25.2% of low stress, 69.6% of moderate stress and 5.3% of high perceived stress during the lockdown of COVID-19 pandemic in general population. Result also found that higher level of the stress has in labour (31.2%), private employees (6.5%), businessman (7.1%) and housewife (6.7%). Some similar study supported it, high rates of anxiety, insomnia, perceived stress and adjustment outcomes found during the lockdown of COVID-19 in the Italian of general population [18]. The psychosocial stress was perceived, and participants presented high levels of perceived distress in the general population [14]. This could be associated with high levels of anxiety and stress because of isolation, indicating adverse mental health [19]. The mental health impact on the non-infected community, revealing significant psychiatric morbidities during the SARS outbreak [20]. Those people in self-isolation or quarantine, where feelings of stress, anxiety, depression, fear, guilt, and anger may manifest [6]. People had trauma-related distress symptoms and significantly higher psychological distress in women and young adult population [21]. Among different professions, students and healthcare professionals were found to suffering from stress, anxiety, and depression more than others and normal ranges found in mental health professionals [22].
LIMITATIONS
The present study has some limitations; the size of the sample in some profession groups was quite small. Accidental sampling technique was used in the present study. Activity of daily living assessment was self-report. The longitudinal study may help to see long term effects of COVID-19 pandemic on job stress, job satisfaction, family conflicts and suicide ideation.
IMPLICATIONS
The present admits that the general population is vulnerable to experience problems related to activities of daily living life and perceived stress while living in pandemic situation at home. The mental health professionals, policy makers and government can take step to secure physical and mental health of general population to impart effective in their daily life. They have to need stress management programs, online counseling facilities, adequate manpower supply, etc. for reduce their perceive stress and improve daily living life.
CONCLUSION
The present study reveals activities of daily living and perceived stress are consequence mental health problems among Indian population during outbreak of the COVID-19 pandemic. The people experienced isolation, loss of social network, risk or infections to family members, decreased income, physical exhaustion, job insecurity and livelihood concerns. The uncertainty was in each age group about future as school, retail shops, entertainment sector remained closed. A great loss to the unorganized sector, private sector caused problems to the young adults.
- Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, et al. (2020) A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res 7(1): 4.
- Haleem A, Javaid M, Vaishya R (2020) Effects of COVID 19 pandemic in daily life. Curr Med Res Pract 10(2): 78-79.
- Pietrobelli A, Pecoraro L, Ferruzzi A, Heo M, Faith M, et al. (2020) Effects of COVID‐19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: A longitudinal study. Obesity (Silver Spring) 28(8): 1382-1385.
- India Lockdown Live Updates: PM Modi Announces 21‑day Complete Lockdown from Midnight Tonight. Times India. Available online at: https://timesofindia.indiatimes.com/india/coronavirus-in-india-live-updates-pm-modi-to-address-the-nation/liveblog/74783769.cms
- World Health Organization (WHO) Coronavirus Disease (COVID-19) Outbreak: Rights, Roles and Responsibilities of Health Workers, Including Key Considerations for Occupational Safety and Health. Accessed on: August 14, 2020. Available online at: https://www.who.int/docs/default-source/coronaviruse/who-rights-roles-respon-hw-COVID-19.pdf
- Altena E, Baglioni C, Espie CA, Ellis J, Gavriloff D, et al. (2020) Dealing with sleep problems during home confinement due to the COVID‐19 outbreak: Practical recommendations from a task force of the European CBT‐I Academy. J Sleep Res 29(4): e13052.
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, et al. (2020) The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 395: 912-920.
- Choudhry V, Avinandan V (2020) Why COVID-19 Outbreak in India's Slums Will Be Disastrous for The Urban Poor. Accessed on: August 26, 2020. Available online at: https://www.outlookindia.com/website/story/opinion-COVID-19-outbreak-in-indias-slums-will-be-disastrous-for-the-urban-poor/350335
- Hull JH, Loosemore M, Schwellnus M (2020) Respiratory health in athletes: Facing the COVID-19 challenge. Lancet Respir Med 8(6): 557-558.
- Chakraborty K, Chatterjee M (2020) Psychological impact of COVID-19 pandemic on general population in West Bengal: A cross-sectional study. Indian J Psychiatry 62(3): 266-272.
- Allen J, Balfour R, Bell R, Marmot M (2014) Social determinants of mental health. Int Rev Psychiatry 26(4): 392-407.
- Xiang YT, Yang Y, Li W, Zhang L, Zhan Q, et al. (2020) Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7(3): 228-229.
- Cohen S, Kamarack T, Mermelstein R, Williamson G, Oskamp S (1983) Quick Facts about the Tool. J Health Soc Behav 24: 386-396.
- Taylor MR, Agho KE, Stevens GJ Raphael B (2008) Factors influencing psychological distress during a disease epidemic: Data from Australia's first outbreak of equine influenza. BMC Public Health 8(1): 347.
- Reinecke L, Aufenanger S, Beutel ME, Dreier M, Quiring O, et al. (2017) Digital stress over the life span: The effects of communication load and internet multitasking on perceived stress and psychological health impairments in a German probability sample. Media Psychol 20(1): 90-115.
- Wang C, Pan R, Wan X, Tan Y, Xu L, et al. (2020) Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 17(5): 1729.
- Pieh C, Budimir S, Probst T (2020) The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J Psychosom Res 136: 110186.
- Rossi R, Socci V, Talevi D, Mensi S, Niolu C, et al. (2020) COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front Psychiatry 11: 790.
- Rajkumar RP (2020) COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr 52: 102066.
- Sim K, Chan YH, Chong PN, Chua HC, Soon SW (2010) Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J Psychosom Res 68(2): 195-202.
- Qiu J, Shen B, Zhao M, Wang Z, Xie B, et al. (2020) A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen Psychiatr 33(2): e100213.
- Rehman U, Shahnawaz MG, Khan NH, Kharshiing KD, Khursheed M, et al. (2020) Depression, Anxiety and Stress Among Indians in Times of Covid-19 Lockdown. Community Ment Health J 23: 1-7.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Pathology and Toxicology Research
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Rheumatology Research (ISSN:2641-6999)


