3962
Views & Citations2962
Likes & Shares
CASE REPORT
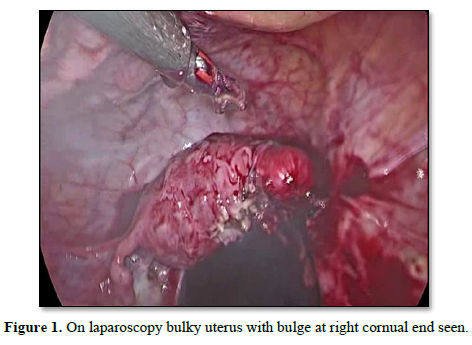
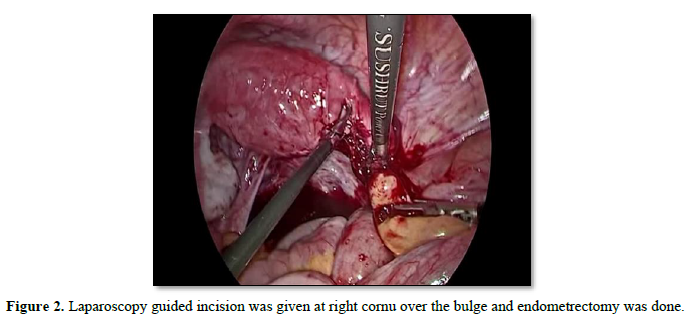
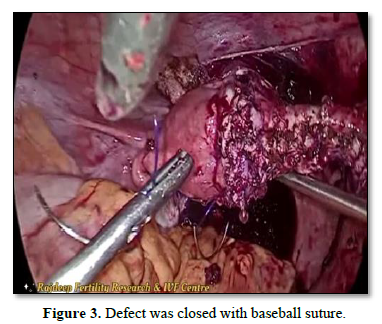
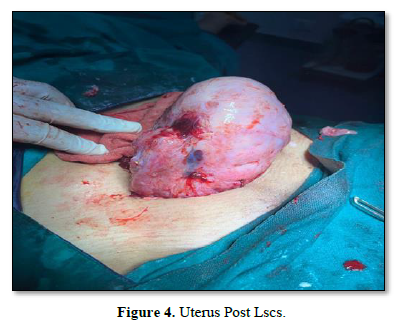
24-year-old married female reported in OPD with severe lower abdominal pain, which was progressive in nature and worsened during menses. There was past history of laparotomy for the same complaints & right-side T.O mass was removed. [1] On USG pelvis there was collection of blood on right side of uterus (adenomyotic); Right ovary absent & left ovary normal. As patient was is severe pain, she was taken for laparo-hysteroscopy after conducting preoperative investigations & obtaining informed consent. On diagnostic laparoscopy, left tube & ovary was normal, uterus was bulky with bulge at right cornual end (Figure 1). On hysteroscopy, uterine cavity appeared normal with normal left ostia & blind right uterine wall (? Septa /? unicornuate uterus). As on laparoscopy uterine contour was normal hence diagnosis of Robert’s uterus was made. Hysteroscopicaly, septa were resected with Collins knife, large amount of old collected blood drained out, still right ostia could not be visualized. Then laparoscopic guided incision was given at right cornu over the bulge and endometrectomy was done (Figure 2). The defect was closed with baseball suture (Figures 3 & 4). Postoperative period was uneventful. Patient was then kept on dienogest for 3 months. 6 months later she conceived spontaneously and delivered healthy male baby at term by LSCS (Figure 5).
 .
.
DISCUSSION
We should always keep obstructive Mullerian anomalies in mind, whenever a young female patient presents with cyclical progressive dysmenorrhea, Asymmetric septate uterus (Robert’s uterus) is a rare Mullerian anomaly. In cases of complex anomalies, a precise representation of the female genital tract can we obtained using 3D USG and MRI with new ESHRE/ESGE classification system [2]. Endometrectomy has been described as the best treatment modality for Robert’s uterus, similar to our case [3]. Signal [4] have reported a pregnancy in asymmetric blind hemi cavity managed by hysterectomy and ipsilateral tubal ligation. In another study, Hysteroscopic unification of a complete obstructing uterine septum, with ablation of the endometrium for prevention of recurrence of hematometra has been reported [5,6]. Ablation is avoided in these young patients, as they are highly concerned of their reproductive function. Hence, intrauterine pediatric Foley’s catheter is inserted for 7 days postoperatively or Cu-T is inserted to prevent intrauterine adhesions. Supplementation with HRT for 5-6 months plus good antibiotic coverage, followed by recheck hysteroscopy and adhesiolysis if necessary, after 12 weeks, have provided good results. In the past, laparotomy for Robert’s uterus was the modality of treatment [7], but now with good endoscopic skills, a minimally invasive approach using combined hysteroscopic and laparoscopic has given us an opportunity to treat these complex anomalies in a much better manner. Hysteroscopic unification has the potential advantage of good fertility outcome but at times, resection of the remaining septa during recheck hysteroscopy may be required. In cases where septal resection is not possible, we should go ahead with the excision of the obstructed half to relieve the symptoms. Thus, ensuring cure in a single sitting but will result in weak lateral uterine wall.
CONCLUSION
Laparoscopy in combination with hysteroscopy and imaging modalities, provides an appropriate approach for rare cases of obstructive Mullerian anomalies, in restoring reproductive function and improving the quality of life.
- Rock JA, Breech LL (2008) Surgery for anomalies of the mullerian ducts. In: Rock JA, Jones HW (eds) Te Linde’s operative gynecology, 10th. edn. Lippincott-Williams and Wilkins a Wolters Kluwer business, Philadelphia, pp: 539-584.
- Di Spiezio Sardo A, Giampaolino P, Scognamiglio M, Varelli C, Nazzaro G, et al, (2016) An Exceptional Case of Complete Septate Uterus with Unilateral Cervical Aplasia (Class U2bC3V0/ESHRE/ESGE Classification) and Isolated Mullerian Remnants: Combined Hysteroscopic and Laparoscopic Treatment. J Minim Invasive Gynecol 23(1): 16-17.
- Capito C, Sarnacki S (2009) Menstrual retention in a Robert’s uterus. J Pediatr Adolesc Gynecol 22: e104-e106.
- Singhal S, Agarwal U, Sharma D, Sirohiwal D (2003) Pregnancy in asymmetric blind hemi cavity of Robert’s uterus-a previously unreported phenomenon. Eur J Obstet Gynecol Reprod Biol 107: 93-95.
- Hucke J, DeBruyne F, Campo RL, Freikha AA (1992) Hysteroscopic treatment of congenital uterine malformations causing hemi-hematometra: A report of three cases. Fertil Steril 58: 823-825.
- Spitzer RF, Caccia N, Kives S, Allen LM (2016) Hysteroscopic unification of a complete obstructing uterine septum: Case report and review of the literature. Fertil Steril 90: e17-2016.e20.
- Gupta N, Mittal S, Dadhwal V, Misra R (2007) A unique congenital mullerian anomaly: Robert’s uterus. Arch Gynecol Obstet 276: 641-643.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Microbiology and Microbial Infections (ISSN: 2689-7660)
- Journal of Astronomy and Space Research
- Advances in Nanomedicine and Nanotechnology Research (ISSN: 2688-5476)
- Journal of Biochemistry and Molecular Medicine (ISSN:2641-6948)
- Journal of Genomic Medicine and Pharmacogenomics (ISSN:2474-4670)
- Proteomics and Bioinformatics (ISSN:2641-7561)
- Food and Nutrition-Current Research (ISSN:2638-1095)







