Research Article
Risks and Challenges Faced by Young Girls During Menstruation and their Attitude Towards the Same: A Prospective Study
4026
Views & Citations3026
Likes & Shares
Introduction: Menarche is a turning point in the lives of adolescent girls. It depicts the transition from childhood to puberty. Girls undergo a lot of physical and emotional changes during this time which can affect their daily life activities. The reproductive health of young women in developing countries requires increased attention. It is vital for young women to obtain appropriate health care so that they can cope with the gynecological problems they may experience during this period and to know the risks so that effective interventions can be made to prevent these problems.
Method: A structured self-administered questionnaire was circulated to young girls within the Pune district of Maharashtra state in India. The collected data were checked for completeness and accuracy and the results were analyzed using appropriate statistical analysis.
Result: A total of 250 young girls participated in the study. It was found that 28.8% of the participants had an irregular menstrual cycle. Polycystic Ovarian Syndrome (PCOS) and thyroid disorders are two of the health conditions noted in this study. Around 33.6% of the participants in this study reported that they experienced pre-menstrual symptoms. The majority of the participants do not visit a gynecologist for a regular check-up.
Conclusion: It was found that the majority of the participants in this study demonstrated a lack of knowledge regarding their menstrual health.
Keywords: Menstruation, Adolescents, Gynecological health, Social stigma
Abbreviations: BMI: Body Mass Index; PCOS: Polycystic Ovarian Syndrome; WHO: World Health Organization
INTRODUCTION
Adolescence is a period of extensive physical and psychological change for young girls. Adolescents constitute over 21.4 % of the population in India [1]. As per the World Health Organization, 10-19 years age groups are defined as the “Adolescent” group and the 15-24 age groups as the “Young” group. Due to the intersection of adolescent and youth ages, the 10-24 age groups are considered as “Young People” [2]. The reproductive health of young women aged 15-24 in developing countries requires increased attention. The number of young women is large, and their numbers are projected to rise. Young girls experience not only changes in the brain, neuroendocrine system, and hormone concentrations but also physical and emotional changes and risks with gynecological problems that affect reproductive health and social life [3]. Young girls encounter some risks with gynecological problems such as menstrual problems, vaginal discharge and infections, pelvic mass and ovarian cysts, trauma and sexual abuse, genital system anomalies, abdominal and pelvic pain, adolescent pregnancies, breast problems, and early and late puberty. Furthermore, the young population is generally perceived as a healthy group that does not require health care services, and thus they cannot adequately benefit from these services. For this reason, the diagnosis of the gynecological problems whose onset is rooted in this period may be delayed, leading to higher mortality or morbidity at adult ages. However, it must be noted that the majority of the health problems experienced in this period may be prevented [4]. Adolescents have the lowest mortality among the different age groups and have therefore received low priority. Many adolescents with menstrual disturbances never present to their family doctor or gynecologists. Uneasiness around discussing menstruation, fear of disease, and ignorance about available services may lead to delayed presentation. Menarche is considered as the central event of female puberty. The average age of menarche is around 12 and 13 years. Menstrual bleeding lasts 2–7 days in 80–90 % of adolescent girls. Most cycles still range from 21 to 45 days which, even in the first year after menarche, is normal. Thus, consideration should be given to a gynecological evaluation in adolescent girls whose cycles are longer than the above interval and have more excessive flow than normal [5]. It is vital for young women to obtain appropriate health care so that they can cope with the gynecological problems they may experience during this period and to know the risks so that effective interventions can be made to prevent these problems. Early detection and treatment of complications and taking required precautions improve both the health and quality of life of young women and may prevent future risks of some chronic gynecological problems. There are few studies that determine the prevalence of extensive risk with gynecologic problems in young women. This study is therefore aimed to determine the risk and taboos with respect to gynecological disorders among young women in the Pune district of Maharashtra in India.
METHODOLOGY
Design
This study was a prospective, questionnaire-based survey conducted for four months between January and April 2021.
Population and Sampling
A total of 250 young girls participated in the study. Electronic and verbal consents were obtained from the study participants prior to the administration of the survey questionnaire. The study included girls who were unmarried and gave consent to participate in the study. Married girls and those above thirty years of age were excluded from the study.
Materials and procedure
A structured self-administered questionnaire prepared in English was used to collect data. It included questions related to detailed history with duration and severity of symptoms of various gynecological problems, menstrual history, history of bleeding disorders, and socio-demographic characteristics of respondents. The common mode of administration of the survey questionnaire was through the online mode and personal interview survey. The collected data were checked for completeness and accuracy.
Data Processing and Analysis
After data collection, each questionnaire collected was checked for completeness and vague responses. With this information, gynecological problems and different types of menstrual disorders commonly found in young women were analyzed. Data analysis was carried out manually by using tally and calculator, and the result was presented by using frequency tables and charts.
Statistical Analysis
The data were checked for normality using the Skewness and Kurtosis test. A 0.5 value was used as a cut-off for Skewness. The data was said to be normally distributed if Skewness ranged between -0.5 and 0.5. The normally distributed data were presented using mean with standard deviation and non-normally using median with interquartile range (IQR). Categorical data are presented in terms of variables and percentages. P values
RESULTS
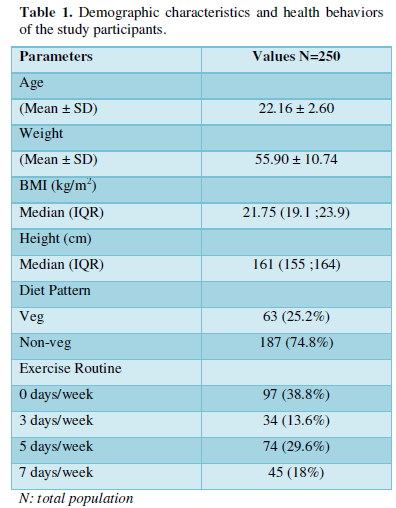
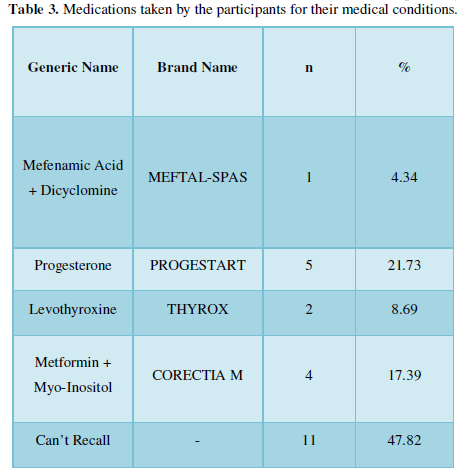
Demographic and health characteristics A total of 250 young girls participated in the study. Table 1 describes the demographic and health behaviors of the study participants. The average age in years of the study participants was 22.16±2.60, and the average weight in kilogram was 55.90±10.74. The participants had a median Body Mass Index (BMI) of 21.75 kg/m2 (19.1; 23.9), and their median height was 161cm (155 ;164). As per their BMI, the majority (n=145) of the participants fall under the normal category, 54 of them are underweight, 9 of them are at risk of being overweight while 34 falls under the category of overweight, and 8 of them come under the obese category. It was found that 74.8% of the participants had a non-vegetarian diet pattern while the remaining 25.2% had a vegetarian diet. Nearly 38.8% of the participants did not engage themselves in any kind of exercise throughout the week, 13.6% exercised 3 times a week, 29.6% exercised 5 times a week, and 18% of them were exercising every day of the week.
Menstrual Characteristics
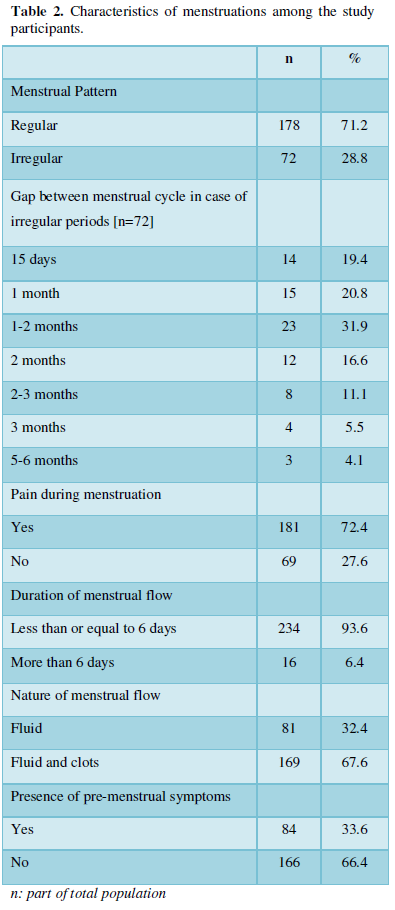
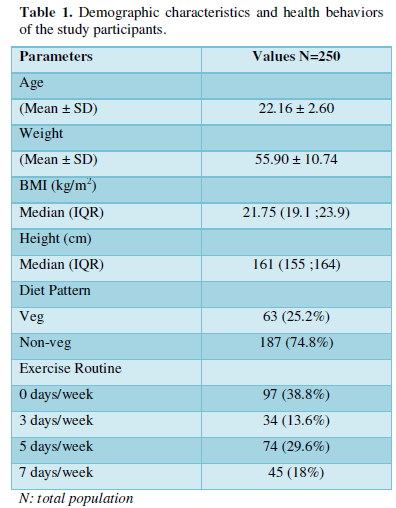
The menstrual characteristics of the participants are given in Table 2. About 71.2% of the participants stated that their menstrual cycle was regular while the remaining 28.8% stated it was irregular. In those who had an irregular menstrual cycle, the gap between their two consecutive menstrual cycles was about 15 days, 1 month, 1-2 months, 2 months, 2-3 months, 3 months, and 5-6 months for 14, 15, 23, 12, 8, 4, and 3 participants respectively. Nearly 93.6% of the participants reported having menstrual flow less than or equal to 6 days while 6.4% stated their menstrual flow lasts for more than 6 days. Pain during menstruation was reported by 72.4% (n=181) of the participants, and the remaining 27.6% (n=69) of them reported no pain during their menstrual discharge. Of the total 181 participants who reported pain during menstruation, 59 (32.59%) of them take over-the-counter (OTC) medications for the same.
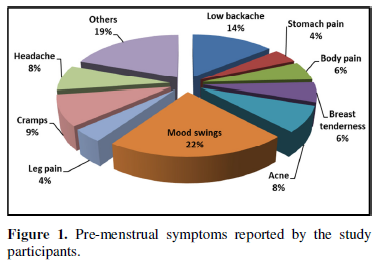
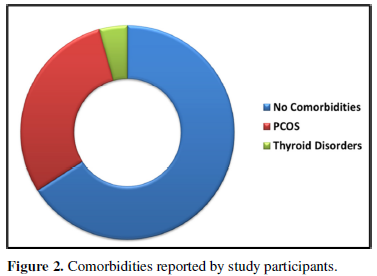
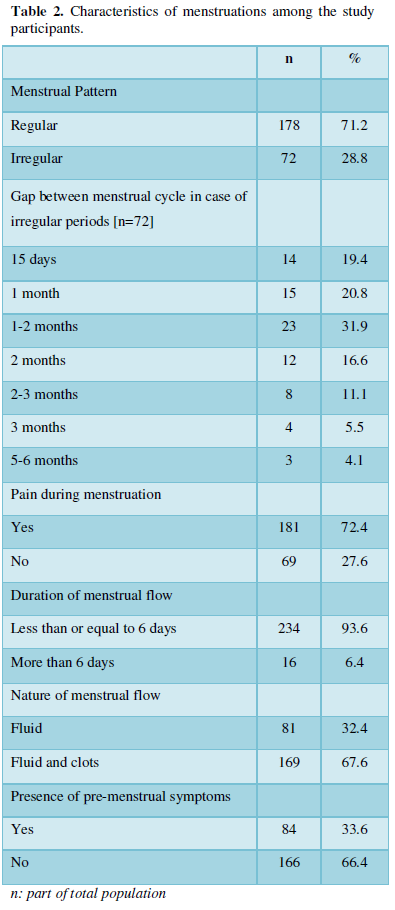
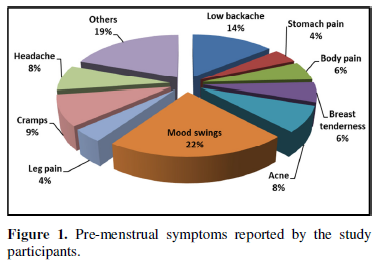
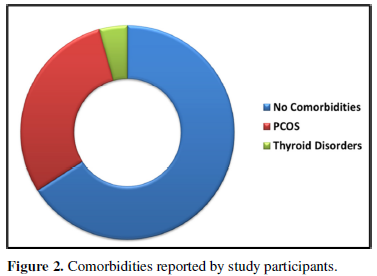
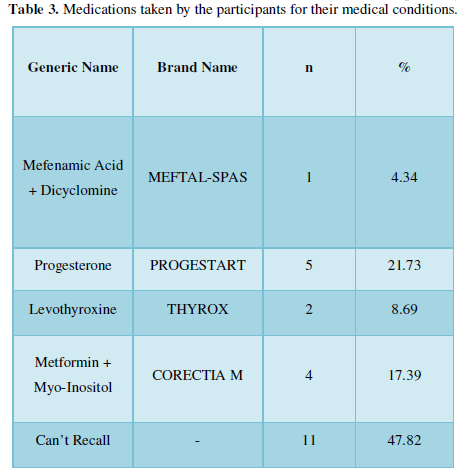
The nature of menstrual flow was mainly fluid and clots for 67.6% of the participants and only fluid for 32.4% of them. Around 33.6% of the participants in this study reported that they experienced pre-menstrual symptoms. The various pre-menstrual symptoms experienced by the participants are depicted in Figure 1. The most common symptoms reported are mood swings, low backache, headache, stomach pain, acne, breast tenderness, cramps, leg pain, and body pain. Some of the fewer common symptoms were bloating, nausea, diarrhea, white discharge, weakness, and muscle pain. In this study, polycystic ovarian syndrome (PCOS) and Thyroid disorders are the two medical conditions that were affecting 35.2% (n=88) of the participants. Thirty per cent of the participants were suffering from PCOS while thyroid disordered accounted for 4.4% (Figure 2). Out of the total 35.2% participants, 73.86% (n=65) do not take any medications for the same. From the remaining 26.13% (n=23), 11 of them couldn’t recall the name of their medications. Name of the medications used by the participants for their medical condition is given in Table 3.
Psychological Factors and Social Stigma
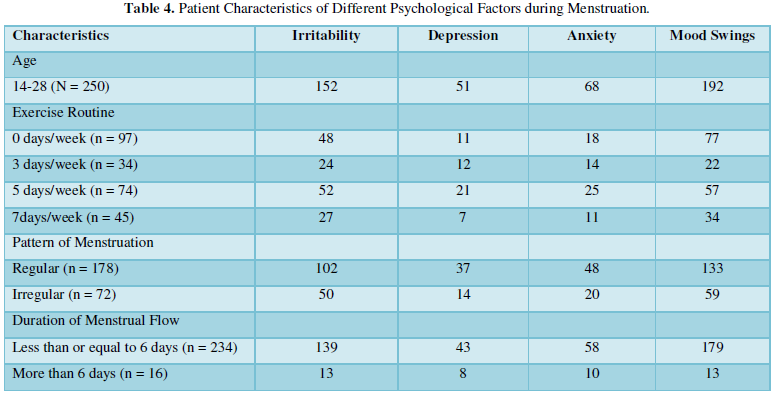
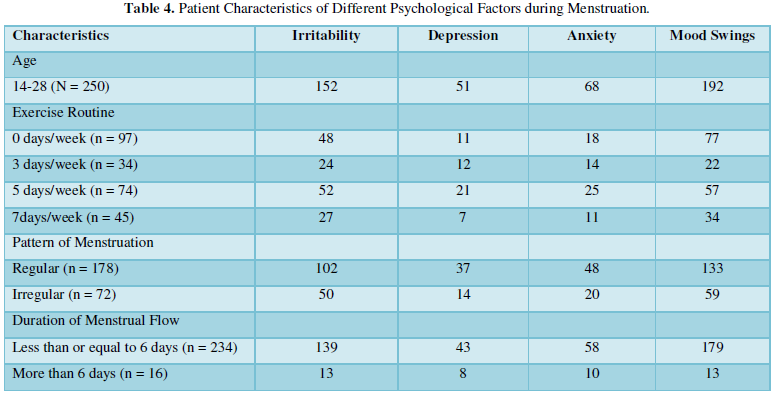
During menstruation, young girls go through a wide range of emotions. Mood swings (n=192) and irritability (n=152) were the most common symptoms of emotional distress during menstruation reported in our study. Some of the other symptoms reported by the participants in this study are anxiety (n=68) and depression (n=51). Nineteen participants revealed that they do not experience any such symptoms during their periods. Table 4 compares the different demographic and menstrual characteristics of the study participants with the various psychological factors during menstruation.
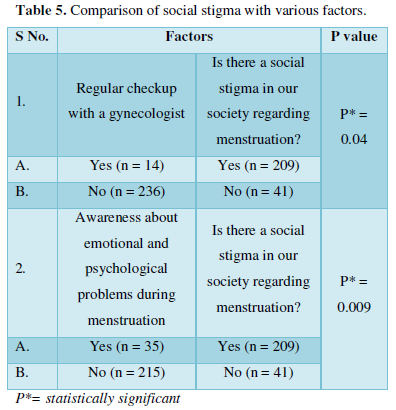
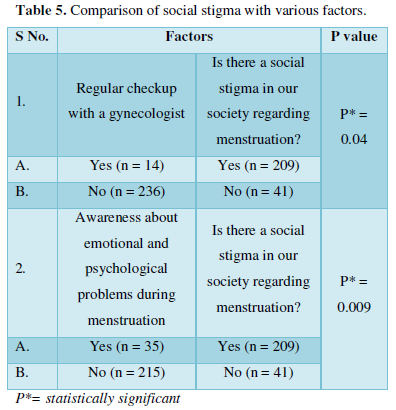
Nearly 44% (n=110) of the participants admitted to missing school due to menstrual discomfort at least once during their school days. Access to adequate menstrual aids was reported by 92.4% of them, while the remaining 7.6% claimed they do not have an adequate supply of menstrual aids all the time. Table 5 compares the perception of social stigma around menstruation with different parameters. A statistically significant result (P = 0.04) was obtained when we compared the results regarding regular gynecological check-up and their perception of social stigma regarding menstruation in our society. A similar result (P = 0.009) was also observed on comparing awareness of emotional and psychological problems during period with social stigma.
DISCUSSION
As per the definition by World Health Organization (WHO), adolescents are individuals who fall in the age group of 10-19 years, youth as individuals between 15-24 years, and young people as those between 10-24 years of age [6]. In this study, 19.2% of the participants are adolescents, while the remaining falls under the young people category. Menarche is a turning point in the lives of adolescent girls. It depicts the transition from childhood to puberty. Healthy eating and physical activity during this stage are important as the various body changes during this time affect an individual's nutritional needs and promote good health respectively. The present study shows that majority of the study participants do not engage in any sort of exercise. Similar results were obtained by Rukiye [7]. A study conducted by Demir et al shows that regular exercise and consumption of a balanced diet helps in reducing the risk of gynecological problems [8]. Various studies have stressed on the importance of Body Mass Index (BMI) as an index of nutritional assessment [9-10]. While most of the participants had a normal Body Mass Index (BMI), 13.6% of them were overweight, and 3.2% were obese. Obesity is linked to various health problems and can cause problems with gynecological health of young girls. There is a well-established link between obesity and PCOS. Being overweight during adolescence and youth can lead to a myriad of menstrual problems over the reproductive years which can ultimately lead to fertility problems post marriage [11]. Similar to obesity, being underweight also comes with a lot of negative effects on health. Almost 21.6% of our participants are underweight. Studies have linked low body fat and weight loss to the late appearance of menarche, disorders of the menstrual cycle, and problems with conception [12-13]. Most females experience some kind of premenstrual syndrome (PMS) throughout their reproductive years. This can range from symptoms such as appetite changes, fatigue, low energy, backache, and cramps to irritability, depressed mood, and anxiety [14-15]. Similarly, the findings of our study also indicate a considerable modulating effect of the menstrual cycle on the simultaneous execution of emotional processing in young girls. A study conducted by Vaghela [16] found that regular exercise and yoga can help in reducing the pain and intensity of PMS symptoms. The presence of menstrual pain and symptoms is common during menstruation. Evidence suggests that the onset of puberty coincides with girls dropping out of school in many of the developing countries [17]. In the present study, 44% of the girls admitted to missing school at some point either due to menstrual discomfort or lack of access to menstrual aids. Nearly 7.6% of the participants reported not having an adequate supply of menstrual aids. A study conducted by Parker et al demonstrated the association between menstrual dysfunction and absence from school [18]. Literature review reveals that the prevalence of PCOS in India is around 3.7 to 22.5 per cent [19]. This study reported that 30.8% of the participants had physician-diagnosed PCOS. Around 4.4% of our participants also suffered from thyroid disorders. Eight girls (3.2%) had both PCOS and thyroid disorder. The presence of both PCOS and thyroid disorders are interconnected, as thyroid autoimmunity increases in those with PCOS. Studies reveal that the prevalence of thyroid disorders increases in females with PCOS [20]. However, this data could be much higher in reality as the majority (94.4%) of the study participants do not have a regular gynecological checkup, and this could lead to the underdiagnosis of such menstrual disorders. Although most of the participants agree that a yearly gynecological examination is essential, only about 5.6% of them have had regular checkups so far. As menstrual problems are considered taboo or embarrassing in India, the rate of visiting a gynecologist is low. A vast majority of the participants are unaware of the emotional and psychological impact of menstruation. Most (83.6%) of them agree that the stigma attached to menstrual health still exists in India. Taboos related to periods in religions and cultures are difficult to fight because of longstanding roles in the societies in which they exist, but various steps should be taken to raise awareness around menstrual stigma and to end the period shame.
CONCLUSION
This study demonstrates a lack of knowledge amongst young girls regarding the importance of good menstrual health. If pre-existing menstrual disorders are not diagnosed at the early stage it can lead to serious health problems and fertility issues later on in life. Health education classes must be conducted to create awareness regarding adolescent gynecological problems in schools and colleges. Government plans should provide period products to all schools, colleges, and universities. Educational programs should be conducted for parents to make them aware of their children's problems and remove the stigma around menstruation within the families.
- Hanson M, Gluckman P (2006) Evolution: Development and timing of puberty. Trends Endocrinol Metab 17(1): 7-12.
- World Health Organization (2018) Promoting the Health of Young People in Custody. 2012. Available online at: http://www.euro.who.int/document/e81703.pdf
- Lerner RM, Steinberg L (2004) (eds) Puberty and Psychological Development. In: Handbook of Adolescent Psychology. Hoboken: New Jersey, John Wiley & Sons. pp: 15-44.
- Akarsu RH, Alsac SY (2019) Risks with Gynecological problems on the health of University Students. Pak J Med Sci 35(3): 758-763.
- Rathod AD, Chavan RP, Pajai SP, Bhagat V, Thool P (2016) Gynecological Problems of Adolescent Girls Attending Outpatient Department at Tertiary Care Center with Evaluation of Cases of Puberty Menorrhagia Requiring Hospitalization. J Obstet Gynaecol India 66(S1): S400-S406.
- World Health Organization. Adolescent Health. Available online at: https://www.who.int/southeastasia/health-topics/adolescent-health
- Akarsu RH, Alsac SY (2019) Risks with Gynecological problems on the health of University Students. Pak J Med Sci 35(3): 758-763.
- Demir B, Algül LY, Güven ESG (2006) Investigation of premenstrual syndrome incidence and associated factors in health care personnel. Turk J Obstet Gynecol 3: 262-270.
- Cherian R, Rajasree S, Soman CR (1988) Anthropometric assessment of malnutrition comparison of two age independent criteria. Indian J Nutr Diet 25: 82.
- Rao D. Hanumantha (1996) Nutrition Profile of Indian Tribes. Nutrition News published by National Institute of Nutrition 17(2): 1-6.
- Wood PL, Bauman D (2015) Gynecological issues affecting the obese adolescent. Best Pract Res Clin Obstet Gynaecol 29(4): 453-465.
- Hayward VH, Stolarczyk LM (1996) Applied body composition. Human Kinetics, Champaign.
- McArdle WD, Katch FI, Katch VL (2014) Exercise physiology: Energy, nutrition, and human performance.
- Steiner M (1997) Premenstrual syndromes. Annu. Rev Med 48(1): 447-455.
- Dickerson LM, Mazyck PJ, Hunter MH (2003) Premenstrual syndrome. Am Fam Physician 67(8): 1743-1752.
- Vaghela N, Mishra D, Sheth M, Dani VB (2019) To compare the effects of aerobic exercise and yoga on Premenstrual syndrome. J Educ Health Promot 8: 199.
- McCarthy K, Brady M, Hallman K (2016) Investing when it counts: Reviewing the evidence and charting a course of research and action for very young adolescents. Population Council.
- Parker MA, Sneddon AE, Arbon P (2010) The menstrual disorder of teenagers (MDOT) study: Determining typical menstrual patterns and menstrual disturbance in a large population‐based study of Australian teenagers. BJOG 117(2): 185-192.
- Ganie MA, Vasudevan V, Wani IA, Baba MS, Arif T, et al. (2019) Epidemiology, pathogenesis, genetics & management of polycystic ovary syndrome in India. Indian J Med Res 150(4): 333-344.
- Singla R, Gupta Y, Khemani M, Aggarwal S (2015) Thyroid disorders and polycystic ovary syndrome: An emerging relationship. Indian J Endocr Metab 19(1): 25-29.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Biochemistry and Molecular Medicine (ISSN:2641-6948)
- Journal of Agriculture and Forest Meteorology Research (ISSN:2642-0449)
- Advances in Nanomedicine and Nanotechnology Research (ISSN: 2688-5476)
- Journal of Genetics and Cell Biology (ISSN:2639-3360)
- Food and Nutrition-Current Research (ISSN:2638-1095)
- Journal of Microbiology and Microbial Infections (ISSN: 2689-7660)
- Proteomics and Bioinformatics (ISSN:2641-7561)




