Research Article
Spontaneous Rupture of An Unscarred Non-Laboring Gravid Uterus at Term: A Case Report
5367
Views & Citations4367
Likes & Shares
Background: Rupture of the pregnant uterus is life-threatening for the mother and fetus. Most ruptures occur in women who have had a previous trans myometrial surgical incision, typically for cesarean delivery. Rupture of the unscarred uterus is rare, but the incidence is increasing. It is associated with higher major maternal and neonatal morbidity than cases of rupture of the scarred uterus.
Case presentation: A 36 years old gravida 4 para 3 mother presented at gestational age of 38 weeks with nonspecific upper abdominal pain of 12 hours which was associated with multiple episodes of vomiting which was initially ingested matter latter became blood mixed. She had no bearing down pain or passage of liquor. She denied any vaginal bleeding or urinary symptoms. The previous deliveries were at term and at home. During her third delivery, after the delivery of baby she failed to deliver placenta and was taken to nearby primary hospital, there placenta was delivered manually and was transfused two unit of blood. Otherwise, she has no history of pelvic surgery, no history of trauma. Initially, she was diagnosed to have severe anemia secondary to acute blood loss secondary to upper gastrointestinal bleeding. Finally diagnosed to have uterine rupture and total abdominal hysterectomy done.
Conclusion: A high index of suspicion is needed in pregnant patients presenting with sudden onset of abdominal pain so as not to miss uterine rupture and its complications.
Keywords: Uterine rupture, Unscarred uterus, Upper gastrointestinal bleeding, Intrauterine fetal death
BACKGROUND
Uterine rupture is a rare but hazardous obstetric complication with catastrophic outcomes. It is a life-threatening obstetric emergency bearing a high risk for the mother and the fetus [1]. Rupture of the unscarred pregnant uterus is a rare event, estimated to occur in 1/5700 to 1/20,000 pregnancies [2]. Here we are presenting unusual case of 36 years female patient with spontaneous upper uterine segment transverse uterine rupture. The purpose of presenting the case is to focus light on possibility of rupture in unscarred uterus in a non-laboring uterus with no previous risk factors.
CASE PRESENTATION
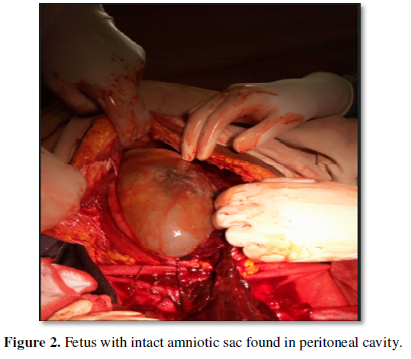
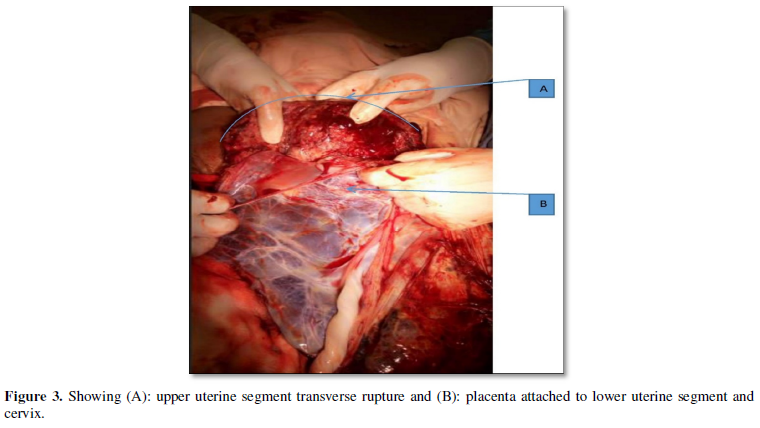
A 36 years old gravida 4 para 3 mother presented at gestational age of 38 weeks with nonspecific upper abdominal pain of 12 hours which was associated with multiple episodes of vomiting which was initially ingested matter latter became blood mixed. She had no bearing down pain or passage of liquor. She denied any vaginal bleeding or urinary symptoms. She had no prenatal care follow up. The previous deliveries were at term and at home. During her third delivery, after the delivery of baby she failed to deliver placenta and was taken to nearby primary hospital, there placenta was delivered manually and was transfused two unit of blood. Otherwise, she has no history of pelvic surgery, no history of trauma. On examination, she was pale and distressed with a PR 140/min and BP 80/60 mmHg. Abdomen was distended, tense and tender. It was difficult to feel fetal body parts. There was no uterine contraction and fetal heart beat was negative. There was fluid thrill and shifting dullness. Emergency obstetric ultrasound scan revealed fetal demise. Placenta covered cervical is totally fluid in peritoneal cavity. Hematocrit was determined and18% and blood group was O positive. Internist was also consulted and she was diagnosed to have hypovolemic shock secondary to acute blood loss secondary to perforated peptic ulcer diseases, severe anemia secondary to acute blood loss, IUFD and placenta previa totalis. She was started on resuscitation with crystalloid and took 2000ml of normal saline over one hour, transfused 2 unit of compatible blood, given omeprazole 80mg intravenously(iv), metoclopramide 10mg iv. Despite these management patient’s clinical condition was the same (still hypotensive and tachycardic) and decided for emergency laparotomy. On entry into the peritoneal cavity, a large (500 mL) hematoma was identified anterior to the uterus (Figure 1), freshly dead male fetus (weight 2800 grams) in intact amniotic sac was found in abdominal cavity (Figure 2). Placenta was found covering lower uterine segment and cervix (Figure 3). There was upper uterine segment transverse uterine rupture which was about 15 cm involving both sides uterine arteries (Figure 3A & B). There was no evidence of Couvelaire uterus and no demonstrable congenital uterine anomaly. Rest of the pelvis looked normal, with no evidence of endometriosis or adhesions. About 1.5 l hemoperitoneum sucked out and hysterectomy done. She received one unit of blood during intraoperative and one unit during the post-operative period. She was discharged 5 days after surgery.

DISCUSSION
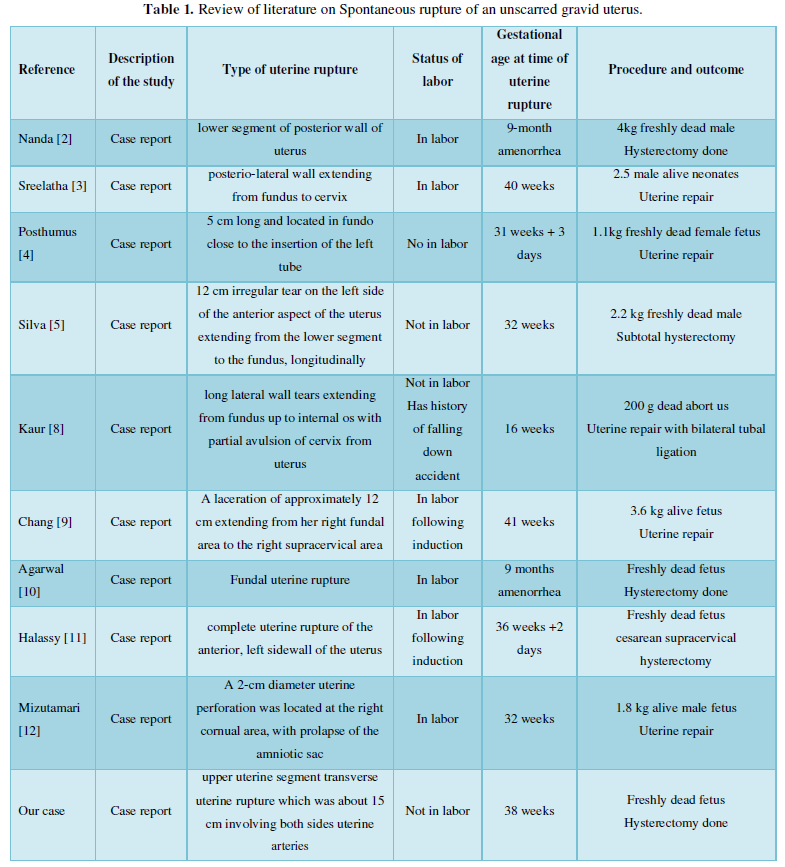
This case presentation describes a rare presentation of Spontaneous rupture of an unscarred non-laboring gravid uterus at term diagnosed upon laparotomy. Rupture of the non-laboring unscarred uterus is rare and is a potentially catastrophic event and can be life-threatening for the mother and fetus. Rupture of an unscarred uterus may be caused by trauma or congenital or acquired weakness of the myometrium. Sources of trauma include motor vehicle accidents, domestic violence and obstetric maneuvers (e.g., internal or external version, breech extraction) [3] which were not present in this case. The myometrium may be inherently weak because of a congenital disorder, such as Ehlers-Danlos type IV [4] but this was not excluded in our patient because genetic testing was not available. The myometrium may become weakened from acquired causes like protracted labor or use of strong uterotonic drugs (e.g., misoprostol), which place prolonged stress on the myometrium [3] but in our case, the patient was not in labor and she was not induced or augmented. Grand multiparty, advanced maternal age, endometriosis, arteriovenus malformation and abnormal placentation like placenta accreta, fetal macrosomia, and uterine instrumentation are all predisposing factors for uterine rupture [3]. In our case, during her third delivery she had retained placenta and it was removed manually and manual removal might have been forceful that might have caused weakening of myometrium. The uterine rupture was upper uterine segment transverse and she had placenta previa totalis with bulk anterior which might support that manual removal of placenta in the previous delivery might have caused myometrial weakening in upper uterine segment. Initial signs and symptoms of uterine rupture are typically nonspecific, which makes diagnosis difficult and sometimes delays definitive therapy [5]. But most commonly uterine rupture in the third trimester presents as sudden occurrence of severe and shearing abdominal pain with cessation of uterine contractions while vaginal bleeding and shock occurs [6]. The fetus suffers in utero distress with bradycardia as well as decreased fetal movement and the infrequent symptoms of uterine rupture are epigastric pain, shoulder pain (right sided or bilateral), abdominal distention and paralytic ileus as well as, hematuria, etc. In our case, the patient presented with upper abdominal pain and vomiting of ingested matter mixed with blood of multiple episodes, which led to the diagnosis of perforated peptic ulcer disease and delayed the diagnosis and management of uterine rupture. The basic treatment for a patient with a ruptured uterus is immediate resuscitation and surgery. At the time of exploratory laparotomy, the patient should be evaluated for possible uterine repair or hysterectomy. For young females especially those who do not have children, it is better to preserve the uterus. But in some cases, the patients often have severe tears not suitable for repair. In general, the surgical option must be individualized and should be dependent upon the type, location and extent of the rupture, as well as on the patient’s parity, the degree of bleeding, the available resources and desire to preserve her child bearing capacity [7]. If possible, repair is probably the best approach. In cases with wide bruises and contaminations, intractable uterine bleeding and multiple uterine rupture sites and longitudinal uterine rupture hysterectomy is preferable [8]. In our case, the patient was resuscitated with 2 bags of crystalloid intravenous fluid and transfused 2 unit of compatible blood before surgery, transfused one unit of blood intraoperatively and one unit of blood post operatively. Hysterectomy was done because, the rupture was upper uterine segment transverse involving both uterine arteries. A comparison of this case with other case reports published previously is presented in Table 1.
CONCLUSION
Spontaneous uterine rupture is a serious and potentially catastrophic event and high index of suspicion is needed in pregnant patients presenting with sudden onset of abdominal pain so as not to miss uterine rupture and its complications
-
Kolala SG, Hareesh SG, Sunil CA, Raju HP (2011) Spontaneous Rupture of Unscarred Gravid Uterus. J Forensic Sci 56: S263-S265.
-
Nanda K, Singh S, Dhama V, Choudhary R, Azad R (2017) A rare case of spontaneous posterior wall rupture in an unscarred uterus during labour. Int J Reprod Contracept Obstet Gynecol 6(9): 4127-4130.
-
Shruthi K, Sreelatha S, Kumar S, Chandushree, Madhuri, et al. (2018) A Rare Case of Uterine Rupture in an Unscarred Uterus. Gynaecol Perinatol 2(3): 281-284.
-
Posthumus L, Donker ME (2017) Uterine rupture in a primigravid patient, an uncommon but severe obstetrical event : A case report. J Med Case Rep 11(1): 339.
-
Silva GRC, Gange P, Karunarathne N, Senevirathne N (2012) Spontaneous rupture of an unscarred non-labouring gravid uterus at 32 weeks gestation. Sri Lanka J Obst Gyn 34(2): 53-54.
-
Zhao Y, Tian B, Xu Y, Dai H (2017) Case Report Spontaneous prelabor unscarred uterine rupture in primigravida : A case report and review of literature. Taiwan J Obstet Gynecol 10(4): 7296-7303.
-
Wang Y-L, Su TH (2006) Obstetric uterine rupture of the unscarred uterus: A twenty-year clinical analysis. Gynecol Obstet Invest 62(3): 131-135.
-
Kaur JBG, Sehgal A (2012) Rupture uterus following blunt trauma at 16 weeks gestation. Int J Reprod Contracept Obstet Gynecol 1: 64-66.
-
Chang CY, Chou SY, Chu IL, Hsu CS, Chian KH, et al. (2006) Silent uterine rupture in an unscarred uterus. Taiwan J Obstet Gynecol 45(3):250-252.
-
Agarwal R, Gupta B, Radhakrishnan G (2011) Rupture of intrapartum unscarred uterus at the fundus: A complication of passive cocaine abuse. Arch Gynecol Obstet 283: 53-54.
-
Halassy SD, Eastwood J, Prezzato J (2019) Uterine rupture in a gravid, unscarred uterus: A case report. Case Rep Womens Health 24: e00154.
-
Etsuko M, Tomoko H, Takashi O, Hidetaka K (2014) Spontaneous Rupture of an Unscarred Gravid Uterus in a Primigravid Woman at 32 Weeks of Gestation. Case Rep Obstet Gynecol 2014: 209585.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Genomic Medicine and Pharmacogenomics (ISSN:2474-4670)
- Journal of Veterinary and Marine Sciences (ISSN: 2689-7830)
- Journal of Microbiology and Microbial Infections (ISSN: 2689-7660)
- Journal of Astronomy and Space Research
- Journal of Biochemistry and Molecular Medicine (ISSN:2641-6948)
- Journal of Agriculture and Forest Meteorology Research (ISSN:2642-0449)
- Food and Nutrition-Current Research (ISSN:2638-1095)





