Research Article
Serum CA125 As A Tumor Marker in Japanese Patients with Endometrial Cancer
5235
Views & Citations4235
Likes & Shares
In this study, we investigated diagnostic and prognostic applications of serum CA125 for endometrial cancer. Between January 2006 and December 2012, serum CA125 levels were examined prospectively in 215 patients with endometrial cancer, and were then determined during treatment and at scheduled follow-up examinations in patients with elevated baseline serum CA125 levels. During this period, a total of 215 patients (stage I, 142; stage II, 19; stage III, 32; stage IV, 22) were treated for endometrial cancer. Subsequently 52 patients (24.2%) relapsed at the time of the last follow-up and the median follow-up time was 86 months (1-141). Elevated serum CA125 levels were identified in 69 patients (32.1%) and were associated with clinical stage (p = 0.0001), histological grade (p=0.001), histological type (endometrioid or other) (p=0.02), myometrial invasion depth (p = 0.0002), lymph node metastasis (p=0.0008), distant metastasis (p=0.002), and relapse of disease (p=0.005). Among the 69 patients with elevated serum CA125 levels, 56 (81.2%) achieved remission and serum CA125 levels returned to the normal range in all cases. Eleven patients (19.6%) had relapses among these patients and serum CA125 level has been elevated again in 8 (72.7%) cases. There is no statistically significant relationship between an elevated serum CA125 levels and OS (p=0.06).
Serum CA125 level seemed to be a potential prognostic indicator for endometrial cancer in clinical practice.
Keywords: Serum CA125, Tumor marker, Endometrial cancer, Japanese patients
INTRODUCTION
Endometrial cancer is the most common gynecologic malignancy of the female, and its incidence is increasing over the world. Although several biomarkers have been associated with clinical characteristics and prognosis in endometrial cancer [1-8], none have been available in clinical practice. Therefore, novel biomarkers for endometrial cancer are required.
In particular, measurement of serum CA125 as a tumor marker has been investigated in patients with endometrial cancer. However, the precise roles of CA125 in preoperative evaluations of endometrial cancer patient remain uncharacterized and controversial [6-8].
In this study, we investigated the diagnostic and prognostic value of serum CA125 levels in patients with endometrial cancer.
MATERIALS & METHODS
Methods
This prospective study was approved by the Osaka City University Graduate School of Medicine Institutional Review Board. Available electronic medical records from January 2006 to December 2012 were reviewed, and serum CA125 levels and clinicopathological features were analyzed in patients with endometrial cancer. Patients with co-existing malignant disease were excluded from analyses.
Clinical management of endometrial cancer in our institution was performed by gynecologic oncologists and diagnoses were established by curettage. All patients were clinically and/or surgically classified according to the International Federation of Gynecology and Obstetrics (FIGO) surgical staging system [9]. Histological diagnoses were confirmed using microscopic examinations of hematoxylin- and eosin- stained sections according to the World Health Organization criteria. In operable cases, patients received total abdominal or radical hysterectomy plus bilateral salpingo- oophorectomy. Peritoneal fluid samples were obtained for cytological testing, and systemic pelvic lymphadenectomy was performed in most cases. Para-aortic lymph node sampling was performed in patients with intermediate or high-risk disease. In patients without lymph node adenectomy, lymph nodes of >1 cm were detected using computed tomography (CT) and/or resonance imaging (MRI) and were considered positive lymph nodes. After surgery, adjuvant chemotherapy was provided for patients with intermediate or high-risk disease. No hormonal therapies or targeted treatments such as monoclonal antibodies or tyrosine kinase inhibitors were administered. Patient treatments were followed with gynecologic examinations including trans-vaginal and/or abdominal ultrasonography and cytological testing of vaginal cut edges, and laboratory examinations including assessments of tumor marker expression. Further CT and/or MRI examinations were performed for patients with clinically suspicious symptoms and/or elevated tumor marker levels. Recurrent disease was diagnosed using biopsy or imaging methods.
Serum CA125 levels were measured before therapy during pre-treatment examinations. A lower level of 35 U/ml was used as the cut-off for normal values of serum CA125 levels. In patients with elevated baseline serum CA125 levels, these were measured again during treatment and at scheduled follow-up examinations. Intervals between follow-up appointments are as shown below; every 2 months for the first 1-3 years after treatment, every 6 months for the 4-5 years after treatment, and annually from the 6th year after treatment.
Statistical analysis
Relationships between clinical groups were analyzed using Fisher’s exact probability test. In the analyses of disease relapse, survival distributions were calculated using the Kaplan-Meier method, and relapse-free patients included those with no evidence of disease recurrence and those who died due to unrelated causes. Univariate and multivariate Cox regression analyses were used to identify variables associated with relapse-free survival and associations were considered significant when p <0.05.
RESULTS AND DISCUSSION
Clinical characteristics of patients with endometrial cancer
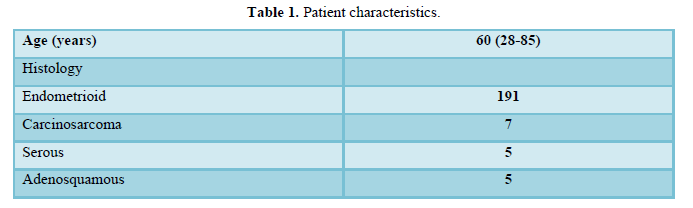
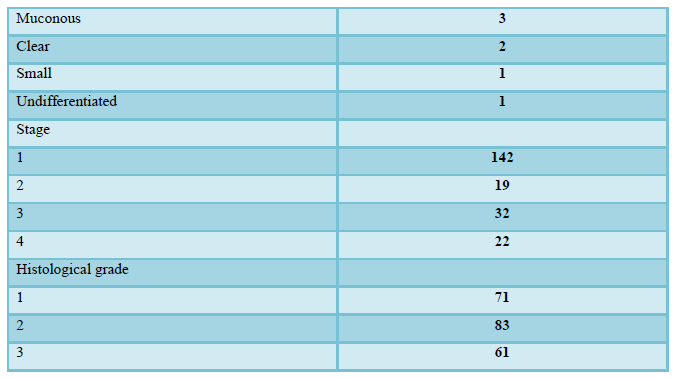
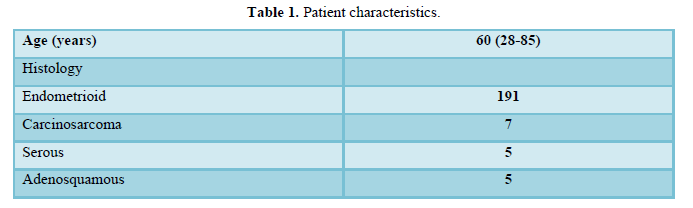
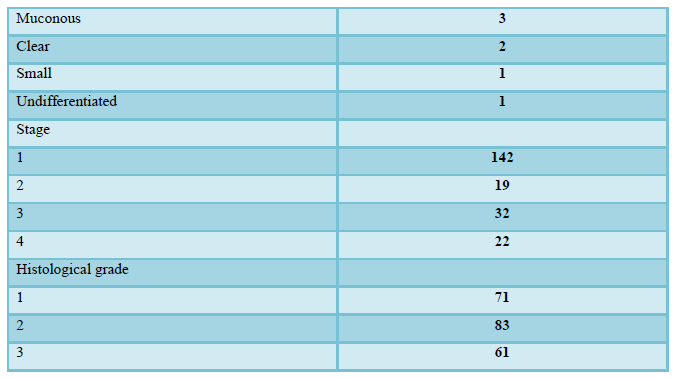
Clinical characteristics of patients with endometrial cancer are shown in Table 1. During this period, a total of 215 patients (stage I, 142; stage II, 19; stage III, 32; stage IV, 22) were administrated. The median age was 60 years (28-85), and histology types included 191 endometrioid adenocarcinomas, seven carcinosarcomas, five serous adenocarcinomas, five adenosquamous carcinomas, three mucinous adenocarcinomas, two clear cell adenocarcinomas, one small cell carcinoma and one undifferentiated carcinoma. Histological grades were defined as grades 1, 2, and 3 in 71, 83, and 61 cases, respectively. Surgery was performed as primary therapy in 212 cases (98.6%) and chemotherapy was performed in three inoperable cases (1.4%). Surgery included total abdominal or radical hysterectomy plus bilateral salpingo-oophorectomy in 210 patients (97.7%) and additional lymphadenectomy was performed in 194 patients (90.2%). Para-aortic lymph node biopsies were performed in 24 patients (11.2%) and tumor biopsies were taken from two patients (0.9%) with advanced disease. After surgery, adjuvant chemotherapy was provided for 101 patients (47.0%) with intermediate or high-risk disease, and included paclitaxel and carboplatin therapy (TC) in 86 patients, docetaxel and carboplatin therapy (DC) in 10 patients, and docetaxel and cisplatin therapy (DP) in five patients. TC therapy was provided for three inoperable cases, and 52 patients (24.2%) had relapse of disease at the time of the last follow-up. The median follow-up time for all patients was 86 months (1-141).
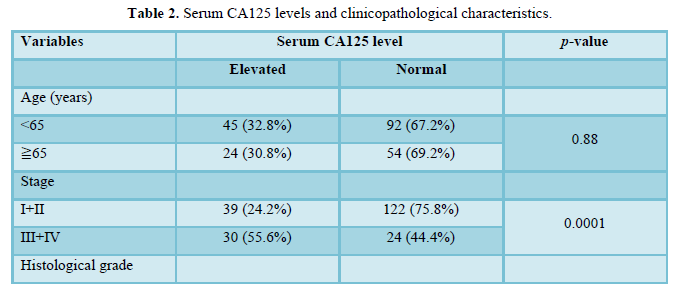
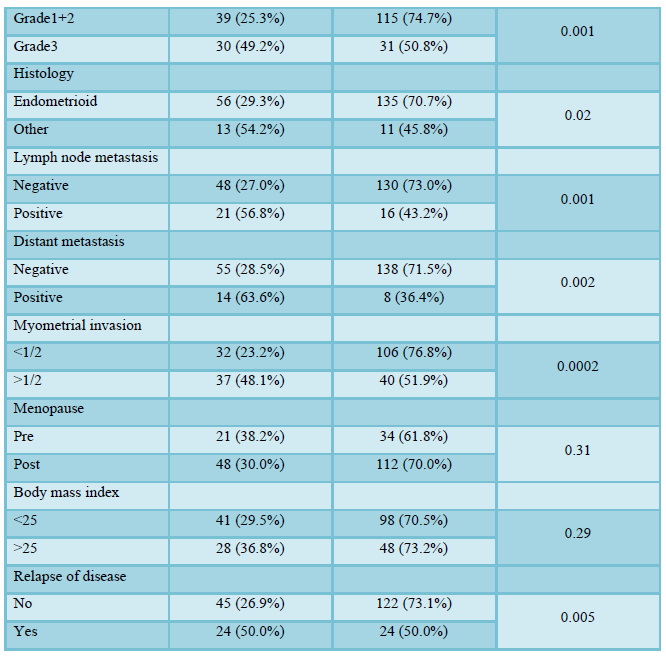
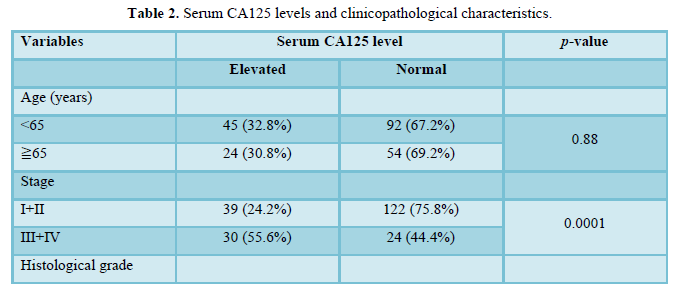
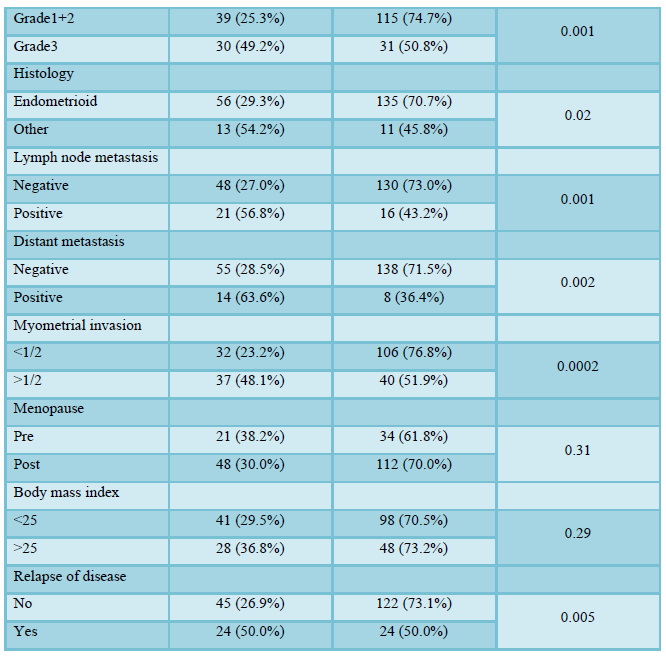
Serum CA125 level in patients with endometrial cancer
Serum CA125 levels and clinical characteristics are shown in Table 2. Elevated serum CA125 levels were detected in 69 patients (32.1%), and were significantly more elevated in patients with histological grade 3 (49.2%) disease than in those with grades 1 and 2 (25.3%) disease (p = 0.001). Serum CA125 levels were significantly elevated in patients with myometrial invasion depth > 1/2 (48.1%) than in those with myometrial invasion depth <1/2 (23.2%) (p=0.0002). Moreover, serum CA125 levels were significantly elevated in patients with lymph node metastasis (56.8%) than in those without lymph node metastasis (27.0%) (p=0.001), and elevated in patients with distant metastasis (63.6%) than in those without distant metastasis (28.5%) (p=0.002). Therefore, serum CA125 levels were significantly elevated
in patients with stage III+IV (55.6%) than in patients with stage I+II (24.2%) (p=0.0001). Elevated serum CA125 levels were not associated with age, menopausal status, or body mass index (BMI).
Among the 69 patients with elevated serum CA125 levels,
56 (81.2%) achieved remission and serum CA125 levels returned to the normal range in all cases. Eleven patients (19.6%) had relapses among these patients and serum CA125 level has been elevated again in 8 (72.7%) cases. Although the patients with elevated serum CA125 levels had significantly frequent relapse of disease (50.0%) more than the patients with normal level (26.9%) (p=0.005), there is no statistically significant relationship between an elevated serum CA125 levels and OS (p=0.06).
DISCUSSION
Numerous studies investigate biomarkers for endometrial cancer [1-8]. In particular, measurement of serum CA125 as a tumor marker has been investigated in patients with endometrial cancer. Duk [6] reported that CA125 was a useful marker in endometrial carcinoma and Patsner [7] demonstrated its utility as a marker for monitoring treatment effects in patients with advanced endometrial cancer. However, the precise roles of CA125 in preoperative evaluations of endometrial cancer patient remain uncharacterized and controversial [6-8]. Nonetheless, no other potential tumor markers have been validated for prognosis and classification of endometrial cancers, warranting identification of tumor markers that can inform the management of patients with endometrial cancer.
In the present study, elevated serum CA125 levels were identified in 69 patients (32.1%) with endometrial cancer.
Serum CA125 levels were significantly elevated in patients with stage III+IV (55.6%) than in patients with stage I+II (24.2%) (p=0.0001). In general, 15% to 25% of patients with disease that is clinically confined to the uterus have elevated serum CA125 levels [6-8], whereas approximately 75% of patients with metastatic disease have elevated serum CA125 levels [7]. Our data is similar with previous reports.
The present study also shows that significantly elevated serum CA125 levels were more common (49.2%) among patients with histological grade3 than in those with grades 1 and 2 (25.3%; p=0.001). Elevated serum CA125 levels were also significantly more prevalent in patients with myometrial invasion depth >1/2 (48.1%) than in those with myometrial invasion depth < 1/2 (23.2%; p=0.0002). Moreover, serum CA125 levels were more common (56.8%) among patients with lymph node metastasis than in those without lymph node metastasis (27.0%; p=0.001), and more common (50.0%) among patients with distant metastasis (63.6%) than in those without distant metastasis (28.5%; p=0.002). However, elevated serum CA125 levels were not associated with age, menopausal status, or body mass index (BMI). In agreement, Sood [3] reported that CA125 correlated with higher stage, higher grade, increased depth of myometrial invasion, and pelvic or para-aortic lymph node metastases. Our data is similar with these data and strongly support the prognostic value of serum CA125 levels. Thirty-two patients had myometrial invasion depths of <50% and concomitantly elevated serum CA125 levels, four of these patients (12.5%) had lymph node metastases. Hence, after preoperative diagnosis of stage IA endometrial cancer using CT or MRI examinations, lymphadenectomy may be indicated for patients with elevated serum CA125 levels. However, measurements of CA125 may not provide further prognostic information after surgical risk stratification.
Fifty-six of 69 patients (81.2%) with elevated serum CA125 levels specifically achieved remission, and serum CA125 levels fell below the normal range in all cases. Eleven patients (19.6%) had relapses among these patients and serum CA125 level has been elevated again in 8 (72.7%) cases. Moreover, in seven cases of eleven relapsing patients (19.6%), serum CA125 levels were again elevated, indicating that CA125 levels may reflect disease status. Therefore, serum CA125 levels may facilitate management of endometrial cancer patients with elevated serum CA125 levels.
CONCLUSION
This study strongly indicates the potential of CA125 as a clinically useful prognostic factor for endometrial cancer.
CONFLICT OF INTERESTS
The authors declare that they have no competing interests.
-
Lo SS, Cheng DK, Ng TY, Wong LC, Ngan HY (1997) Prognostic significance of tumor markers in endometrial cancer. Tumour Biol 18: 241-249.
-
Kurihara T, Mizunuma H, Obara M, Andoh K, Ibuki Y, et al. (1998) Determination of a normal level of serum CA125 in postmenopausal women as a tool for preoperative and postoperative surveillance of endometrial carcinoma. Gynecol Oncol 69: 192-196.
-
Sood AK, Buller RE, Burger RA, Dawson JD, Sorosky JI, et al. (1997) Value of preoperative CA125 level in the management of uterine cancer and prediction of clinical outcome. Obstet Gynecol 90: 441-447.
-
Kaku T, Kamura T, Hirakawa T, Sakai K, Amada S, et al. (1999) Endometrial carcinoma associated with hyperplasia-immunohistochemical study of angiogenesis and p53 expression. Gynecol Oncol 1: 51-55.
-
Yasa C, Takmaz O, Dural O, Akhan SE (2013) The value of tumor markers in endometrial carcinoma: Review of literature. J Cancer Ther 4: 966-970.
-
Duk JM, Aalders JG, Fleuren GJ, Bruijn HW (1986) CA125: A useful marker in endometrial Am J Obstet Gynecol 155: 1097-1102.
-
Patsner B, Mann WJ, Cohen H, Loesch M (1998) Predictive value of preoperative serum CA 125 levels in clinically localized and advanced endometrial carcinoma. Am J Obstet Gynecol 158: 399-402.
-
Patsner B, Yim GW (2013) Predictive value of preoperative serum CA-125 levels in patients with uterine cancer: The Asian experience 2000 to 2012. Obstet Gynecol Sci 56(5): 281-288.
-
Pecorelli S (2010) Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet 108(2):
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- BioMed Research Journal (ISSN:2578-8892)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Advance Research on Alzheimers and Parkinsons Disease
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Allergy Research (ISSN:2642-326X)


