5967
Views & Citations4967
Likes & Shares
Abbreviations: IDF: International Diabetes Federation; AFR: Africa; EUR: Europe; MENA: Middle East and North Africa; NAC: North America and Caribbean; SACA: South and Central America; SEA: South-East Asia; WP: Western Pacific
There are different diagnosing procedure for diabetes that are based on plasma glucose criteria, either the fasting plasma glucose (FPG) value or the 2 h plasma glucose (2 h PG) value during a 75 g oral glucose tolerance test (OGTT) or A1C criteria. The number of people with diabetes is increasing due to population growth, aging, urbanization, and increasing prevalence of obesity and physical inactivity [12-14]. Regular screening of adults is essential for early detection and care [15].
STATISTICS
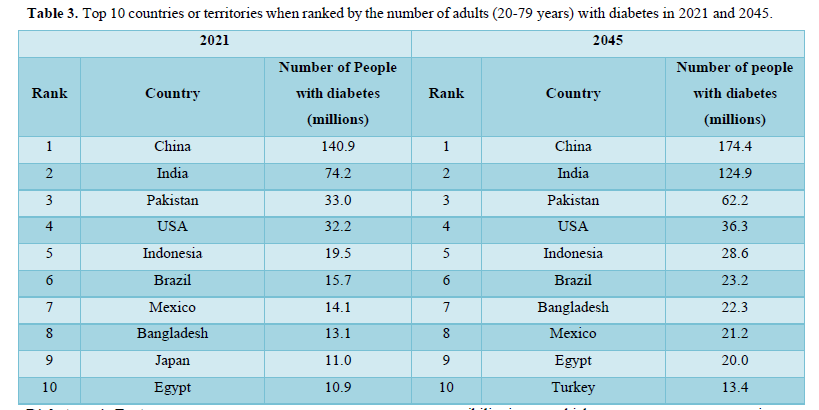
Diabetes mellitus (DM) is fastest growing global health emergencies of the 21st century that affects one in every ten of human population [16-18]. The prevalence of diabetes worldwide increases yearly and about half a billion people are living with diabetes [17,19]. The top 10 countries with all types of diabetic patient in the years 2021 and 2045 are shown in Table 3. China is on top with 140 million diabetic patient in 2021 and Pakistan on third with 33 million people with diabetes. The prevalence of DM was 10.5% (536.6 million people) in 20-79 year olds in 2021, rising to 12.2% (783.2 million) in 2045 [18,19]. Diabetes prevalence was similar in both genders equally and highest in old aged person. According to reports of IDF in 2021 the prevalence of DM was estimated 12.1% in urban and 8.3%in rural areas, whereas 11.1% in well-developed countries as compared to 5.5% in under-developed countries. It is expected that in 2045 the prevalence of diabetes relatively increase in middle-income countries by 21.1% compared to 12.2% in high-income and 11.9% in low-income countries. Developing countries encounters 80% of the diabetes disease burden with high portion of diabetes type 2 [17]. The estimated outbreak of diabetes in adults aged 20–79 years has more than tripled since 2000, from an estimated 151 million about 4.6% of global population to 537 million that 10.5% today human population [17,20]. It has been predict 643 million people will have diabetes by 2030 (11.3% of the population) and 783 million (12.2%) by 2045 [16]. WHO estimates that between 2000 and 2030, the world population will increase by 37% and the number of people with diabetes will increase by 114%. About 90% of people with undiagnosed diabetes live in developing, low- and middle income countries [16]. World diabetes-related health expenditures were 966 billion USD in 2021 and projected 1,054 billion USD by 2045 (Table 1) [19].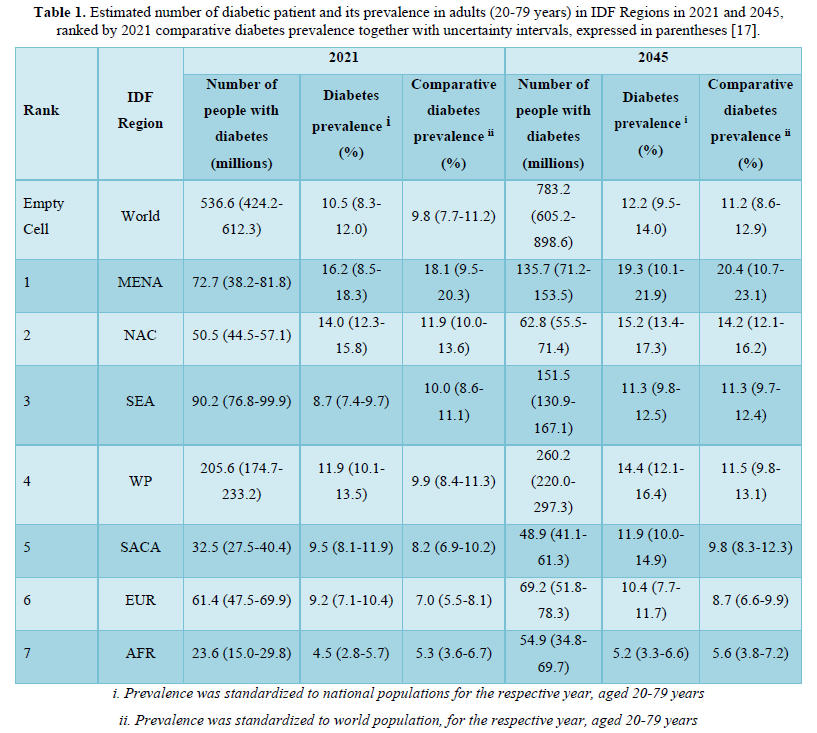
Like other developing countries in South Asia, Pakistan - the fifth most populous country with about more than 229 million population in the world and third highest number of people living with diabetes in the world with 33 million (2021- IDF) adults in Pakistan are living with diabetes - a 70% increase since 2019[16-20]. In 2021, 400,000 deaths in the country due to diabetes. About 11 million adults have Impaired Glucose Tolerance (IGT) that places them at high risk of developing type 2 diabetes [17]. Pakistan has 25% diabetes prevalence in adults. Table 2 shows the top ten countries with the highest comparative prevalence for the years 2021 and 2045. All top ten countries have prevalence of more than 20% but the country with the highest prevalence at 31% is Pakistan which is projected to have a prevalence of over 34% in 2045 [17], Top most causes of blindness and kidney failure in Pakistan is diabetes. Diabetes is the 7th leading cause of disability in all adults and 8th causing factor of deaths in all age groups. Almost 4% of pregnant women have diabetes but only 30% women in rural areas are tested for diabetes in pregnancy (Table 3) [17].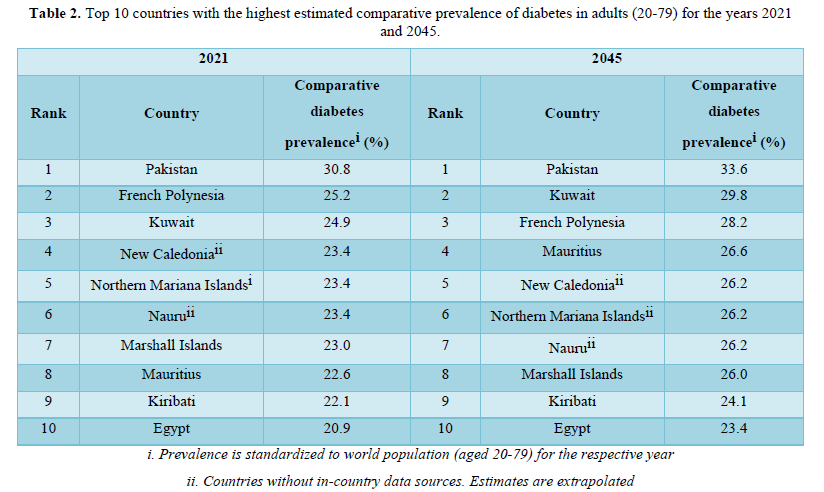
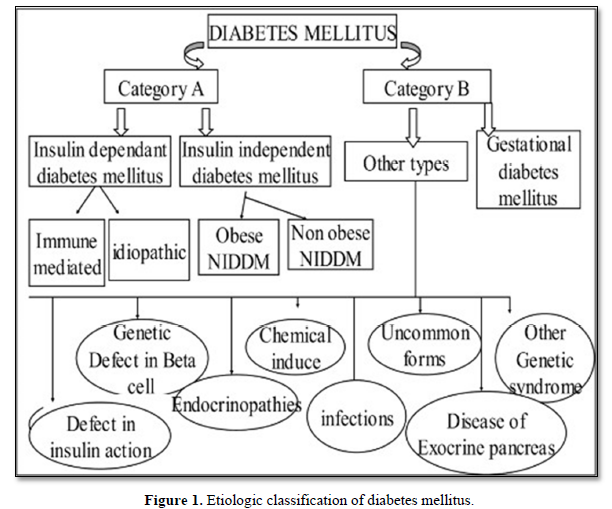
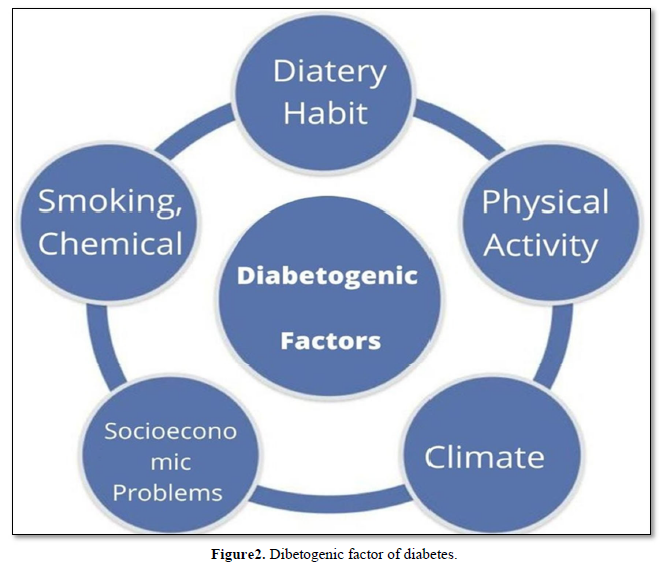
Diabetogenic Factors
The etiology of diabetes in Pakistan is multifactorial disease that can be cause by many factor including genetic susceptibility and environmental factors [21]. Genetic susceptibility is ones which are connect to our gene or it may cause by inheritance and also some epigenetic factor [21]. The genetic factors are related to mutation or single nucleotide polymorphisms while the epigenetic factors include gene methylation, histone modification as well as microRNAs [11]. But along with diabetes has been a chronic disease with a powerful impact on our environment factors such as climate, dietary habits, food production, manufacturing and marketing, social networks, viral infection, psychosocial factors, health services, belief, urbanization, globalization, industrialization and economic transition [13,14,22-28]. That why diabetes is also known as paradigmatic social disease. Diabetes mellitus is usually correlated with its complicated side effect [29]. In Pakistan Due to ignorant and illiterate diabetes since from the being, there has been an increase in its complications along with diabetes (Figure 2) [29].
Climate
Climate change and diabetes are interlinked with each other’s. Temperatures changes can provoke a person's susceptibility to suffers diabetes as well as impose adverse outcomes on those who already diagnosed with diabetes (such as increased incidence of hospitalization, dehydration and mortality) [30]. During extreme heat conditions diabetic patients are at greater possibility of facing cardiovascular and dehydration events. Increase in temperature is directly effect on chance of cardiovascular event and heat related for people living with diabetes. Sudden alter in temperature can affect insulin requirement. Cold weather, can raise insulin need while warm weather, by contrast insulin demands might drops down. Extreme temperatures changes in the body that may lead to a drop or spike in blood sugar. Climates of Pakistan are more dangerous for diabetes sufferers.
Dietary Habits
To maintain a healthy nutritional status at any age is very important. Diabetes mellitus (DM) is a metabolic disease with many systemic complications that can be prevented by dietary modifications and physical exercise. Unhealthy diet is very important factor that contributes toward the diabetes specially type 2 diabetes [31]. Making healthier food choices is important to manage your diabetes and to reduce your risk of diabetes complications [32]. Due to poverty the majority of population living in both urban and rural areas in Pakistan is unable to meet their basic diet and nutrients requirements. The nutritional status and food intake pattern of the population can be affected by various health-related changes. Despite these changes, a healthy lifestyle and proper nutrition can improve the quality of life and nutritional status among the population. Nutrition and physical activity are important parts of a healthy lifestyle when you have diabetes. To manage your blood glucose level, you need to balance what you eat and drink with healthy physical activity and diabetes medicine. There is sufficient evidence that long-term consumption of high fat and sugar rich foods can contribute to diabetes in low and middle income countries like Pakistan [33]. DM are also associated with the deficiency of vitamin D [25,34], lack of sun light exposure [25].
Physical activity
Physical activity has been measured to shrink mortality rates in different population with diabetes mellitus [35] because during exercise, our cells become more sensitive to insulin so it works more effectively to lower your blood glucose. Healthy physical exercise directly effect on the insulin production and blood glucose management [36]. Physical activity has the potential of improving insulin action and resistance and is, therefore, play important role in prevention and treatment of diabetes [37]. Physical activity, sports and exercise should be supported in all persons with diabetes [36,38]. Healthy diet and regular exercise can delay diabetes [39]. The clinical trial proved that a low-fat diet, combined with a walking or other low-intensity exercise daily, decrease the risk of developing diabetes type 2 by 58 percent [39]. As diabetes has become age related disease because of the lack of physical activities in old age. The diabetes patients showed a low level of motivation and they were more unwilling in doing physical activity as they had pain and swelling of feet whenever they started physical activity [29]. Pakistan being an under developing country, most of the population are under poverty so these rick factor may contributes to DM.
Socioeconomic problems
The exponentially prevalence of diabetes seen in the last decade can be attributed mostly as a result of rapid socioeconomic growth to the change in lifestyle [40]. Diabetic patient had to face socioeconomic issues from the society and family that leads them more depressed and early fatigue [29]. The increase in urban population, aging and socioeconomic growth are the main determinants of the rise in prevalence of diabetes in developing world [40,41]. Scio-economic status also contributes to DM prevalence such as education and income, has been associated with increased risk of diabetes [26,27,42]. Current meta-analysis reported that due to illiteracy [42]. Occupational class or status, poverty, and income was associated with DM with almost 30-40 % higher risk [26,27]. Physiological factor mays also cause complication with diabetes such as hypertension, stress and depression [28,43,44] It is estimated that the substantial increase in urbanization, socioeconomic problem in Pakistan might be the risk for diabetes.
Smoking and alcohol drinking
The prevalence of diabetes is to be 45% higher in smokers than among nonsmokers [45]. Smoking and alcohol are also causing factor for diabetes type 2 [24]. Smoking increases the risk of central obesity and insulin resistance and nicotine exposure has several other deleterious effects. Asian countries such as China and India continue to produce and consume tobacco products and hence face a huge public health problem. The increasing use of alcohol in Asian countries, especially among the middle class and rural population, also increases the risk for diabetes and other metabolic diseases.
Pollution and chemicals
Pollution and environmental toxicants acting as endocrine-disrupting chemicals (EDCs) are emerged as novel metabolic diabetes risk factors. Long term exposure to air pollution and endocrine-disrupting chemicals (EDCs) create a high chance of getting DM [46,47]. It has been reported that there is positive associations for prevalence of DM with exposure of nitrogen dioxide (NO2) [48], polycyclic aromatic hydrocarbons (PAHs) [49,50], perfluoroalkyl substances (PFAS) metabolites [51,52], lead, cadmium, mercury, selenium [53], Phenols and phthalates (PAEs) [48,54], Persistent Organic Pollutants (POPs) (including dioxins, polychlorinated biphenyl (PCBs) and organochlorine pesticides (OCPs)) [55,56], arsenic [47,57]. These chemicals and pollutants are highly concentrated in the atmosphere especially in the populated cites of Pakistan.
Complication of diabetes
Diabetes mellitus also have serve complication that can be cause if the diabetic syndrome are prolonged or due to no medication or prevention from diabetogenic factors [3,58-60]. The complication may be chronic or acute vary from person to person. Several complication of diabetes mellitus is nephropathy, which is damage or disease of the kidney, retinopathy (loss of vision), peripheral neuropathy (risk of foot ulcer) [60], periodontal diseases (bone and tissue supporting teeth), sexual dysfunction, and autonomic neuropathy cause gastrointestinal, cardiovascular disorder and genitourinary [59]. If a diabetic patient don’t take an account of the factor that contribute diabetes than there is greater chance of getting these complication.
CONCLUSION
The prevalence of diabetes mellitus in the population of Pakistan is very high and increases at an uncontrollable rate. These environmental factors contribute large proportion in the diabetes prevalence. Moreover, being an under develop country Pakistan doesn’t have a well-developed medical care system for any diseases. By controlling and managing these factors prevalence can be reduced. That as a under developed country Pakistan must take into account of these environmental factor that are becoming a risk factor for the high prevalence of diabetes.
- Frank LL (1957) Diabetes mellitus in the texts of old Hindu medicine (Charaka, Susruta, Vagbhata). Am J Gastroenterol 27(1): 76-95.
- Ahmed AM (2002) History of diabetes mellitus. Saudi Med J 23(4): 373-378.
- Riaz S, Alam SS (2012) Study of Diabetic Hypertensive Nephropathy in the Local Population of Pakistan in Diabetic Nephropathy. IntechOpen 9: 147-166.
- Egan AM, Dinneen SF (2019) What is diabetes? Medicine 47(1): 1-4.
- Association AD (2019) Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care 43(Supplement_1): S14-S31.
- Kiani AK, John P, Bhatti A, Zia A, Shahid G, et al. (2015) Association of 32 type 1 diabetes risk loci in Pakistani patients. Diabetes Res Clin Pract 108(1): 137-142.
- Association AD (2020) Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2021. Diabetes Care 44(Supplement_1): S15-S33.
- McIntyre HD, Catalano P, Zhang C, Desoye G, Mathiesen ER, et al. (2019) Gestational diabetes mellitus. Nat Rev Dis Primers 5(1): 47.
- Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH (2018) The Pathophysiology of Gestational Diabetes Mellitus. Int J Mol Sci 19(11): 3342.
- Sweeting A, Wong J, Murphy HR, Ross GP (2022) A Clinical Update on Gestational Diabetes Mellitus. Endocr Rev 43(5): 763-793.
- Dalrà MG, Burlina S, Del Vescovo GG, Lapolla A (2020) Genetics and Epigenetics: New Insight on Gestational Diabetes Mellitus. Front Endocrinol (Lausanne) 11: 602477.
- Frank LD, Adhikari B, White KR, Dummer T, Sandhu J, et al. (2022) Chronic disease and where you live: Built and natural environment relationships with physical activity, obesity, and diabetes. Environ Int 158: 106959.
- Gary-Webb TL, Suglia SF, Tehranifar P (2013) Social Epidemiology of Diabetes and Associated Conditions. Curr Diab Rep 13(6): 850-859.
- Golden SH, Brown A, Cauley JA, Chin MH, Gary-Webb TL, et al. (2012) Health Disparities in Endocrine Disorders: Biological, Clinical, and Nonclinical Factors-An Endocrine Society Scientific Statement. J Clin Endocrinol Metab 97(9): E1579-E1639.
- Muninarayana C, Balachandra G, Hiremath SG, Iyengar K, Anil NS (2010) Prevalence and awareness regarding diabetes mellitus in rural Tamaka, Kolar. Int J Diabetes Dev Ctries 30(1): 18-21.
- Federation ID (2021) IDF Diabetes Atlas, 10th
- Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, et al. (2019) Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th Diabetes Res Clin Pract 157: 107843.
- Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, et al. (2022) IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract 183: 109119.
- Federation IDJ (2015) IDF Diabetes atlas 9th
- Lone IM, Iraqi FA (2022) Genetics of murine type 2 diabetes and comorbidities. Mamm Genome 33(3): 421-436.
- Zorena K, Michalska M, Kurpas M, Jaskulak M, Murawska A, et al. (2022) Environmental Factors and the Risk of Developing Type 1 Diabetes & Old Disease and New Data. Biology (Basel) 11(4): 608.
- Taha-Khalde A, Haim A, Karakis I, Shashar S, Biederko R, et al. (2021) Air pollution and meteorological conditions during gestation and type 1 diabetes in offspring. Environ Int 154: 106546.
- Na J, Chen H, An H, Ren M, Jia X, et al. (2022) Passive Smoking and Risk of Gestational Diabetes Mellitus among Nonsmoking Women: A Prospective Cohort Study in China. Int J Environ Res Public Health 19(8): 4712.
- Sørensen IM, Joner G, Jenum PA, Eskild A, Brunborg C, et al. (2016) Vitamin D‐binding protein and 25‐hydroxyvitamin D during pregnancy in mothers whose children later developed type 1 diabetes. Diabetes Metab Res Rev 32(8): 883-890.
- Dray-Spira R, Gary-Webb TL, Brancati FL (2010) Educational disparities in mortality among adults with diabetes in the US. Diabetes Care 33(6): 1200-1205.
- Robbins JM, Vaccarino V, Zhang H Kasl SV (2005) Socioeconomic status and diagnosed diabetes incidence. Diabetes Res Clin Pract 68(3): 230-236.
- Katon WJ, Rutter C, Simon G, Lin EHB, Ludman E, et al. (2005) The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care 28(11): 2668-2672.
- Nazeer T, Tahir A, Din ST, Asif M, Alam A, et al. (2020) Level of physical activity among diabetic patients of rural and urban areas. Pak J Med Health Sci 14(1): 219-222.
- Cuschieri S, Agius JC (2021) The interaction between diabetes and climate change - A review on the dual global phenomena. Early Hum Dev 155: 105220.
- Riaz S (2018) Therapeutic Implication of Folate-Homocysteine Interaction in the Local Diabetic Pakistani Population. Ann Vasc Med Res 5(1): 1085-1089.
- Alam SS, Riaz S (2015) Thiamine and the Cellular Energy Cycles-A Novel Perspective on Type 2 Diabetes Treatment, in Treatment of Type 2 Diabetes. IntechOpen.
- Ahmed J, Rehman SU, Mughal F (2016) Assessment of dietary behavior of high school students of an urban setting in Pakistan. Int J Health Sci 10(4): 548-555.
- Lai G-R, Lee Y-F, Yan S-J, Ting H-J (2020) Active vitamin D induces gene-specific hypomethylation in prostate cancer cells developing vitamin D resistance. Am J Physiol Cell Physiol 318(5): C836-C847.
- Karnadipa T, Nurfikri A, Arifin S (2022) Telehealth to Improve Physical Activity in Adults with Diabetes Mellitus: A Narrative Review. Jurnal Aisyah: Jurnal Ilmu Kesehatan 7(2): 615-622.
- Hu EA, Pan A, Malik V, Sun Q (2012) White rice consumption and risk of type 2 diabetes: Meta-analysis and systematic review. BMJ 344: e1454.
- Lee-Ødegård S, Olsen T, Norheim F, Drevon CA, Birkeland KI (2022) Potential Mechanisms for How Long-Term Physical Activity May Reduce Insulin Resistance. Metabolites 12(3): 208.
- Kalra S, Jacob J (2019) Activity day rules in diabetes. J Pak Med Assoc 69(12): 1919-1921.
- Wu JH, Micha R, Imamura F, Pan A, Biggs ML, et al. (2012) Omega-3 fatty acids and incident type 2 diabetes: A systematic review and meta- analysis. Br J Nutr 107(S2): S214-S227.
- Ramachandran A, Snehalatha C, Shetty AS, Nanditha A (2012) Trends in prevalence of diabetes in Asian countries. World J Diabetes 3(6): 110-117.
- Shokat S, Riaz A, Iqbal R, Yaqub A, Riaz S (2022) Statistical Evaluation of Environmental Factors as Diabetogenic Agent in Type 2 Diabetes Mellitus. Int J Innov Sci Technol 4(1): 288-299.
- Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A (2011) Type 2 diabetes incidence and socio-economic position: A systematic review and meta-analysis. Int J Epidemiol 40(3): 804-818.
- Chida Y, Hamer M (2008) An association of adverse psychosocial factors with diabetes mellitus: A meta-analytic review of longitudinal cohort studies. Diabetologia 51(12): 2168-2178.
- Golden SH (2007) A review of the evidence for a neuroendocrine link between stress, depression and diabetes mellitus. Curr Diabetes Rev 3(4): 252-259.
- Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J (2007) Active smoking and the risk of type 2 diabetes: A systematic review and meta- analysis. JAMA 298(22): 2654-2664.
- Arslan M, Ikram M, Zahid R, Riaz S (2021) Type 3c Diabetes. A New Challenge of 2021 to Diabetologists. Int J Clin Stud Med Case Rep 13(2): 1-7.
- Matti HA, Shokat S, Iqbal R, Zubair M, Riaz S (2022) Evaluation of Environmental Influence of Arsenic Compounds on Patients Suffering From Type 2 Diabetes. Int J Probiotics and Dietetics 2(1): 23-28.
- Park SK, Adar SD, O'Neill MS, Auchincloss AH, Szpiro A, et al. (2015) Long-Term Exposure to Air Pollution and Type 2 Diabetes Mellitus in a Multiethnic Cohort. Am J Epidemiol 181(5): 327-336.
- Stallings-Smith S, Mease A, Johnson TM, Arikawa AY (2018) Exploring the association between polycyclic aromatic hydrocarbons and diabetes among adults in the United States. Environ Res 166: 588-594.
- Yang L, Zhou Y, Sun H, Lai H, Liu C, et al. (2014) Dose-response relationship between polycyclic aromatic hydrocarbon metabolites and risk of diabetes in the general Chinese population. Environ Pollut 195: 24-30.
- He X, Liu Y, Xu B, Gu L, Tang W (2018) PFOA is associated with diabetes and metabolic alteration in US men: National Health and Nutrition Examination Survey 2003-2012. Sci Total Environ 625: 566-574.
- Sun Q, Zong G, Valvi D, Nielsen F, Coull B, et al. (2018) Plasma Concentrations of Perfluoroalkyl Substances and Risk of Type 2 Diabetes: A Prospective Investigation among U.S. Women. Environ Health Perspect 126(3): 037001.
- Wei H, Sun J, Shan W, Xiao W, Wang B, et al. (2022) Environmental chemical exposure dynamics and machine learning-based prediction of diabetes mellitus. Sci Total Environ 806: 150674.
- Sargis RM, Simmons RA (2019) Environmental neglect: Endocrine disruptors as underappreciated but potentially modifiable diabetes risk factors. Diabetologia 62(10): 1811-1822.
- Wolf K, Bongaerts BWC, Schneider A, Huth C, Meisinger C, et al. (2019) Persistent organic pollutants and the incidence of type 2 diabetes in the CARLA and KORA cohort studies. Environ Int 129: 221-228.
- Heindel JJ, Blumberg B, Cave M, Machtinger R, Mantovani A, et al. (2017) Metabolism disrupting chemicals and metabolic disorders. Reprod Toxicol 68: 3-33.
- Nizam S, Kato M, Yatsuya H, Khalequzzaman Md, Ohnuma S, et al. (2013) Differences in Urinary Arsenic Metabolites between Diabetic and Non-Diabetic Subjects in Bangladesh. Int J Environ Res Public Health 10(3): 1006-1019.
- Nibali L, Gkranias N, Mainas G, Di Pino A (2022) Periodontitis and implant complications in diabetes. Periodontol 2000 90(1):88-105.
- Pop-Busui R, Januzzi JL, Bruemmer D, Butalia S, Green JB, et al. (2022) Heart Failure: An Underappreciated Complication of Diabetes. A Consensus Report of the American Diabetes Association. Diabetes Care 45(7): 1670-1690.
- Matoori S (2022) Diabetes and its Complications. ACS Pharmacol Transl Sci 5: 513-515.
- Migdalis IN, Czupryniak L, Lalic N, Papanas N, Valensi P (2022) Chronic diabetic complications: Current challenges and opportunities. J Clin Med 11(3): 673.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- BioMed Research Journal (ISSN:2578-8892)
- Chemotherapy Research Journal (ISSN:2642-0236)




