Research Article
Assessment of the Diabetes Management Capacities of Bamako - Mali Hospital Structures
4209
Views & Citations3209
Likes & Shares
Context: The demographic growth of the city of Bamako estimated at 5.4% (RGPH 2009) is higher than the national average (3.4%). The outlook for the period 2006-2020 shows that Bamako will experience the strongest annual growth of all African agglomerations. By 2025, more than 3 million inhabitants will reside in Bamako. This growth is accompanied by environmental changes leading to changes in people's lifestyles, especially food. The consequences can be the rise of obesity, overweight and diabetes which begins to weigh on the Malian health system.
Objective: Analyze the diabetes-related health offer in public health services (reference health centers (CSREF), hospitals in the district of Bamako in Mali.
Methods: Retrospective cross-sectional study focused on data from January to December 2019 with 10 health structures which were (04 Hospitals; 06 CSREF).
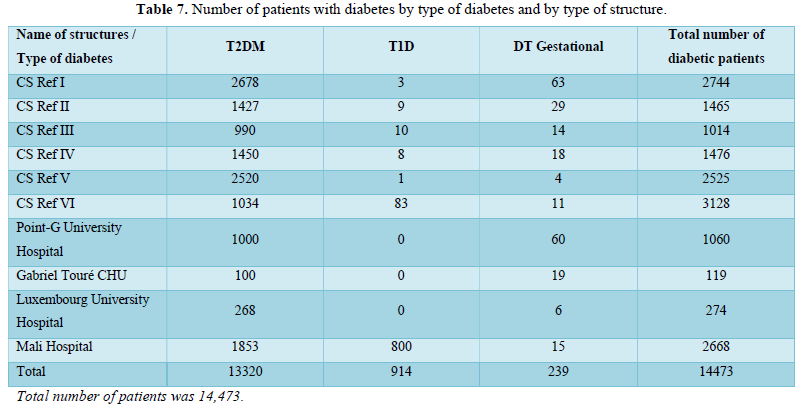
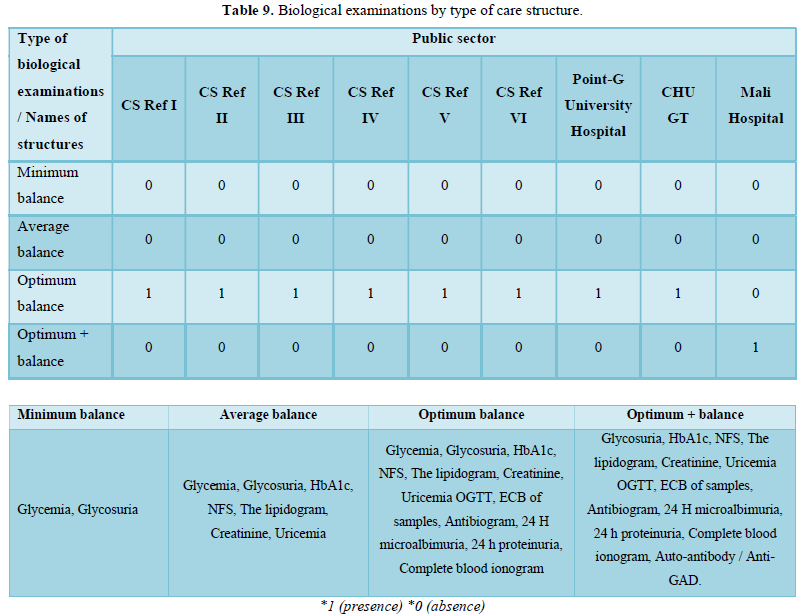
Results: All 10 structures surveyed are from the public sector. Diabetes screening and management were effective in these structures. Of these 10 structures, 06 were CSRefs and 04 were hospitals. Diabetes care in the CSRefs and hospitals was provided by at least an endocrinologist and / or a diabetologist (10 structures and 18 specialists). It was noted that there were no specialists at the primary level (CSCom). The active file of diabetic patients was estimated at 14,473 patients in the 10 structures.
Conclusion: This research made it possible to identify the process of managing diabetes in Bamako. Identify the capacities and existing gaps between the different structures but also the multiple underlying constraints. This study could facilitate the planning of capacity building actions and the technical platform of health structures. Allow, to overcome some of the difficulties raised, to amplify the impact of the actions targeted on the optimization of the management of diabetes in Mali.
Keywords: Diabetes, Health offer, Health structures, Bamako
INTRODUCTION
Mali is considered one of the poorest countries in the world, ranked 175th out of 188 countries according to the UNDP Human Development Index [1]. The population of Mali in 2009 is estimated at 14,517,176 inhabitants, 49% of whom are men and 51% women (DNSI, RGHP 2009). The majority of the population is rural 73.2% against 26.8% of the urban population. She is relatively young with 46.06% under 15 years old and 42.92% between 15 and 49 years old. The demographic growth of the city of Bamako estimated at 5.4% is higher than the national average (3.4%) [2]. The outlook for the period 2006-2020 shows that Bamako will experience the strongest annual growth of all African agglomerations, thus ranking 6th globally. By 2025, more than 3 million inhabitants will reside in the urban area of Bamako [3].
Faced with these food and environmental issues, awareness has emerged in the health services and the ministries concerned: a strategic plan to fight against non-communicable diseases is being drawn up in Mali [4]. Despite the goodwill displayed by the players in the sector, this situation prevents the definition of clear guidelines and intervention or prevention programs. This necessary approach is however made difficult by the lack of reliable health data related to cardiovascular disease and associated risk factors such as nutrition, physical exercise and the availability of drugs [5]. Previous studies have shown that in most cases diabetes was diagnosed at the stage of acute complications, which was responsible for significant morbidity and mortality in the absence of appropriate and early treatment [6,7]. Their appropriate management posed enormous problems due to:
- delay in diagnosis;
- lack of training of health personnel and specialists;
- insufficient adequate technical platform;
- high individual and collective cost of care.
- lack of education for diabetics and their social environment.
It is therefore essential today to assess the precise situation of the food and health environment in the hospital structures of the district of Bamako. The model developed offers a comprehensive approach to the hospital system while integrating the perceptions of the various health professionals [8].
To achieve this end, our study focused on diabetes, which is a result of this nutritional transition, will allow the development of recommendations and advocacy for better consideration of these issues in public policies. An in-depth analysis of secondary data from health structures and an estimate of the size of the number of diabetic people treated in Bamako would allow a better definition of public policies aimed at better addressing the public health problems linked to diabetes.
OBJECTIVES
- Main objective: Carry out an inventory of diabetes cases taken care of and analyze the capacities of hospital structures in the district of Bamako.
- Specific objectives
- Inventory the cases of diabetes treated in hospital structures in Bamako
- Evaluate the diabetes care offer in hospital structures in Bamako.
METHODOLOGY
The study took place in several stages:
- The first stage of the project involved carrying out a literature review on the subject, followed by the drafting of an exploratory pilot study protocol on diabetes in Bamako. Then thanks to this review, a draft of the diabetes questionnaire was written by the research team.
- The second step was to recruit and train a medical thesis student. During the training, he familiarized himself with the content of the collection tool. This made it possible to readjust the questionnaire, to establish a back-planning of the handing-over of documents, but also to supervise the material organization of the survey.
Study setting, study type and population
This is a retrospective cross-sectional study carried out from March to June 2020, focused on data from January to December 2019. The study took place in the district of Bamako and concerned 10 hospital structures selected systematically:
- 04 Hospitals (Point G and GT, Hospital du Mali and Luxembourg)
- 06 CSREF (I, II, III, IV, V, VI).
We considered that this sample was representative of the diversity of the public hospital care offer in the city of Bamako. A pre-survey step was to send an awareness letter by mail to the 10 selected structures targeting both those in charge of these structures but also the doctors who had to answer questions.
Data collection
The last step was to pass the questionnaire through the 10 structures. The data was collected from the referring physicians through interviews via a questionnaire and completed with registers or patient files. All 10 Questionnaires have been completed. The following information was collected systematically by structure:
- In each structure surveyed (Presence or not of screening or diabetes care). The structures that could do the screening were those that had (blood glucose meters, scales, height gauges, blood pressure monitors). The structures that could do screening and PEC were those that had (blood glucose meters, scales, height gauges, blood pressure monitors, BMI disc, tape measure, diabetic foot care equipment and HBA1c device).
- The human resources present in the structures for support. Here we are interested in the nature of the formation and the number by structure and overall.
- The data collected were:
- Specialists (endocrinologists, diabetologist)
- General practitioners trained or not
- Other specialties (internists).
- Presence or not and the human resources present in the structures for the laboratory and the pharmacy if they existed (pharmacist, biologist, laboratory assistant, manager and others). The interest was to know what type of professional would manage the laboratory
- The data collected were:
- Technical platform
- Availability or not of equipment related to screening and diagnosis (reading blood glucose, HbA1c, blood pressure monitor, scale and tape measure)
- Availability or not of equipment related to complications example of the foot kit (dressing box, nail clipper, hand and foot treatment, scissors, sensor and adapter, cuffs and toe inflator etc.)
- Availability or not of equipment related to TVE (DVD player, television set, station, BAI (Picture box) and the prevention guide)
- Presence or absence of data collection tools (diabetes consultation register, patient file (paper or electronic) and reporting framework)
- Support data:
- Number of patients by type of diabetes and by structure;
- Complication related to diabetes;
- Type of biological examination part type of structure ensuring the PEC of diabetes.
- Medicines:
- Presence or absence of oral antidiabetics and insulin
- Presence or absence of antihypertensive drugs
- Sources of supply.
Statistical analyzes and studied variables
Statistical analysis of the data was performed using SPSS software and exported to Excel.
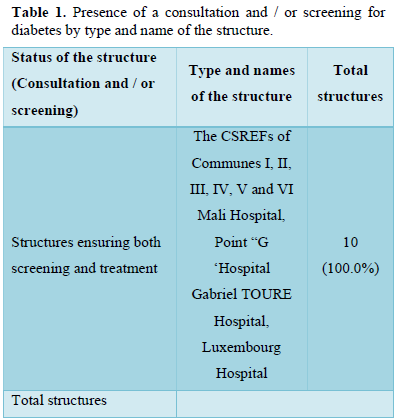
RESULTS (Tables 1-11)
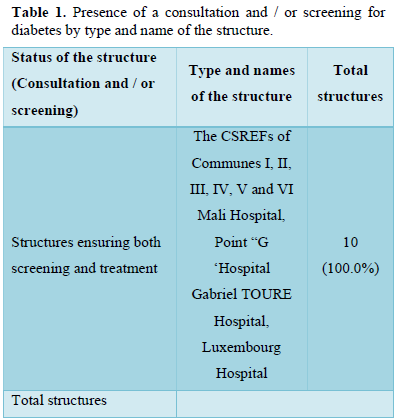
- Human Resources
All the care structures had an endocrinologist or internist. From the first referral, there was at least one endocrinologist in all CSRefs.
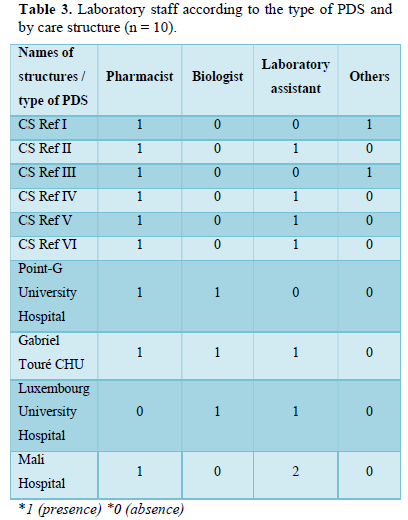
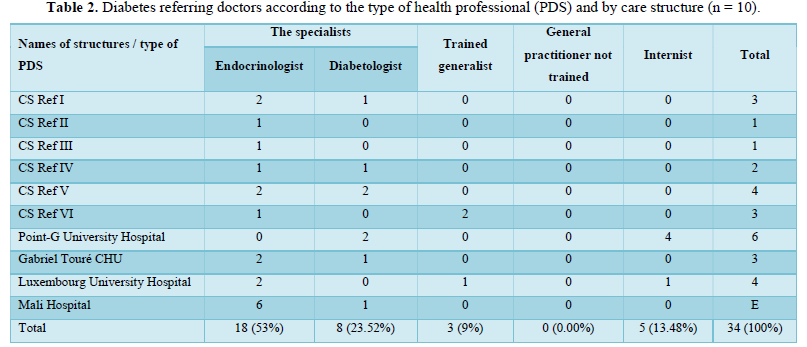
Nine out of ten structures providing care (69.23%) had a pharmacist.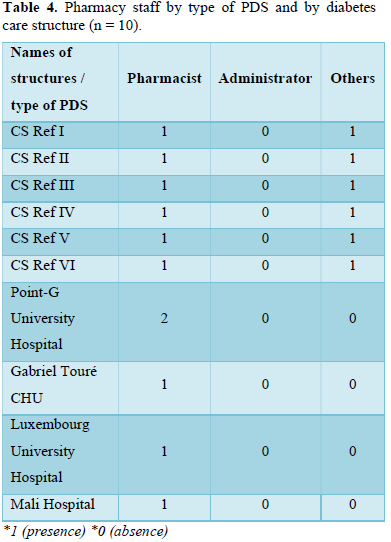
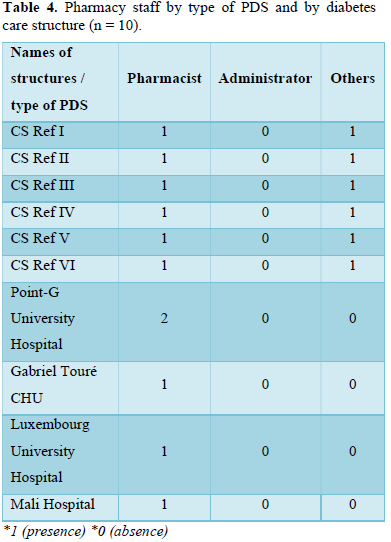
We have noticed that all the support structures have a sales depot. We noted the presence of a pharmacist in our 10 structures surveyed.
2.Technical Platform Linked to Diabetes by Structure
2.Technical Platform Linked to Diabetes by Structure
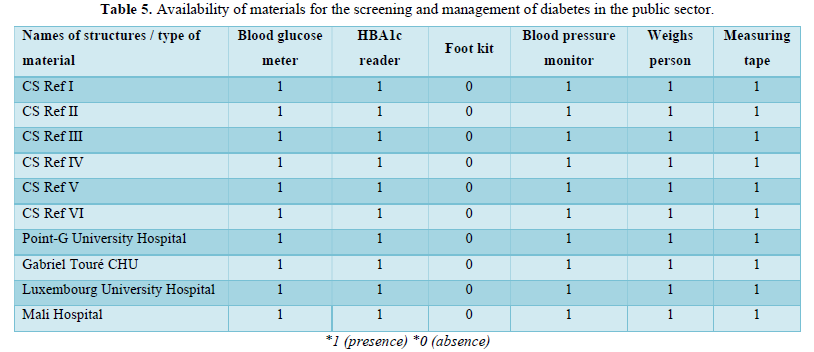
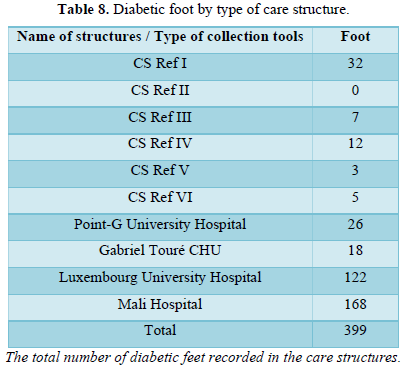
All public sector structures have blood pressure monitors, personal scales and tape measures and blood glucose meters. The HbA1c reader and the Foot Kit were not always available.
Foot kit (Dressing box, nail clipper, hand and foot cure, scissors, Sensor and adapter, cuffs and toe inflator etc.
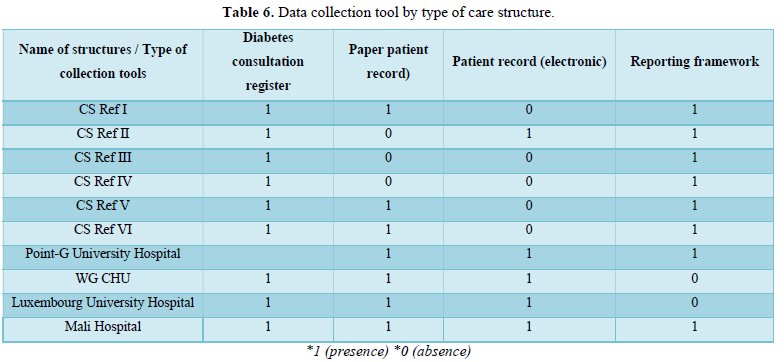
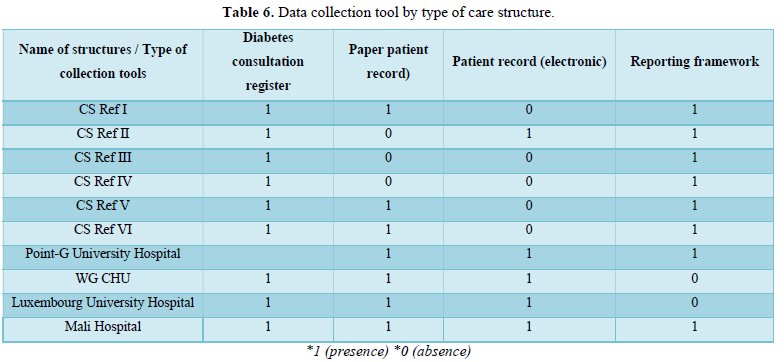
In the different structures, the main data collection tool used was the consultation register. Data was collected systematically via monthly or quarterly reports.
3. Support Data
3. Support Data
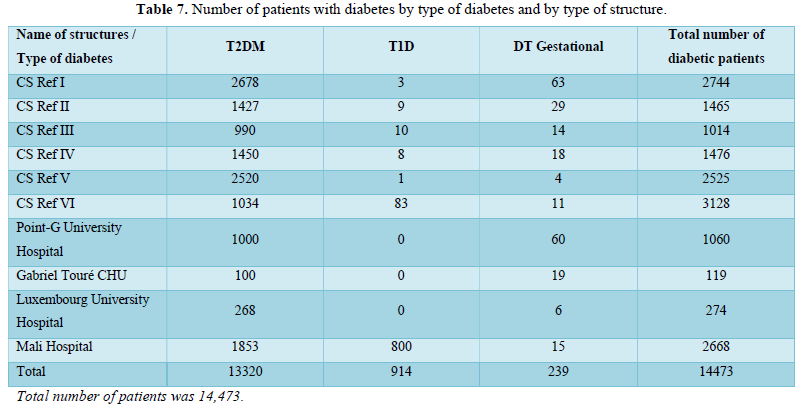
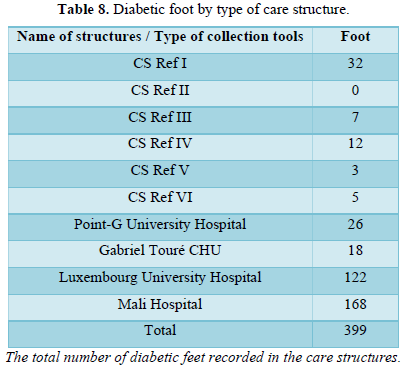
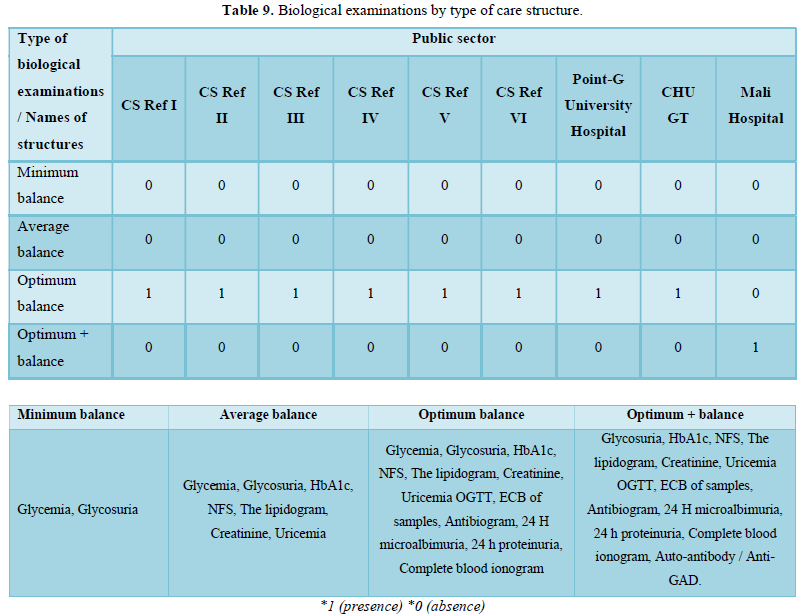
All diabetes care structures provided minimum check-ups. The CSRefs and the Hospitals ensured the optimum balance sheets except the hospital in Mali also provided the optimum balance sheet.
4.Medications
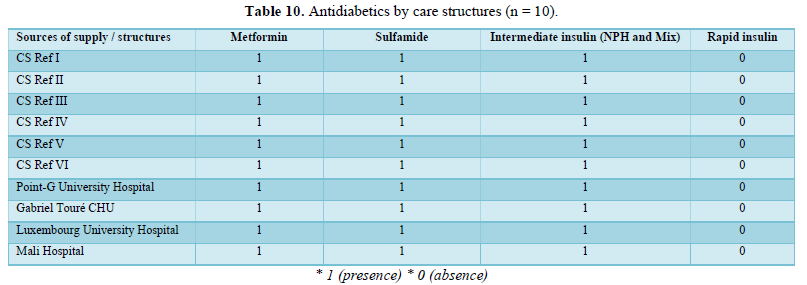
4.Medications
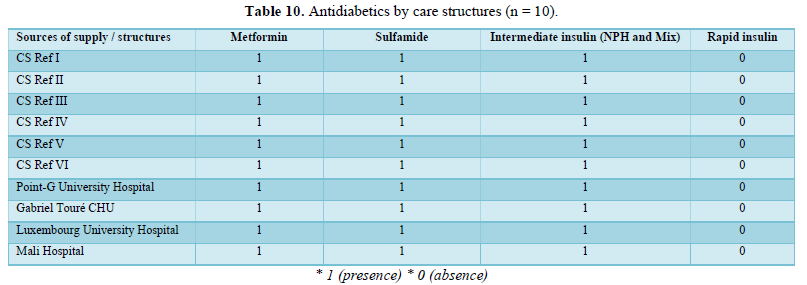
There was at least one oral antidiabetic drug (Metformin or Sulfamide) in the stores all the structures doing screening and PEC. In addition to at least one ADO, CSRefs and hospitals had at least the insulin intermediate. Rapid insulin was often out of stock in CSRefs and hospitals.
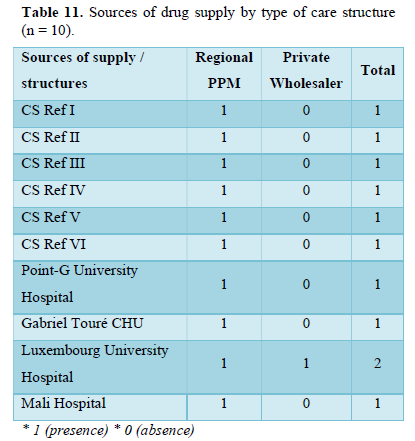
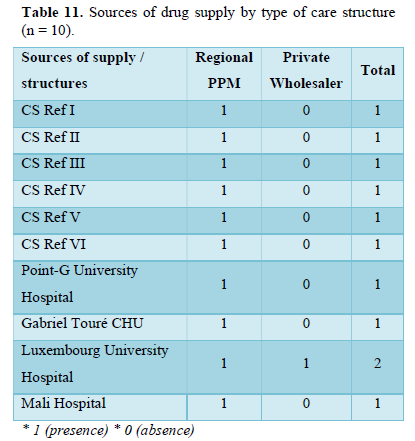
We have noticed that all our structures get their supplies from the regional PPM except the CSRef V and Luxembourg University Hospital have recognized that they often get their supplies from private wholesalers as well.
DISCUSSION
Our study was cross-sectional, focused on data from January to December 2019 from 10 health structures in Bamako. Diabetes screening was effective in all facilities. Diabetes screening and management were effective at all 10 facilities. We also noted that 6/10 were CSRefs (first referral structure) and 04 were hospitals.
The management of diabetes in the structures was ensured by at least an endocrinologist and / or a diabetologist in the 10 structures in total they had at least 18 specialists. This care provided by specialists is provided at CSRef and hospital level. The presence of specialists in these structures is explained by the creation of a diploma course (DES / DU) at the University of Bamako since 2010 and the recruitment of specialists by the public service of the state and communities in Bamako [9]. All public sector structures have equipment for screening for diabetes and these risk factors, namely a blood glucose meter, a blood pressure monitor, a bathroom scale and a tape measure. In addition to screening equipment, CSRefs and hospitals had at least one HbA1c reader and foot kit. The therapeutic education material (televisions and DVD players, BAI, posters) is no longer functional in a majority of structures. In the different structures, the main data collection tool used was the consultation register. Data was collected systematically via monthly or quarterly reports. There is a disparity in the centralization of data since to date several modes of data feedback in both the public and private sectors. This lack of centralization and data processing makes it difficult to advocate, but also to monitor consultations and the supply of anti-diabetic drugs.
The active file of diabetic patients was estimated at 15,000 patients. This figure highlights an almost daily increase in the number of diabetic patients followed in Bamako. A hospital prevalence of 5.1% was reported in a recent article published in Mali Medical [10]. Other old studies carried out by Malian medical specialists indicated that diabetes affects around 3% of the population, and that type 2 represents 90% of cases [11]. The adoption of the STEP wise strategy [12], which is a chronic disease surveillance approach through risk factors carried out in Mali in 2013, gave a prevalence of overweight 16.6% and that of obesity 8, 8% in Bamako [13]. Mali is going through a health transition, as increased globalization and accompanying urbanization have created a double burden of communicable and non-communicable diseases.
All diabetes care structures provided minimum check-ups. The CSRefs and the Hospitals ensured the optimum biological assessments. The hospital in Mali, in addition to the optimum assessment, carried out other more specialized tests, in particular the dosage of diabetes auto-antibodies. This hospital houses a sub-unit for the management of type 1 diabetes in Bamako, which is the result of a collaboration between the Ministry of Health and Sante Diabetes with the support of the Life for A Child program. It is reported that although few resources are available for health in Mali, a mobilization around diabetes has gradually taken shape, since 2003, other actors have become involved, in particular Santé Diabète, but also the Malian State, which created in 2002 a section specific to non-communicable diseases within the National Directorate of Health [14]. This MNTs section of the DNS has now become a division in the General Directorate of Health and Public Hygiene (DGSHP). Mali has included NCDs in its Health and Social Development Program II since the 2005 period and the IV currently being validated.
This study allowed us to have an inventory of the health offer in connection with the screening and management of diabetes in the health system in Bamako. The challenges are still enormous, such as the often-late management of diabetic patients, but also by other factors, such as the difficulty of patients to respect a balanced diet or the difficulty of access to treatment.
CONCLUSION
With this research, we tried to identify some key elements of the diabetes management process in Bamako. More specifically, we have highlighted the role played by referring physicians and the underlying logic of their interventions in the offer and structuring of care and the construction of knowledge in initial and continuing training. This study makes it possible to understand the process of screening and treatment of diabetes, to identify the capacities and the gaps existing between the different structures but also the multiple underlying constraints. These results focus on the planning of capacity building actions and the technical platform of health structures. The amplification of targeted actions based on some of the difficulties raised by the various referring physicians, could make it possible to optimize the management of diabetes in Mali. We recommend practical proposals to improve the diabetes response:
- align the response to the health transition with the strengthening of health systems by decentralizing the PEC for diabetes at the primary level (CSCOM).
- improve data on Diabetes;
- the implementation of a structured approach to strengthen the achievements and work on the overall prioritization of CVD in Mali.
- Human Development Report (2020) Fractured Societies Lead People and Planet to Collision, UNDP Says UNDP in Mali. Accessed on: November 11, 2021. Available online at: https://www.ml.undp.org/content/mali/fr/home/presscenter/pressreleases/2020/rapport-sur-le-developpement-humain-2020-selon-le-pnud.html
- Soumaoro B (2018) Mme OUANE Aïssatou TANGARA, Statistician. INSTAT: 57.
- Wesenbeeck CFA van (2018) Distinguish urban and rural food security in West Africa. Accessed on: March 2, 2020. Available online at: https://www.oecd-ilibrary.org/fr/development/distinguer-securite-alimentaire-urbaine-et-rurale-en-afrique-de-l-ouest_159010a5-fr
- ICCP-Portal (2013) Mali-National Policy for the Control of Noncommunicable Diseases. Accessed on: November 11, 2021. Available online at: https://www.iccp-portal.org/sites/default/files/plans/Mali-Politique%20nationale%20de%20lutte%20contre%20les%20maladies%20non%20transmissibles%202013.pdf
- Yaya SH, Kengne AP (2014) Management and control of hypertension in Africa: A barrier analysis. The challenge of preventing cardiovascular disease. 2014: 163.
- Traore A (2006) Problem of the care of diabetic patients in health centers in Mali. University of Bamako.
- Dembélé S (2021) Problem of the management of Graves' disease in sub-Saharan Africa (case of Mali). [PhD Thesis]. USTTB.
- Gobatto I, Traoré AT (2011) From one knowledge to another, the fight against diabetes in Mali. Otherwise, Mook Collection.
- Diabetes in Mali: A health emergency! (2016) Le Monde.fr. Accessed on: March 13, 2020. Available online at: https://www.lemonde.fr/afrique/article/2016/03/28/diabete-au-mali-une-urgence-sanitaire_4891061_3212.html
- Aa D, Ia N, Am G, Aht D (2019) Epidemiological and Clinical Study of Sugar Diabetes in A Reference Health Center of Sikasso. 2019: 6.
- Sidibé AT, Besançon S, Beran D (2007) Diabetes: A new public health issue for developing countries: The example of Mali. Med Metabol Dis 1(1): 93-98.
- WHO (2006) STEPS: The WHO STEPwise approach to chronic disease risk factor surveillance: WHO STEPS surveillance manual. Accessed on: March 9, 2020. Available online at: https://apps.who.int/iris/handle/10665/43483
- Bâ HO, Menta I, Camara Y, Sangaré I, Sidibé N, et al. (2014) Overweight and obesity in the population over 20 years old in Bamako urban areas (Mali). Pan Afr Med J 19: 352.
- Martini J, Fligg A (2020) The emergence of type 2 diabetes as a public health problem in Mali. Analysis of national health policies and training of health professionals.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Journal of Allergy Research (ISSN:2642-326X)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Advance Research on Alzheimers and Parkinsons Disease
- BioMed Research Journal (ISSN:2578-8892)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)


