Research Article
Prevalence of Respiratory Disease Based on High Resolution Computed Tomography Chest among High Altitude Residents
4671
Views & Citations3671
Likes & Shares
Background: High-resolution Computed Tomography (HRCT) closely reflects changes in lung structure and suited to evaluate the pulmonary parenchyma and airways and has superior sensitivity over conventional chest radiography in a wide range of lung diseases. Study reveals that 14.8% respiratory infection was prevalent causing disease burden in Jumla. This study aims to assess the prevalence and type of lung patterns detectable at high-resolution computed tomography (HRCT) chest in a primary care population and to diagnose the types of diseases.
Methods: This was an observational, retrospective, cross-sectional study conducted in Karnali Academy of Health Sciences, Jumla over the period of July 2019 to September 2020. Data was interpreted in frequency, percentage and standard deviation. HRCT Scan was carried out with CT machine using 120kV, 200mA with scan time per slice as 1-2 sec with slice thickness 1 mm, at full inspiration with patient in supine position. The HRCT patterns of 40 patients obtained at the primary visit for cough, shortness of breath, chest pain and fever were evaluated.
Results: A total of 40 patients were enrolled in this study with mean age ±SD (min-max) 52.6 ± 17.7 (24-85) among which 50% were females and 50% males. HRCT chest findings which were visualized in console were categorized, among which 50% patients had fibrosis in lung affecting mostly Upper lobe, 30% centrilobular nodules, 22.5% had hyperinflation and many more. The most common diagnosis according to the HRCT findings was normal (28 %), Post TB Fibrosis (22%) and Chronic Obstructive pulmonary disease (COPD, 20%). These findings helped in the diagnosis and management of the patients who were previously labelled as Chronic Obstructive Pulmonary Disease.
Conclusion: Imaging plays an integral role in the diagnosis and management of suspected pulmonary infections and may reveal useful signs on CT scan. The respiratory infection in a primary care population shows patterns of COPD reflected in HRCT as centrilobular nodules (32.5%), hyperinflation (22.5%), bullae etc. similarly complication of PTB as fibrosis was noted in 50%, followed by bronchiectasis (17.5%) were commonly prevalent in our part.
Keywords: Chronic obstructive pulmonary disease, High-resolution computed tomography, Respiratory diseases
BACKGROUND
High-resolution Computed Tomography (HRCT) of the lungs allows superior imaging of fine structures of the lung and its airways and has superior sensitivity over conventional chest radiography in a wide range of lung diseases [1,2]. HRCT is well established for diagnosing and managing many pulmonary diseases and characterizing diseases that affect the pulmonary parenchyma and small airways [3]. Respiratory diseases constitute the most common non-communicable disease in Nepal with chronic obstructive pulmonary disease forming a major portion. 80% of facilities in Karnali Province offer support services for chronic respiratory disease including diagnosis, prescription of treatment and management [4]. Paudel [5] study reveals that 14.8% respiratory infection as the common disease burden. The purpose of this study was to assess the HRCT Chest; of patients seeking help for cough, fever, shortness of breath and to assess the prevalence of respiratory diseases and patterns of diseases in lung. This will also help in the planning and implementation of future regional government health policies.
METHODS
This was an observational, retrospective, cross-sectional study conducted in KAHS as it is a referral centre for the upper Karnali region and CT scan is only available in this centre. Jumla being a mountainous district situated in Karnali Province and it accommodates only 2% population of Nepal. The upper region of Karnali referral centre is Karnali Academy of Health Sciences (KAHS) which has been providing services by specialist doctor since 2072 [6]. All the patients above 15 years of age, who were admitted to medicine department with history of cough, chest pain, fever or shortness of breath and agreed to undergo HRCT chest from July 2019 to September 2020 were included in this study. Informed consent was taken from the patient or patient party after explaining about the study. The study protocol was approved by the Institutional Review Committee of KAHS. HRCT Scan was carried out with Philips 16 slice, helical scan, 3rd generation CT machine using 120kV, 200mA with scan time per slice as 1-2 sec with slice thickness 1 mm, at full inspiration with patient in supine position. HRCT images of subjects were visualized by me and my corresponding authors for any abnormalities and findings were recorded as presence or absence of the features according to the localization and number of affected lobes and segments involved. This study aimed to report solely the results of the radiological examinations. Data were filled in the Microsoft Excel 2010 and was presented in frequency, percentage and standard deviation.
RESULTS
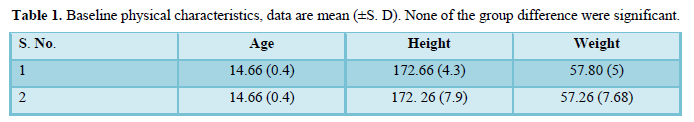
A total of 40 patients were enrolled in this study with mean age ±SD (min-max) 52.6 ± 17.7 (24-85) among which 50% were females and 50% males (Table 1).
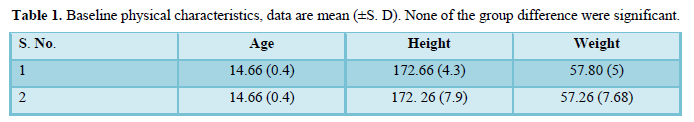
HRCT chest findings which were seen and categorized among which 50% patients had fibrosis in lung affecting mostly Upper lobe, 32.5% centrilobular nodules, 22.5% had hyperinflation and many more as shown below. Most of the patterns had multilobar findings in HRCT chest (Table 2).
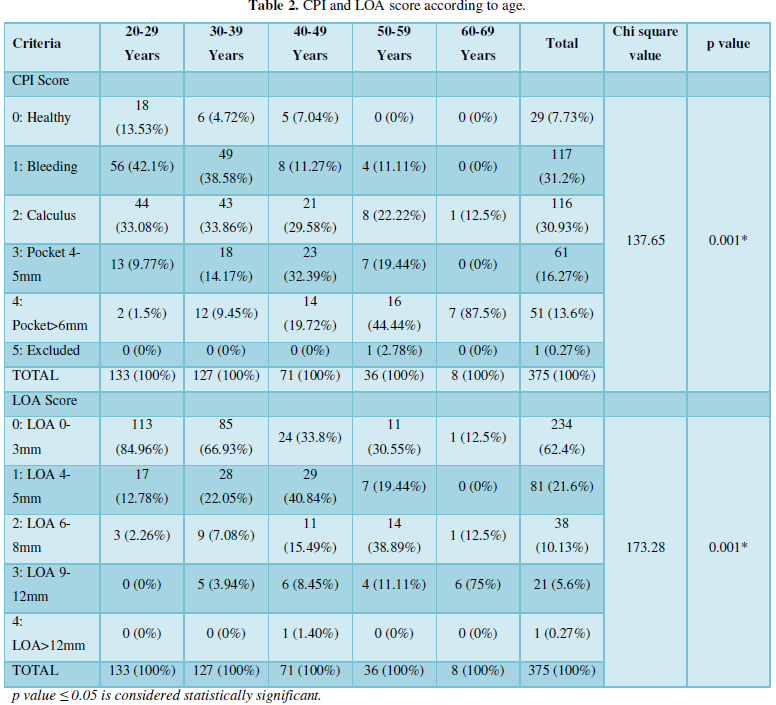
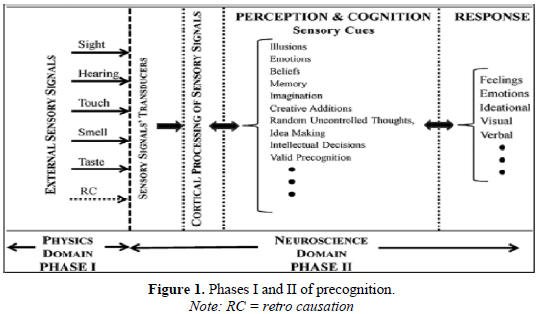
Most common diagnosis according to the HRCT findings was as shown, among which 28 % had normal finding, 22% post-TB fibrosis (post-Tuberculosis), 20% COPD (Chronic Obstructive Pulmonary Disease) and many more (Figure 1).
These findings helped in the diagnosis and management of the patients who were previously labelled as COPD.
DISCUSSION
Lung infections is the most common cause of high morbidity and mortality, especially in the elderly and immunocompromised patients, similarly in our part it accounts for 34% [6,7]. Basnyat [8] states that respiratory problems are high in high altitude commonly due to hypoxic conditions, crowding in huts, smoky wood stoves, and cold, dry air. HRCT allows superior imaging of fine structures of the lung and its airways and are helpful in the diagnosis and detection of chronic diffuse lung disease [1]. Out of 40 patients, HRCT pattern was looked in all types of respiratory disease whether CXR showed upper, middle or lower zone involvement. Whereas Lahde [2] looked for the HRCT pattern in patients of lower respiratory tract only [2]. In our study, 27.5% had normal HRCT, 50% had fibrosis in different lobes of the lungs mostly involving bilateral lobes 12 (60%) and segments, GGO (7.5%), septal thickening (25%), consolidations (15%) with similar Lahde et al (2002) study showed ground-glass opacity (58%), discrete consolidations (52%) and peribronchovascular thickening (37%). In our study 20% had COPD changes in HRCT described as hyperinflation, centrilobar nodules, air trapping. Nemec [9] study specifies that among patients with pulmonary tuberculosis (PTB), HRCT shows centrilobar small nodules and branching linear/ nodular opacities (tree-in bud sign), also could show patchy or lobular areas of consolidation, interlobular thickening and cavitation of nodules that may later heal resulting in fibrotic lesion [9]. In 5% of our active PTB patients HRCT had tree in bud appearance, consolidation (1), cavitation (1) and healed fibrosis was present in both patients. Complications of PTB as empyema (5%) and pulmonary fibrosis (22.5%) were seen in HRCT. Thus, CT helps in showing such complications better [9]. Whereas, in Lahde et al (2002) study, confluent consolidations were seen in 16% (1 case with an air bronchogram) and tree-in-bud pattern in 26% [2]. Walker [10] states that tree-in bud sign as an imaging manifestation of various infections caused by bacteria, fungi, parasites or viruses due to impaction of pus, mucus or fluid resembling a budding tree with branching nodular V or Y shaped opacity [10]. Thus, during these days; HRCT of the lungs had developed into a mature technique for the evaluation of diffuse pulmonary parenchymal abnormality and plays a key role in pulmonary infections diagnosis given that standard radiography is lacking in specificity [11].
LIMITATIONS
Due to the small size, it may not represent all the population of Jumla. Due to cost effect of HRCT not all patients could be involved in our study. It was not funded study.
CONCLUSION
Imaging plays an integral role in the diagnosis and management of suspected pulmonary infections and may reveal useful signs on CT scan. The respiratory infection in a primary care population shows patterns of COPD reflected in HRCT as centrilobular nodules (32.5%), hyperinflation (22.5%), bullae etc. similarly complication of PTB as fibrosis was noted in 50%, followed by bronchiectasis (17.5%), were commonly prevalent in our part.
- Swensen JS, Aughenbaugh LG, Douglas WW, Myers LJ (1992) High resolution CT of the lungs: Findings in Various Pulmonary Diseases. Amer J Roe 158: 971-979.
- ACR–STR practice parameter for the performance of high-resolution computed tomography of the lungs in adults. Development Chronology for this Practice Parameter. Revised 2020 (Resolution 33). Available online at: https://www.acr.org/-/media/ACR/Files/Practice-Parameters/HRCT-Lungs.pdf
- Lähde S, Jartti A, Broas M, Koivisto M, Syrjala H (2002) HRCT findings in the lungs of primary care patients with lower respiratory tract infection. Acta Radiologica 43: 159-163.
- Karnali Province: Key Findings from the 2015 Nepal Health Facility Survey and 2016 Nepal Demographic and Health Survey. Kathmandu, Nepal: Ministry of Social Development, Karnali Province, Nepal. Available online at: https://dhsprogram.com/pubs/pdf/SR255/SR255.pdf
- Paudel T, Amgain K, Sanjel S (2018) Health Scenario of Karnali Province. J Kar Aca Heal Sci 1(3): 35-40.
- Pal A, Paudel S (2018) Pattern of Illnesses among the Tribal Communities of Jumla, Nepal: Hospital Based Study. J Kar Aca Heal Sci 1(1): 4-7.
- Herold CJ, Sailer JG (2004) Community-acquired and nosocomial pneumonia. Eur Radiol 14(Suppl. 3): E2-E20.
- Basnyat B, Cumbo AT, Edelman R (2001) Infections at High Altitude. Clin Infect Dis 33: 1887-1891.
- Nemec FS, Bankier AA, Eisenberg LR (2013) Upper Lobe-Predominant Diseases of the Lung. AJR Am J Roentgenol 200: W222-W237.
- Walker MC, Abbott FG, Greene ER, Shepard O, Vummidi D, et al. (2014) Imaging Pulmonary Infection: Classic Signs and Patterns. AJR Am J Roentgenol 202: 479-492.
- Aubrya B C, Godetb C, Caumes E (2012) Lung infections: The radiologist’s perspective. Diagn Interv Imaging 93: 431-440.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)



