3523
Views & Citations2523
Likes & Shares
Understanding the science of safety and the core principles of high reliability are first steps in creating a true culture of safety wherein human factor can contribute in the improvement in healthcare delivery. In the world of healthcare, very little training in human factors is provided to staff, unlike the other safety-critical industries. Human factors research examines the environmental, organizational and job factor of human interacting with the system as well as physiological and psychological characteristics that influence behavior at work. Principle of safety science is a commitment to zero harm. Understanding and implementing the best practices can build high reliability organizations a roadmap to achieve exemplary clinical outcome. Topics highlighting several key safety principles including just culture, professional bodies in healthcare organization, a range of human factors such as managerial, team and individual characteristics that influence the behavior of healthcare staff in relation to safe patient care and framework to demonstrate the role of human factors in patient safety and are known to reduce patient harm and improve the safety and quality of patient care. Best practices performed consistently over time have demonstrated superlative outcomes. Developing a model like system approach which demonstrated consistent application of leader rounding; hourly purposeful rounding and bedside shift report can influence how patient safety can be possibly achieved. A commitment to zero harm and application of best clinical and safety practices are critical steps in developing a culture of safety in healthcare organizations contributed significantly in reduction of patient harm a compelling reason for nurses in all healthcare settings to embrace safety science and the principles of high reliability.
Keywords: Human factor, Patient safety, Culture in patient safety, Human engineering, System ergonomics, Human performance
INTRODUCTION
In the world of healthcare, very little training in human factors is provided to staff, unlike the other safety-critical industries. In the United States over 440,000 individuals die each year as a result of preventable hospital errors [1]. Yet healthcare continues to lag behind other highly complex organizations such as the aviation and nuclear industries in overall safety practices. Understanding the science of safety and the core principles of high reliability are first steps in creating a true culture of safety wherein human factor can contribute in the improvement in healthcare delivery as well as the achievement of excellent patient care delivery outcome. Patient safety is a global challenge that requires knowledge and skills in multiple areas, including human factors and systems engineering [2]. Some care settings or care situations are particularly prone to hazards, errors and system failures. For instance, in intensive care units (ICUs), patients are vulnerable, their care is complex and involves multiple disciplines and varied sources of information and numerous activities are performed in patient care; all of these factors contribute to increasing the likelihood and impact of medical errors. Health care organizations must create and foster an environment in which safety will become a top priority.
Approach to Human Factors and Ergonomics
As cited in WHO report (2009) [3] human factors usually linked closely to Ergonomics which is the application of scientific information concerning humans to the design of objects, systems and environment for human use. In a work context, human factors research examines the environmental organizational and job factor of human interacting with the system as well as physiological and psychological characteristics that influence behavior at work. Principle of safety science is a commitment to zero harm. Understanding and implementing best practices that can build high reliability organizations and importantly sustaining those practices, is a roadmap to achieving exemplary clinical outcomes. There are several key safety principles including just culture, professional bodies in healthcare organization, a range of human factors such as managerial, team and individual characteristics that influence the behavior of healthcare staff in relation to safe patient care and framework to demonstrate the role of human factors in patient safety and are known to reduce patient harm and improve the safety and quality of patient care.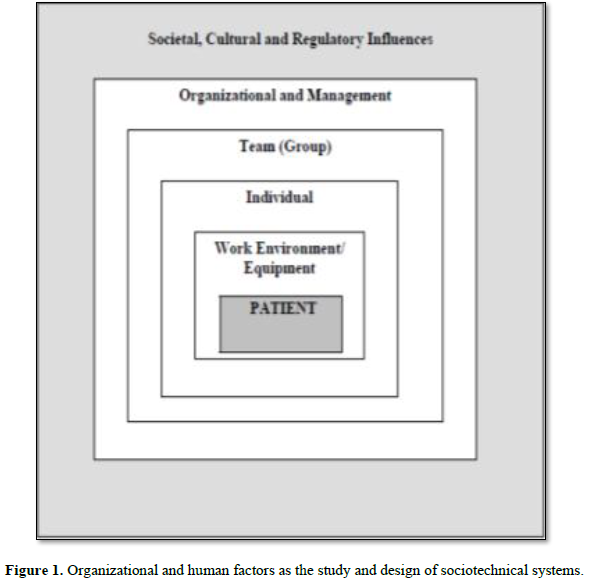
Implementation Approach
A high reliability framework provides the structure needed for organizations to achieve desired safety and quality goals. Best practices performed consistently over time have demonstrated superlative outcomes. A hospital can develop a model which demonstrates that consistent application of leader rounding; hourly purposeful rounding and bedside shift report can influence how patient safety can be possibly achieved as well as a model to demonstrate the role of human factor in patient safety. Human factors consider three domains of system design: physical, cognitive and organizational [4]. The physical domain focuses on how the human body and physical activity interacts with work design, for example, the layout of computer desks. The cognitive domain focuses on how mental processes interact with other elements of systems. This includes memory, information processing and decision making. The organizational domain focuses on how individuals and teams interact with tools and technologies. According to scientists [5], human factors approaches can be used to design systems that support health care providers to deliver safe patient care at the same time as reducing work injuries and improving the quality of people’s working life. Taking a human factors approach means that when safety incidents occur, it is important to have a non-punitive culture [4]. Instead of blaming individuals for events, the systems approach focuses on building systems to reduce potential risks and prevent future error, building system defenses to reduce the likelihood of errors resulting in patient harm.
A systems approach is essential and it is human systems which are the critical factor in leading to unsustainability, and potentially can be changed to enable transition towards sustainability [6]. Sociotechnical systems are systems with a human element and there is particular knowledge accumulated about them that is useful in design [3, 7] which produced a model of the organizational, human and technical components of sociotechnical system (Figure 1).
CONCLUSION
Nurses are at the sharp end of care. A commitment to zero harm and application of best clinical and safety practices are critical steps in developing a culture of safety in healthcare organizations [8-10]. A suggestion for the wider adoption of human factors in patient safety practices was concluded by World Health Organization [3]. The significant reduction in patient harm that results is a compelling reason for nurses in all healthcare settings to embrace safety science and the principles of high reliability. The overall human factors philosophy is that the system should be designed to support the work of people, rather than designing systems to which people must adapt [11-13].
1. James JT (2013) A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf 9: 122-128.
2. Carayon P, Wood KE (2010) Patient safety, the role of human factors and system engineering. Stud Health Technol Inform 153: 23-46.
3. World Health Organization (2009) Human factors in patient safety review of topics and tools.
4. World Health Organization (2016) Human factor: Technical series on safer primary care.
5. Marras WS, Hancock PA (2014) Putting mind and body back together: A human system approach to the integration of physical and cognitive dimension of task design and operation. Appl Ergon 45: 55-60.
6. Hopkins TS, Bailly D, Elmgren R, Glegg G, Sandberg A, et al. (2012) A systems approach framework for the transition to sustainable development: Potential value based on coastal experiments. Ecol Soc 17: 39.
7. Moray N (2005) Ergonomics: The history and scope of human factors (Volume 1).
8. Brown SC, Legg (2010) Achieving transition to sustainability: Lessons from human factors and ergonomics.
9. Dul J, Bruder R, Buckle P, Carayon P, Falzon P, et al. (2012) A strategy for human factors/ergonomics: Developing the discipline and profession. Ergonomics 55: 377-395.
10. Lawler EK, Hedge A, Pavlovic VS (2011) Cognitive ergonomics, socio technical system and the impact of healthcare information technologies. Int J Ind Ergon 41: 336-344.
11. Shekelle PG, Wachter R, Pronovost P, et al. (2013) Making health care safer II: An updated critical analysis of the evidence for patient safety practices. Comparative Effectiveness Review No. 211 prepared by the Southern California-RAND Evidence-based Practice Center under Contract No 290-2007-10062-I. Rockville, Maryland: Agency for Healthcare Research and Quality.
12. The Joint Commission: Human Factor Analysis in Patient Safety System (2015) The Source 13.
13. Weaver SJ, Dy SM, Rosend MA (2014) Team-training in health care: A narrative synthesis of the literature. BMJ Qual Saf 23.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- Advance Research on Alzheimers and Parkinsons Disease
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)



