Review Article
Lessons Learned from Infectious Diseases’ History
5346
Views & Citations4346
Likes & Shares
Global reports of infectious diseases - such as the measles, tuberculosis, HIV, syphilis, cholera, a persistently high incidence of malaria as well as other transmissible diseases - denote a periodical occurrence, often associated with an increase in the numbers of affected people. In addition, new infectious diseases, caused by unknown pathogens or by organisms known yet not considered pathogenic to humans, are emerging.
With the propagation of Covid-19, caused by the ‘new’ coronavirus SARS-CoV-2, the biomedical research efforts have been redirected toward an early diagnosis and rational therapy of respiratory viruses. These latter have been associated with conventional means (limitation of direct contacts, face masks protection, hand hygiene, testing and tracking of cases, quarantine of infected people and their contacts) to prevent further spreading. As a result, ensuring the rapid development of safe and effective vaccines, using the latest biomedical technology (e.g., the sequencing of the SARS-CoV-2 genome), is essential to stop further contaminations.
Keywords: Infectious diseases, Epidemy, Pandemic, Eradication, Anthropo-zoonoses, Focus of infection, Spread infections, Population growth, Migration, Intercontinental transport
INTRODUCTION
Vaccination programs, increasing the level of hygiene in housing estates and the working environment, ensuring the health safety of drinking water and food in industrialized countries, have dramatically reduced perinatal, infant and child mortality from infectious diseases and has significantly extended life expectancy for both women and men. In the early 1960s, 181 years after the discovery of vaccination by Edward Jenner, Professor Karel Raška, Head of the Division of Communicable Diseases at the World Health Organization (WHO) in Geneva, greatly contributed to the eradication of the smallpox (Variola vera) - caused by the poxvirus (Poxviridae) - and of one of the most serious infectious diseases.
The worldwide successful eradication of the smallpox triggered a wave of optimism is regards to the possibility to deal with other dangerous infections to a similar extent in the foreseeable future. This hope was reflected in 1967 by US Chief Hygienist WH Stewart’s statement: “We can close the book on infectious diseases”. Unfortunately, two years later, limits to this statement had already been reached [1].
A decade later, on December 14, 1977, the WHO announced, through the voice of its then director H. Mahler “We have signed the death certificate of smallpox in Asia and the last case of smallpox in the world. There has been a real way to abolish smallpox via vaccination since 1980, which means saving $2 billion a year” [2]. Following the global scale smallpox vaccination program, last reservoirs of smallpox in Latin America disappeared in 1971, in Afghanistan and Pakistan in 1974, in India and Nepal in 1975. In October of the same year, the last case of smallpox in Bangladesh was three-year-old Rahima Banu. The last sick person in Africa was Ali MaowMaalin in 1977 [3,4]. The global eradication of the disease was solemnly declared in 1980 during the 33rd World Health Assembly solemnly.
In the biomedical research field, the epidemiological problem of infections and their immunological aspects importance has receded into the background [5], especially in industrialized countries, with a number of clinics and specialized departments focusing on the treatment of infectious diseases being shut down. Warning reports of new infections, especially in developing countries, have not been taken seriously enough [6,7].
Czechoslovakia became, in 1961, the first country in the world being poliomyelitis-free. In effect, following the eradication of the smallpox, poliomyelitis (polio) was the next focus of eradication. Even though it had been eliminated on some continent, there was still a need for global vaccination against it. The contribution of Czech experts and researchers, especially the one of virologist Dimitrij Slonim (1925-2017), in the search for a vaccine against polio, led to making Czechoslovakia one of the five countries in the world in 1957 to produce an effective vaccine against this disease, and two years later, Czechoslovakia became the first in the world to vaccinate children.
Vaccination against other infectious diseases has also been effective in reducing the number of patients to a minimum in a number of countries. An example would be the one of the measles, that was declared by the World Health Organization (WHO) to be under control i.e., per 1 million inhabitants, one or even fewer diseases would occur in the span of a year.
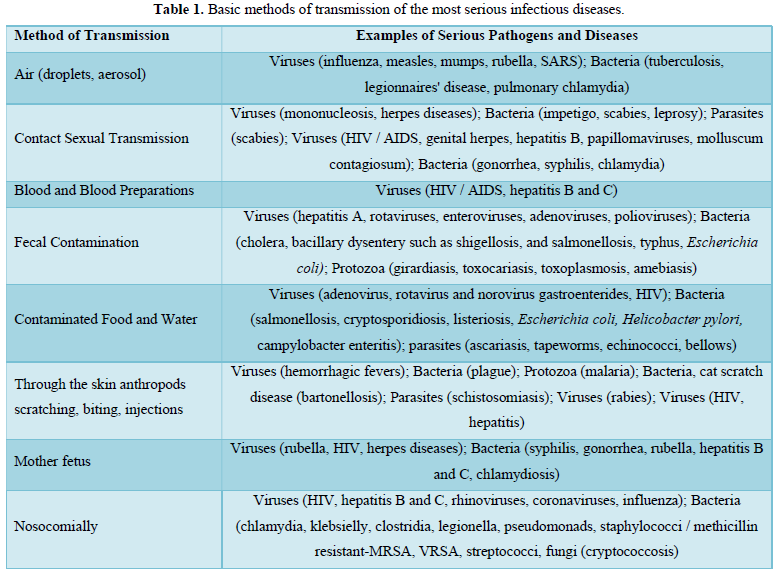
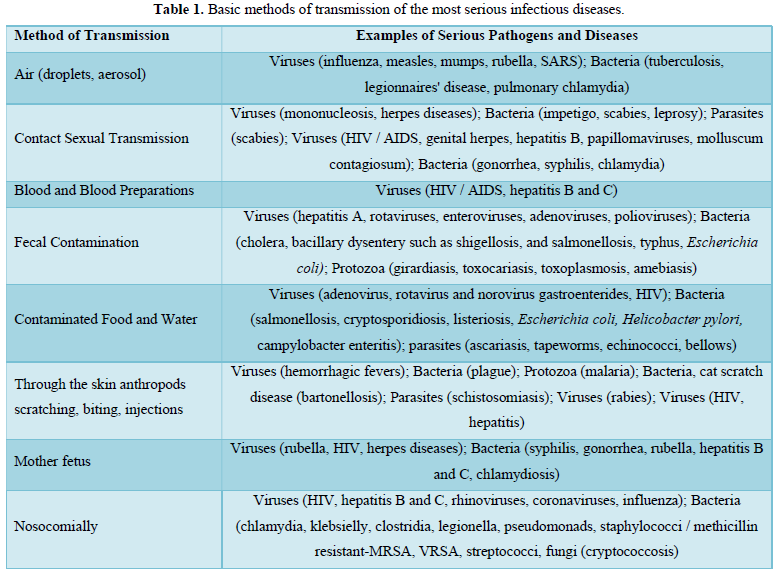
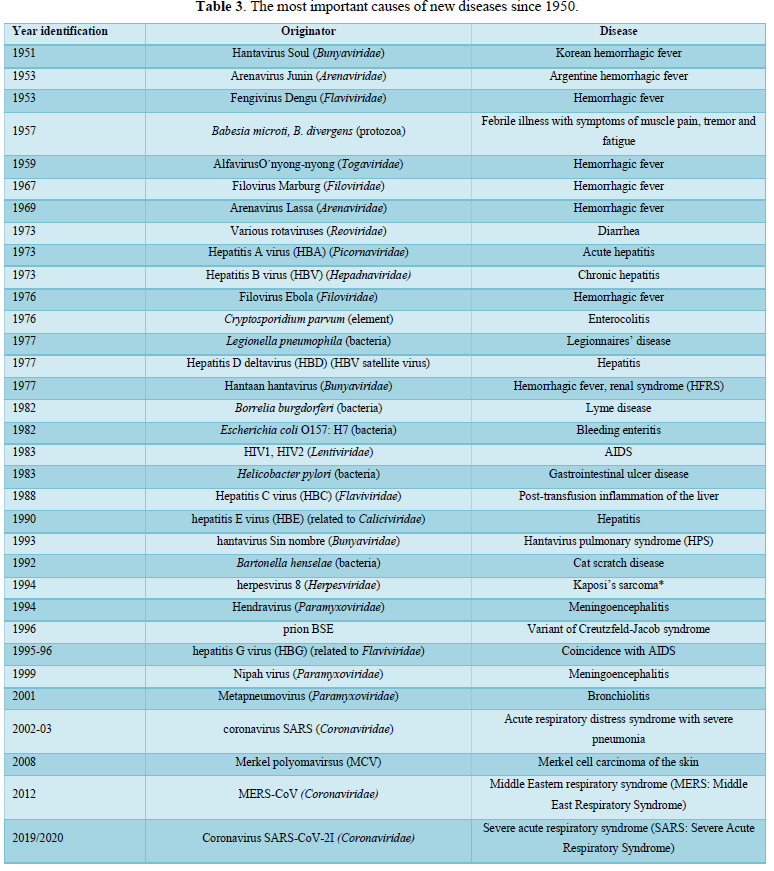
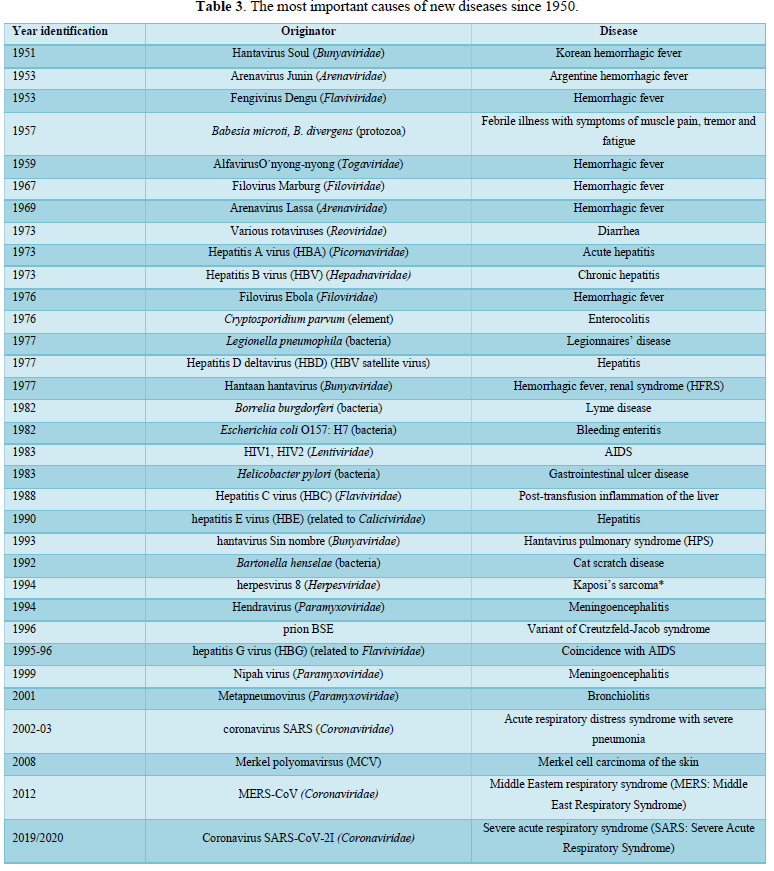
Infectious diseases are usually classified according to either taxonomic aspect, the pathogen causing them, or the organs they attack, however for practice, the classification according to their method of transmission is more illustrative (Table 1). Still, each classification has its specific informational value in terms of epidemiology.
PRE-EPIDEMIC PHASE OF ANTHROPOGENESIS
The number of people living in a certain area was really low, reducing contact between members of a population. It was therefore estimated that gathering and hunting would happen over an area of 1 to 10 km2. With such a low population density, pathogens causing acute diseases had little chances of spreading, or the infections were contained within the same groups, making the probability of infectious diseases spreading very low. This period, right before the onset of the Neolithic area i.e., the beginning of the agrarian revolution, was thus referred to as the pre-epidemic phase of anthropogenesis [6]. Everything changed with the development of agriculture, which, however, could only develop under very specific conditions (fertile soil, enough water for irrigation…), and in relatively limited regions with a mild climate and no significant weather fluctuations.
More people were also needed to carry out agricultural work. Only horticulture (i.e., primitive tillage, often without irrigation) could feed 1-3 people per 1 km2, more advanced agriculture [10-20] people and in combination with animal husbandry up to 165 people in the same area [7]. Increasing population, the emergence of settlements with a low hygienic standard within a large population, and the domestication of wild animals were the cause of an unprecedented onset and increase in the number of new infectious diseases, which then began to accompany humans more and more often. All this happened in a relatively short period of human development. This is aptly summed up by the American historian and writer S. Budiansky in his book “The Treaty of the Wilderness: Why Animals Chose Domestication”: “For two million years we have been hunters; then in tens of thousands of years we have become farmers”. The epidemic phase in human history began [8-12].
PATHOGENS IN COEVOLUTION WITH HUMAN
As is the case with other species of living organisms, many viral, bacterial, fungal and parasitic pathogens are inherent to humans and live in close coevolution with them. It is typical for these to cause only clinically milder diseases with relatively low mortality. They usually also live in their hosts throughout their lives and are passed vertically from parents to future generations. Examples are herpes viruses (Eppstein-Barr virus, γ-herpesvirus), polyomaviruses (JC virus, John Cunningham virus), papovaviruses, papillomaviruses (HPV), retroviruses and oncogenic viruses but there are many others.
PATHOGENIC AGENTS TRANSMITTED BETWEEN ANIMALS, FROM ANIMALS TO HUMANS AND FROM HUMANS TO ANIMALS
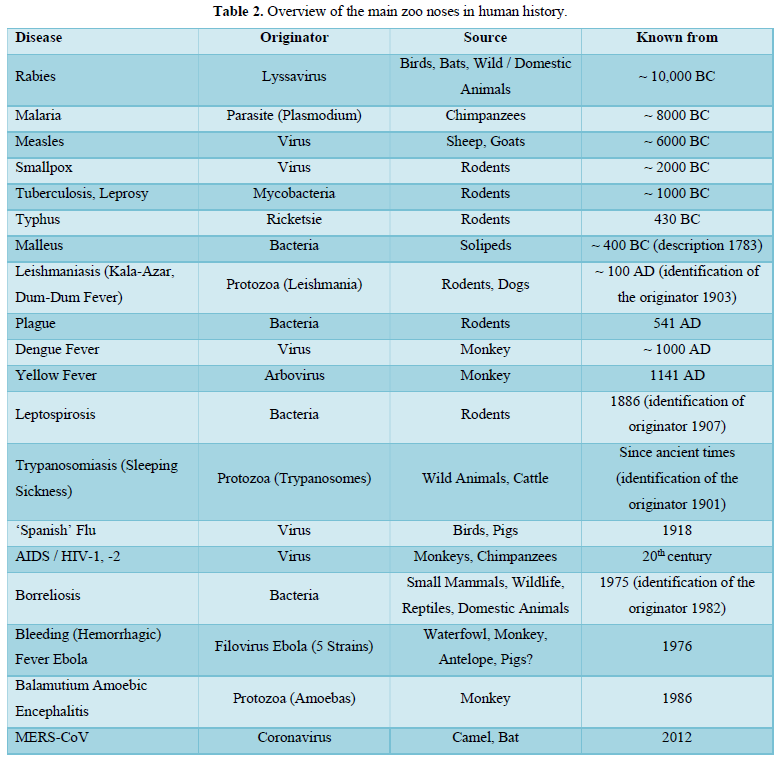
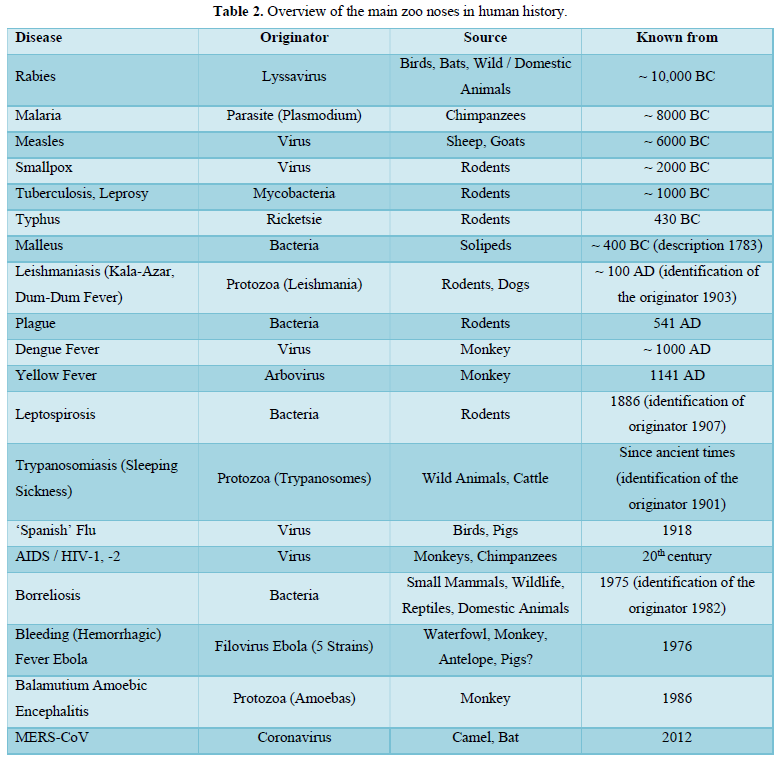
The origin of other pathogenic agents causing human infections, known as anthropozoonoses, can be traced back to animal sources. We know more than 500 agents (viruses, prions, bacteria, yeasts, fungi, protozoa and multicellular parasites) transmitting diseases from animals to humans and vice versa (Table 2) [13]. They have accompanied mankind since the beginning of time, and their detailed presentation would be beyond the scope of this Communication.
Leptospirosis is considered to be the world's most common zoonosis [14]. The zoonoses also lies epizoonoses, skin parasitic diseases which are caused by the imbalance of integument mostly insect parasites living on the surface and so may lead to penetration of infectious agents into the body (viruses, rickettsia, bacteria). In a broader sense, episoonoses also cover the spectrum of skin disorders, e.g., after insect bites.
Infections of wild animals did not initially attract attention until they began to cause large-scale epidemics among livestock and spread to humans. In 1889, a large plague starting from Asia broke out among African even-toed ungulates. It was caused by a paramyxovirus, thought to have developed the measles virus 5,000 years ago. This panzoonosis spread to a distance of 5,000 km in less than 10 years and in 1897 reached the Cape of Good Hope. It reduced herd numbers by 90% in Kenya alone. It also caused the local extinction of the tsetse fly and indirectly affected the conditions of other species, especially predators. After more than a hundred years, it still threatens herds of even-toed ungulates in East Africa. This was also the case with brucellosis introduced to the American continent, which permanent reservoir was even-toed ungulates in Yellowstone National Park [15]. Another example of the emergence and spread of a new infectious disease was the reforestation and introduction of ungulates and bisons in the northeastern United States in the 1920s and 1930s as part of so-called rescue programs. There had been an increase in tick-borne infections, febrile protozoa (babesiosis) and, in addition, a widespread epidemic of the hitherto unknown infectious disease first described for almost half a century (1975), Lyme borreliosis, caused by Borrelia burgdorferi. in 1981 [16]. To illustrate this point, one can also mention the introduction of flavivirus-induced zoonosis (identified as early as 1937), which in 1999 in New York, caused an outbreak of West Nile fever affecting 62 people. At the same time, the virus was isolated from dead birds. Previously, the disease occurred only in Africa, the Middle East and Western Asia, and sporadically in Central and Southern Europe. Further monitoring had shown that the virus was spreading via mosquitos’ bites and had already become endemic in the bird populations of East America and South Canada.
To this day, it is not known how the virus penetrated the American continent i.e., who was the vector, whether an infected person, migrating birds, or an airborne mosquito. Some of the blame for its spread was attributed to long-distance truck transport (infected eggs and mosquito larvae), or mosquitoes hatching in water in discarded tires or transported to the USA for recycling from Asia and Africa.
CAUSES OF EPIDEMIA AND PANDEMIA OF INFECTIOUS DISEASES
From ancient times to almost the 18th century, epidemics were viewed as punishments from demons or gods for the guilt and transgression of men. The unfavorable position of the stars or the ‘miasmas’ were also accused.
The theory of miasma was emitted by Galen (129-199 AD), one of the most famous physicians of the Roman period [17]. According to this idea, diseases were caused and transmitted by the presence of toxic vapor (miasma) in the air, which contained particles of decaying matter and had a characteristic odor [18].
This idea was later challenged by the ‘disease theory’ proposed by Girolamo Fracastoro in 1546, which considered germs to be chemical rather than living organisms, and revealed three different modes of disease transmission: direct contact with a sick person, indirect contact through objects and clothing belonging to the sick and remote transmission by air [19,20]).
At the beginning of the 19th century, both the theory of ‘miasma’ and the principle of ‘contagion’ began to be replaced by the ‘germ theory’ postulated by Louis Pasteur and supported by the evidence presented by Robert Koch [9,10]. However, under pressure from shipowners in 1818, the British Parliament voted that the plague was not contagious, and when a local epidemic of yellow fever broke out in Barcelona in 1821, French doctors explained its cause by miasma theory. In 1828 the French House ruled that yellow fever was not a contagious disease, and in that context, Nicolas Chervin was awarded the Grand Prize for Medicine by the Academy.
When a cholera epidemic broke out in Europe a year later (1829), believers of the germ theory of contagious disease were considered to be completely ignorant. This was another half a century before Robert Koch definitively confirmed, in 1876, Louis Pasteur’s germline theory of infectivity [21]. Epidemics have always triggered feelings of guilt and repentance (flagellation). Even the English historian E. Gibbon (1737-1794) interpreted the causes of the disintegration and demise of the Western Roman Empire as a punishment for softened and immoral life [16-18]. Almost at the same time, the English economist TR Malthus (1766-1834) published his population theory [19], which had a significant impact on demography, sociology and economics. He was the first to explain the causes of epidemics sociologically: uncontrollable population growth, associated with scarce food and other resources, resulted in poverty, hunger, social storms, and ultimately the outbreak of an epidemic as a natural brake on overpopulation.
Misinterpretations of the causes of epidemic outbreaks have arisen, on one hand, from the limited knowledge we had at the time, but also from clinging to earlier, seemingly proven evidences and facts. As an example, in the recent past, gastroduodenal ulcers were thought to be the result of so-called civilization stress, but their presumed etiological agent is Helicobacter pylori (discovered in 1982) [21].
NEW FOCUSES ON DISEASES AND THE WAYS OF THEIR SPREAD
As in the past, outbreaks of disease are still emerging in overcrowded urban agglomerations. Mass migration from rural regions brings specific infections to cities where newcomers live in primitive unhygienic conditions, without sanitation, electricity or affordable healthcare. The nutritional habits, social and sexual behaviors of the population are changing.
As far as the transmission of diseases directly between people is concerned, tourism and intercontinental air transport of people constitute a serious threat. The populations travel more and more often, especially between climatically diverse localities with a different history of infections. Migration represents the greatest cause of infections spreading. Populations from different ethnicities and religions, political and war conflicts all contributed to an increased traffic between different parts of the world. There is no shortage of examples from the past. Already at the time of the migration of nations, infections such as the plague, the typhoid fever, the smallpox and measles, were spreading, decimating America's original population within decades of their discovery. However, it is not just about human migration. The transport of livestock’s, through which pathogens enter new areas, plays an important role in the emergence and spread of infections.
The relocation of critically endangered plants and animals also plays a role here as part of rescue programs organized by, for example, the International Fund for Animal Welfare (IFAW) and a number of other organizations. In the last few decades alone, there have been several hundred relocations of livestock and wildlife worldwide without recording their health status or systematically monitoring their morbidity. To this can be added harvested timber as well as agricultural and food products international mass transport. Another vector spreading infectious diseases are the dozens of species of microorganisms (viruses, bacteria, protozoa) and multicellular parasites that contaminate wastewater. Therefore, some of the most serious infections are spread, especially in third world countries. Their incidence and number of victims are quantified in millions and are constantly changing. Up-to-date information can be obtained from the relevant WHO references [22]. Another potential risk is bioterrorism, the misuse of highly virulent pathogenic microorganisms capable of causing difficult-to-manage epidemics. Potentially, these are mainly viral (hemorrhagic fevers) and bacterial (plague and anthrax) infections [8,9].
COMMUNICATIONS DISEASES AFFECTING THE CURRENT GENERATION
‘Old’ infectious diseases
These include, in particular, tuberculosis, which still affects a large part of the world's population, regional leprosy and cholera. This latter is an indicator of the social and hygienic conditions that millions of refugees and migrants find themselves in (see above) remaining therefore a global threat. According to the WHO, it still affects 1.3 to 4 million people a year and causes 21,000 to 143,000 deaths a year. While some diseases were the causes of epidemics and pandemics that destroyed humanity more than wars, others, such as diarrheal diseases, malaria, measles and twentieth-century diseases, AIDS are also dangerous. Pertussis, cryptosporidiosis and hepatitis C and Mycobacterium leprae, which are still surviving in leprosarium’s, are also considered to be potentially threatening [23].
New Infections
Over the past fifty years, a number of previously unknown and undiagnosed infections have emerged. These mainly include AIDS, and a number of hemorrhagic fevers of viral origin, namely Ebola caused by filoviruses derived from monkeys (recorded in 1976). Between 2014 and 2016, local epidemic arose in West Africa (Guinea, Sierra Leone and Liberia), and in Congo between 2018 and 2020. Due to strict, uncompromising anti-epidemic measures, enforced by high mortality, which ranged from 40 to 60%, the foci were eliminated before an active vaccine was developed. New viral hepatitis, new influenza diseases (caused by H5N1, H7N7, H1N1 viruses) and coronaviruses (SARS, MERS, SARS-CoV-2) also developed (Table 3). Typical features of these diseases include their rapid spread and acute course. The vast majority of their agents is pathogenic, especially for humans, and begins as anthropozoonoses.
The disease was described as early as 1872 by the Hungarian physician M. Kaposim, rare at that time, today it mainly affects patients with impaired immunity (AIDS).
At the beginning of this century, completely new epidemic diseases appeared, caused by corona viruses (Coronaviridae). The first human coronavirus was discovered by the Scottish virologist JD Almeid (1930-2007) as early as 1964 [24]. The first epidemic of the disease occurred in 2002-2003, and because it was characterized by severe breathing difficulties, it was called Serious Acute Respiratory Syndrome (SARS). In 2012, a new coronavirus disease appeared in Saudi Arabia, which spread to 27 countries in the Mediterranean, Africa and Asia. It was referred to as MERS (Middle East Respiratory Syndrome) and manifested by an inflammation of the lungs and digestive system. As an anthropozoonosis, its original source of infection was bats and it was transmitted to humans from camels [25-27]. We are currently witnessing a completely new pandemic, which is again caused by coronaviruses. The disease broke out in 2019 and has since spread globally. In the short time taken by the disease to spread, dozens of studies, often contradictory, have been published. However, it is still too early to evaluate accurately its course or the number of infected people or deaths. Current data can again be found on the WHO portals [28].
CONCLUSION
Despite the unmissable achievements of biomedicine, humanity will still be threatened by both recurring and emerging infectious diseases. Some diseases (namely poliomyelitis) are already approaching eradication, but others, mainly caused by viral pathogens (influenza, hepatitis and similar viruses), are not yet close to disappear. We still have to reckon the high genetic variability of viruses, antibiotic resistance of pathogenic bacteria and adaptability of multicellular parasites or their vectors. Potential problems could also arise from permafrost thawing. In the future, practicing traditional preventive measures, such as basic hygienic anti-epidemic measures or restricting the movement of people in an effort to prevent the spread of infections in the community would not be enough. The development of reliable diagnostic tests, effective and at the same time safe vaccines as well as new effective medicines is primordial. Regarding the testing and tracing of contacts, it is important especially in the initial phase of the epidemic before mass, community spread, i.e., in the phase enabling effective tracing and subsequent isolation of contacts.
Monitoring of SARS-CoV-2 in municipal wastewater using RNA polymerase reverse transcription (RT-qPCR) is now considered as a promising tool for virus surveillance and impeding epidemic prediction [29]. Within endangered, high-risk areas, adopting social programs to improve living conditions, including tolerable hygiene standards for local populations, ensuring early detection and reliable identification of the pathogens, early initiation of the above-mentioned anti-epidemic measures and clear identification of the population at risk of infection, are desirable steps. The occurrence of the current SARS CoV-2 pandemic is considered positive in the sense that it is a ‘wake-up call’ for a situation in which an epidemic such as a virus with mortality at the Ebola level develops. In this context, criminally enforceable rules could be voted to palliate the often indiscipline of part of the population.
ACKNOWLEDGEMENTS
The authors thank for the support of the grant COVMON security research MV4 VSBV III.
- Stewart WH (1968) Symposium on circumpolar health related problems, July 23-28, 1967. Opening remarks. Arch Environ Health 17(4): 460-461.
- Mahler H (1977) Worldwide smallpox eradication: 1977. Nord Med 92(10): 236-240.
- Fenner F, Henderson DA, Arita I, Jezek Z, Ladnyi ID (1988) Smallpox and its eradication. Geneva: World Health Organization. Available online at: https://apps.who.int/iris/handle/10665/39485
- Boylston AW (2012) Defying Providence. Smallpox and the forgotten 18th century medical revolution. Charleston, SC: CreateSpace, 2012. 282 pp: ISBN 978-1478232452.
- WHO (1982) Archives of the smallpox eradication program, a guide and inventory. Geneva.
- Black FL (1975) Infectious diseases in primitive societies. Science 187(4176): 515-518.
- Sakula A (2021) Robert Koch: Centenary of the Discovery of the Tubercle Bacillus [online]. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1790283/pdf/canvetj00269-0053.pdf
- Riedel S (2005) Anthrax: A continuing concern in the era of bioterrorism. Proc (Bay Univ Med Cent) 18(3): 234-243.
- Klement C (2020) Biological weapons and bioterrorism - a permanent role for public health. Hygiene 65(1): 3-4.
- Koch R (1876) The etiology of environmental public health, based on the developmental history of Bacillus Anthracis. Contrib Plant Biol 2: 277-310.
- CDC (2021) History of Anthrax [online]. Available online at: https://www.cdc.gov/anthrax/resources/history/index.html
- Budianski S (1997) The covenant of the wild: Why animals chose domestication. London: Phoenix.
- Karamanou M, Panayiotakopoulos G, Tsoucalas G, Kousoulis AA, Androutsos G (2012) From miasmas to germs: A historical approach to theories of infectious disease transmission. Infez Copper 20(1): 58-62.
- Wikipedia (2021) Miasma theory [online]. Available online at: http://broughttolife.sciencemuseum.org.uk
- Infectious diseases at the Edward Worth library (2021) Theory of Contagion [online]. Available online at: http://infectiousdiseases.edwardworthlibrary.ie/theory-of-contagion/
- Oldstone MBA (2020) Viruses, plagues and history: Past present and future. New York: Oxford University Press.
- Gibbon E (1983) The Decline and Fall of the Roman Empire: Committee. 1st Prague: Odeon.
- Karlen A (1995) Plague’s progress: A social history of man and disease. London: Indigo.
- Malthus TR (2003) An essay on the principle of population. Available online at: http://www.esp.org/books/malthus/population/malthus.pdf.
- Bencko V (2011) Primary disease prevention: Current pitfalls and opportunities. (In Czech) Prakt Lék 91(3): 127-130.
- Warren JR, Marshall B (1983) Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet 1(8336): 1273-1275.
- WHO (2021) World Health Data Platform [online]. Available online at: https://www.who.int/data
- White Franco-Paredes C (2015) Leprosy in the 21st Clin Microbiol Rev 28(1): 80-94.
- Almeida DJ, Tyrrell DAJ (1967) The morphology of three previously uncharacterized human respiratory viruses that grow in organ culture. J Gen Virol 1(2): 175-178.
- Šíma P (2003) Infectious diseases do not end there. Universe 82: 443-445.
- Coronaviridae Study Group of the International Committee on Taxonomy of Viruses, Gorbalenya AE, Baker SC, et al (2020) The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol 5(4): 536-544.
- WHO links: https://www.who.int/data
- Mlejnková H, Sovová K, Vašíčková P, Očenášková V, Jasiková L, et al. (2020) Preliminary study of SARS-Cov-2 occurrence in wastewater in Czech Republic. Int J Environ Res Public Health 17: 5508.
- Lowe N, Bencko V (2021) Using wastewater-based epidemiology as an upcoming tool for the prediction and control of COVID-19 disease outbreaks. Am J Biomed Sci Res 14(2): AJBSR.MS.ID.001975.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Oncology Clinics and Research (ISSN: 2643-055X)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)



