INTRODUCTION
In the United States (U.S.), children are required to receive vaccines before entering kindergarten. However, 17 states, including Utah, allow parents to exempt their children from vaccines based on medical necessity, religious beliefs, or personal choice [1]. Of these three types of exemptions, the most common reason Utah parents request exemption from school vaccination requirements is personal choice. In fact, the vast majority of U.S. school-aged children who are unvaccinated are exempted because their parents do not personally believe in vaccinations [2].
Vaccine exemptions for personal reasons are on the rise. In Utah, vaccine exemptions for personal reasons rose from 2.1% in 2007 [3].to 5.3% in 2017 among kindergarteners [4]. Because of the increase in vaccine exemptions, outbreaks of vaccine-preventable diseases (VPDs) have become more common in Utah. For example, in 2015 the incidence of pertussis in Utah was more than double the national average [5]. In addition, [6]. named Salt Lake County the 19th most at-risk county in the U.S. to experience disease outbreaks (namely measles) due to both high vaccine exemption rates and influx of air travelers from disease-afflicted regions.
The school setting is a prime environment for transmission of infectious disease due to close proximity of students for extended hours during the school day [7]. In 2017, 45% of pertussis outbreaks identified in Salt Lake County occurred in school-aged children [8]. Children attending charter schools are particularly at risk for developing VPDs since students are 2.3 times more likely to have a non-medical exemption compared to students at public non-charter schools [9]. Consequently, the largest pertussis outbreak in Salt Lake County in 2017 occurred in a charter school with a vaccination exemption rate of 11% [8]. In addition to decreased community immunity, vaccine exemptions put vulnerable populations at risk for VPDs [10]. In 2017, a pertussis outbreak in Salt Lake County occurred in a school for children with disabilities [8]. Children with certain disabilities, who are immunocompromised, are at greater risk for developing complications from VPDs [11,12].
School nurses are strong advocates for childhood health and wellness. The National Association of School Nurses [13]. recognizes that school nurses are leaders who protect and promote student health through evidence-based practice and collaboration. As leaders in their respective communities, school nurses use their expertise to provide effective education on health promotion and disease prevention topics and, as a result, reduce health care costs. Cost-benefit analyses have shown school nurses are effective health advocates whose leadership results in a net benefit for schools and communities [14].
Researchers have also identified the key role school nurses play in equipping students and families with knowledge and skills to prevent the spread of disease. According to Lineberr [15], significantly fewer students become ill after school nurse led interventions on infection prevention. When school nurses lead school disaster planning teams, the schools had improved disaster preparedness scores when compared to schools with non-school nurse led disaster planning teams [16].
During a disease outbreak in the school setting, a school nurse may have a significant impact on controlling the spread of VPDs. Researchers have examined the positive effect school nurses have on vaccine compliance [15]. but few have explored the role of school nurses in managing a disease outbreak [17].
The theoretical underpinnings of this study are based upon the Roy Adaptation Model [18]. which incorporates concepts from Helson’s Adaptation-level Theory of Perception [19]. According to these theorists, humans are in constant interaction with their environment and respond holistically to changes. The environment requires a person to adapt and changes can be positive or negative [20]. During a disease outbreaks school nurses must adapt to the increased workload to properly care for students.
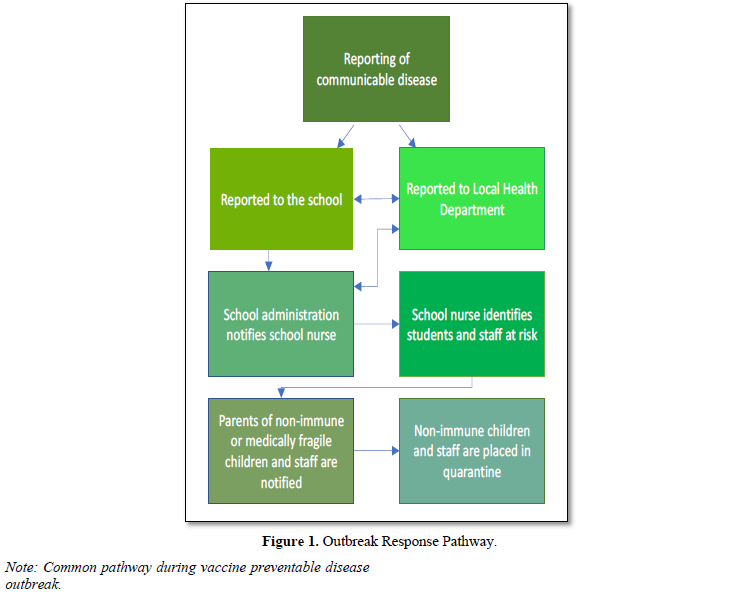
In Utah’s 41 school districts, it is unknown if schools and school nurses have clearly defined guidelines for action during a disease outbreak. Therefore, the purpose of this study is to explore the following research questions (Figure 1).
- What are the responsibilities of Utah school nurses in the event of a disease outbreak?
- What disease outbreak training do Utah school nurses receive?
- What other groups do school nurses collaborate with when controlling a disease outbreak in a Utah school?
- What is the greatest concern of Utah school nurses during disease outbreaks?
METHODS
Eligible participants in this study were school nurses currently employed in the state of Utah. Inclusion criteria also involved attendance at the 2017 Utah School Nurse Association (USNA) Conference and a willingness to participate in a focus group held during the conference.
After receiving Institutional Review Board approval, the USNA President granted permission to conduct focus groups during the April, 2017 USNA Conference. Emails were sent to registered conference attendees two weeks before the conference. Attendees were notified of the study and invited to participate in the focus group. Interested participants were asked to email the researchers so their name could be added to a list of potential focus group participants. Participants were then scheduled for a focus group on the same day as the USNA Conference.
Three focus group sessions, each with eight participants, were assembled for data collection. A member of the research team informed participants of the study purpose and answered any questions prior to data collection. Informed consent documents were collected, and each participant was given a copy of the consent document. Focus group sessions lasted 45 min and were led by a member of the research team. Discussion was guided by four global questions: 1) describe your responsibilities in the event of a disease outbreak; 2) explain any training you received specific to disease outbreaks in schools; 3) what departments, individuals, or groups do you coordinate with during a disease outbreak; and 4) what is your greatest concern regarding disease outbreaks? At the conclusion of each focus group, participants were thanked by a member of the research team and reminded that all personal identifiers would remain confidential. Participants were given a 20-dollar gift card and refreshments in appreciation for their participation.
The semi-structured interview guide for focus groups was developed by public health experts from the Utah County Health Department and vaccine experts from the Utah Scientific Advisory committee, in addition to the expertise of the research team members. The interview guide was used to assess Utah school district disease outbreak plans and the role of school nurses during disease outbreaks.
A member of the research team transcribed audio recordings of two of the focus groups verbatim. The third focus group audio recording was damaged and thus only field notes were available for analysis. Field notes, taken by the group moderator, captured verbally expressed information which was also analyzed by the research groups for clarification and emerging themes. To ensure accuracy of the transcription, two research groups (each with two researchers) conducted an independent content analysis, coding and analyzing each open-ended response. The synthesized data and codes were then compared until consensus was reached. Additionally, another researcher with qualitative inquiry expertise verified the findings by conducting an independent analysis of content and themes.
There were 24 total participants, all actively employed Utah school nurses, and all self-identified as white. While not all 41 Utah school districts were represented, many of the largest school districts in the state were represented including Alpine, Davis, Jordan, Salt Lake, and Washington. The vast majority of participants were female, with only 1 male participating in the study. Twenty participants reported at least 8 years of experience in school nursing, and 14 participants had been involved in a VPD outbreak. Additionally, half of the school nurse participants reported they provided care for at least 5 schools. The results were organized into thematic descriptions with illustrative quotes in response to the four global questions: responsibilities, training, collaboration, and concerns.
When participants were asked about responsibilities as school nurses during disease outbreak, they described a variety of duties. Currently the response to a disease outbreak in Utah schools follows a general pattern (Figure 1) but varies according to the type of VPD as well as school district and local health department (LHD) policies. In the case of a VPD outbreak, action begins when a primary care provider (PCP) diagnoses a school-aged child with a reportable disease and contacts the LHD. The LHD then contacts the school administrator at the affected child’s school, who then notifies the school nurse. Occasionally a parent simply calls the school to report their child’s illness and the school administrator contacts the LHD and the school nurse. In some school districts, it is the responsibility of the school nurse to file an official VPD with the LHD where the case, including disease history and symptoms, is reported.
Depending on the disease, a certain number of cases must be reported in a classroom before more action is taken, which varies by district and health department policies. Managing the VPD outbreak begins under the guidance of the LHD with strong collaboration between the LHD and the school nurse. School nurse participants collectively commented on the integral role the LHD played during a disease outbreak. As one participant stated the (local) health department has been so excellent as far as giving us direction, letting us ask questions, [and] providing documentation that needs to be sent out to the parents. So, we work very hard in conjunction with the (local) health department.
The school nurse and LHD work quickly to prevent the spread of disease and have several tasks to complete in a short period of time. The school nurse must confirm the disease with the child’s PCP and parents. One school nurse participant described the process:
What we do is call the [healthcare provider’s] office to find out if it’s been confirmed, because a lot of the times we hear second hand from parents or other students and teachers and we call and find out the source.
The school nurse then identifies students and staff who are not fully vaccinated against the disease to which they may have been exposed. Non-vaccinated staff and parents of non-vaccinated students are notified of the presence of the disease in the classroom through letters, emails, or personal calls and given options for action based on the VPD. Children and staff who are unvaccinated against the disease in the outbreak is excluded from school, ranging from a few days to a few weeks or, for some diseases, students may choose to receive antibiotic treatment and then return to school. School nurses also identify and notify others who may have been exposed to the disease, as well as children in the school who are medically fragile. Under the direction of the school administrator, the nurse may opt to send a letter about the disease and its symptoms to parents of children in the affected classroom or the entire school. One nurse commented on the collaborative decision-making process: “I always make a suggestion or recommendation but [administrators] ultimately have the final say of what they want to do [regarding methods of communication with parents].”
When participants were asked about disease outbreak training, several Utah school nurses reported receiving little to no formal training on managing a VPD outbreak prior to an actual event. When a VPD outbreak occurred in their school, school nurses used the Centers for Disease Control and Prevention guidelines and collaboration with the LHD to manage the outbreak. Participants reported being unsure about district specific guidelines in managing a VPD outbreak and relied on contact with the LHD. One school nurse participant described her experience. Well, I’m a new school nurse this year and I only learned about [the guidelines] when I had a [student with] chickenpox and my boss was out for surgery and so the epidemiology people at the county told me what to do.
There were very few Utah school nurses who received VPD outbreak training as part of their hiring process. One participant reported an optional training program available on the school nurse website; however, training topics vary from year to year and are not always geared specifically toward managing disease outbreak. Overall, Utah school nurses stated there was no policy or specific VPD outbreak training required.
In addition to a lack of standardized VPD outbreak training, available resources to manage an outbreak also varied, particularly between LHD-employed nurses and school district-employed nurses. Eight school nurse participants in this study were employed by a LHD, rather than the school district. Several participants who were employees of a LHD reported they only received VPD outbreak management training “once in a while.” Some school nurses stated they had a disease outbreak guidebook that was provided by the school district or LHD, while others had only a phone number for a contact at their LHD. One school nurse participant voiced her frustration about outdated resources when she noted that the “the state health department has developed a communicable disease book on what to do, but it’s from 2007”.
COLLABORATION/COMMUNICATION
When school nurse participants were asked what other groups were involved in controlling a disease outbreak, the collective response detailed a multifaceted collaboration with the LHD, school administrators, and PCPs.
LOCAL HEALTH DEPARTMENT
Participants agreed that communication with the LHD was essential in managing a VPD outbreak. Not only did the LHD provide guidelines on controlling a VPD outbreak, it was also a source of authority. Several participants illustrated a cohesive and positive working relationship with the LHD, often referring to LHD as their guide. One nurse elaborated:
I think the [local] health department has done a really good job of giving us [de]lineated algorithms on what to do. We don’t even have to second guess[ourselves], we know exactly what to do. It’s so nice to go immediately to the [local] health department and get that resource going.
Although nurses described a strong working relationship with the LHD, they noted that specific policies regarding VPD outbreak management varied between school districts. One school nurse commented that while she did not know initially how to manage an outbreak, she “knew to call epidemiology” at the LHD. She also stated, “I had a paper that had their phone numbers on it but I didn’t have any idea what to do from there.”
Variability in VPD outbreak management also exists in employment as school nurses can work for the district, state, LHD, or even a private agency. One school nurse participant employed by her school district noted that while her relationship with the LHD was “good” it was “just not as fluid as for [nurses who worked for the local health department].” She continued:
I don’t work for the [local]health department, I work for the [school]district…If I need to call up epidemiology, they don’t know who I am and there’s not that communication that’s helping with those type of things.
Participants described the LHD staff as readily available to answer questions and concerns, and school nurses often utilized LHD resources, such as literature. School nurses noted that the frequency of telephone communication with the LHD varied based on the situation. One school nurse said she called once a month with vaccination questions, while another school nurse called 2 to 3 times a day for guidance on how to manage a pertussis outbreak in one school.
When disseminating VPD outbreak information or excluding students, school nurse participants described their role as a messenger. School nurses relied heavily on the LHD for support, especially when informing parents that their unvaccinated child would be excluded, or be unable to attend school, due to risk of disease transmission. Participants reported that parents and administrators often perceived the LHD’s word to hold more value than what the school nurse said, so school nurses utilized their partnership with the LHD to disseminate information, because, as one participant explained, the LHD holds greater authority due to “government backing.” One school nurse summarized:
Working with the [local] health department or working in conjunction with them, you’ve got them behind you. So, it’s not just ‘the school nurse says this,’ it’s the [local] health department has this mandate. It has to be handled this way.
Participants discussed the importance of maintaining a strong team dynamic with the LHD and establishing an authoritative presence. School nurses perceived this alliance as a way to improve cooperation among parents and school administrators during a VPD outbreak.
SCHOOL ADMINISTRATORS
Problems communicating with school administrators was one of the most common barriers to Utah school nurses trying to manage a VPD outbreak in the school setting. Some school nurses described the feeling of being left out of the loop of communication in a VPD outbreak because school secretaries contacted the LHD directly about the presence of a reportable disease but never contacted the school nurse. School nurses also explained that school administrators may wait for the school nurse’s next routinely scheduled visit to their school before informing them of a VPD in the classroom. This delay in communication between school administrator and school nurse could be days, even weeks after exposure, putting unvaccinated children who should be excluded from school at risk. One nurse commented:
I know that [failing to contact the nurse about illness in the classroom] was an issue with some schools no matter how many times I told them, ‘You’ve got to let me know by email or call. I need to know this.’
Utah school nurses also emphasized that the working relationship with school administrators must be strong to enforce student exclusions from school, because the nurse is not in the school every day. When there was not a clear understanding of the importance of compliance with student exclusions during a VPD outbreak, the school nurse’s ability to effectively prevent the spread of disease in classrooms was impaired. One nurse expressed frustration over an incident which involved a faculty member who allowed an exempt student to come after school to audition for the school play, saying: “That is totally not ok. And I had to deal with that but my principal and administration were so onboard with [following correct procedures].” Preventing the spread of VPD in the school setting is a team effort which requires interprofessional cooperation and communication.
PRIMARY CARE PROVIDERS
School nurses also experienced problems in communication with PCPs, who were usually responsible for reporting or confirming the diagnosis of a VPD. School nurses described that often PCPs do well in reporting diseases to the LHD. However, PCPs or office staff will at times give parents information that conflicts with the information from the school nurse. For example, one nurse described a parent bringing in a note from the PCP during an outbreak, saying their child could be in school without the required antibiotic treatment, because the parent accepted the risk. The school nurse, however, could not accept the note and had to inform the parent that the child needed to receive treatment or remain out of school for the required number of days, regardless of what the PCP said.
School nurse participants also voiced frustration about PCPs not actually testing for a VPD but just assuming and treating symptoms. One nurse recalled her experience, saying, “Parents hear that [their child was diagnosed with a communicable disease] and they call the school and say, ‘My kid has pertussis’ when actually maybe they do, maybe they don’t.” Nurses must then rely on the LHD for follow up with the PCP in order to confirm a VPD.
School nurses expressed many concerns about managing a VPD outbreak, including concern for medically fragile students, inefficient communication with community members, lack of vaccination records for school staff, and the high nurse-to-student ratio.
MEDICALLY FRAGILE STUDENTS
A few nurses expressed concern for medically fragile students during a VPD outbreak, because guidelines for safely managing these students are not clear. Medically fragile students are more susceptible to disease; therefore, precautions should be taken to protect these vulnerable students. However, school nurses expressed unease about being able to manage these students. School nurses were especially concerned that because of communication delays, they may not be notified of VPDs in the classroom or school in time to notify parents of medically fragile students. As one nurse reported, “I mean I always worry, like, will I get to these parents on time to make sure they’re really out of school as soon as they need to be?”
Some school nurses rely on school administrators to notify them of diseases in classrooms with medically fragile students, while other school nurses ask the teachers to notify them. Because there is no standard for dealing with medically fragile students, nurses create their own systems, tailored to individual students. Thus, nurses were concerned they would miss somebody or not be notified in time to effectively protect a medically fragile student.
COMMUNICATION WITH COMMUNITY
Communication with community members through social media have also presented problems for school nurses. During a VPD outbreak, communication with parents is essential. In fact, during a disease outbreak, many parents attempt to contact school nurses for information. School nurses described the essential role the LHD played during a VPD outbreak to help field calls from concerned parents. School nurses also described problems with social media as alarmed parents share feelings or false information, leading to panic in the community. During a disease outbreak, the school is frequently inundated with phone calls and school nurses are often responsible to address angry and frightened parents. For school nurses, this process of communication is time-consuming and frustrating. Participants agreed that while answering questions was not specifically a barrier, the amount of effort required considerable amount of time away from other duties. One nurse described an event that illustrates complications and parental reactions surrounding an outbreak:
Part of the problem was we were having the school play and kids in the school play had pertussis. And so, you’ve got, ‘what am I gonna do with this play because my lead has pertussis!’ And parents get kind of agitated some of the students were so upset about being excluded but the parents would not give in.
School nurses must also be cautious because community members may identify and share which children in the classroom are infected with a disease, resulting in a breach of confidentiality for infected children. Participants reported lack of training regarding social media messages and, therefore, struggled with how to manage the repercussions from messages shared by parents on social media.
TEACHER AND SCHOOL STAFF VACCINATION RECORDS
One issue many Utah school nurses addressed was the lack of vaccination records for teachers and staff. In a VPD outbreak, non-vaccinated teachers and staff must also be excluded from school. However, most school districts have no vaccination records for teachers and staff since reporting vaccination status is optional in most Utah school districts. The lack of vaccination records presents a problem for school nurses, who then must spend their time identifying non-vaccinated staff. In a VPD outbreak, a timely response is essential for preventing the spread of disease, and school nurses expressed frustration about spending so much time helping staff review their individual vaccination records and determine who needed to be quarantined. In addition, staff may also be excluded from school or be required to receive vaccinations because they cannot find their records quickly enough. One school nurse commented, “20-50 employees trying to call their moms to look through their baby book [to find vaccination records.] That’s what it was! And then they were bringing me their baby books”.
HIGH NURSE-TO-STUDENT RATIO
Participants identified the Utah school nurse-to-student ratio as a major barrier to effective management of a VPD outbreak. On average, Utah school nurses reported covering 5-15 schools or about 4,500 students per nurse, visiting each school every few days or sometimes once every 2 weeks. School nurses also reported difficulty in effectively managing emergencies in schools because of travel distance between the schools they served: “You’ve got to think about the driving time. If you’re thinking 4,500 kids but they’re separated you are going and going and it’s not like it’s 2 min across the street.” Because of the high nurse-to-student ratio, school nurses struggle to complete daily tasks, in addition to tasks related to VPD outbreaks.
Supportive of previous research, nurses in this study described heavy workloads in the face of time constraints and limited resources [15]. Areas of greatest concern voiced by school nurses in this study included staff vaccination records, high student-to-nurse ratio, and communication challenges.
STAFF VACCINATION RECORDS
School nurses identified the act of contacting staff members about their vaccination status as one of the most time-consuming tasks in a VPD outbreak. Since teachers and school staff must also be excluded from school if not immune, it is logical that staff members should report their vaccination status to the school upon hire. The impact of the time-consuming task of gathering this information can create an immense barrier to positive student and community health outcomes. For example, non-vaccinated staff members pose a physical threat to students as they could potentially carry and spread disease [21]. Additionally, securing substitutes for teachers who must be quarantined because he or she is unvaccinated or cannot locate their vaccination records poses a financial burden [22]. Thus, requirements for teachers and staff members to report their vaccination status upon hire would reduce spending and protect students in an outbreak.
Participants reported that a major barrier to effective VPD outbreak management was the high nurse-to-student ratio. Unfortunately, the school nursing shortage is not unique to Utah. In fact, 12 other states (California, Colorado, Florida, Idaho, Illinois, Michigan, Montana, North Dakota, Ohio, Oklahoma, Oregon, and Wisconsin) reported high nurse-to-student ratios ranging from 1:2,000 to 1:4,000 [26]. In contrast, the [27]. recommends at least one full-time nurse in every school and one nurse for every 750 students [28]. According to the [29] the nurse-to-student ratio in Utah is 1:4,100. The overwhelming number of students, in addition to travel distance and time between schools becomes problematic in the event of a school emergency. A compounding difficulty to travel distance and time was the limited hours allotted specifically for school-related duties for nurses working for both the school district and LHD. Because of time constraints created by job roles and travel distance, school nurses may struggle to complete required tasks.
School nurses strongly agreed that a lower nurse-to-student ratio would allow them to work more effectively in all aspects of their job. The current high nurse-to-student ratio is a result of lack of funding for school nurses [30]. Greater funding for school nurses would allow more nurses to be hired, decreasing the nurse-to-student ratio. However, while standardized nurse-to-student ratios have been widely recommended, [31]. and [27]. stress the importance of an evidenced-based workload model that mirrors the diverse needs of students and complex health needs.
Ineffective communication was an underlying theme in barriers to VPD outbreak management. Comparatively, numerous studies identify ineffective communication as a major barrier to the school nurses’ roles in general [32-34]. Coordination of care during a VPD outbreak requires ongoing communication among school nurses, LHD administrators, PCPs, and parents [35]. Since school nurses are not in daily contact with all their assigned schools, communication with school administration can be ineffective. Because of this lack of daily communication, school administrators may fail to report diseases promptly. Consequently, faculty’s perception of communication barriers was directly influenced by the time school nurses spent on-site [36]. Additionally, timely communication between school nurses and administration has been identified as a primary element of student health [37]. prompting reevaluation of current disease-reporting practices in schools.
Communication barriers were exacerbated by the lack of continuity between school nurses and PCPs regarding parent education about vaccination and quarantine policies. Therefore, an evaluation of disease-specific training among school nurses and PCPs is warranted. It is, therefore, reasonable to consider that standardized training of PCPs and school nurses regarding statutes and guidelines may improve communication and allow for continuity between the VPD information provided by school nurses and other PCPs. While there are gaps in the literature regarding specific training geared toward VPD outbreaks for both nurses and PCPs, subject-specific training and resources builds knowledge and confidence in school nurses. which may support communication efforts.
IMPLICATIONS FOR SCHOOL NURSING
The results of this study have several implications. VPD outbreak training for school nurses could be vastly improved and would help nurses work more effectively during outbreaks, thus decreasing the number of exposures to VPDs. School nurses in the focus groups stated they either did not receive training regarding how to manage a VPD outbreak, or that they rarely received training. Many expressed a desire to receive more training on VPD outbreak management, or at least receive materials outlining the actions they should take during a VPD outbreak.
Implementing standardized training and resources for school nurses in each school district or LHD would help nurses feel more prepared for VPD outbreaks. School nurses expressed that it would be helpful to include VPD outbreak management as part of a standard training upon hire, followed by periodic reviews. Additionally, orientation would also include access to an updated manual or guidebook.
Training may include introductory and periodic seminars or webinars specifically about VPD outbreak management. Access to training should be convenient and be offered both online and in-person, to cater to school nurses’ busy schedules and learning preferences. Online training modules should offer simplified refresher courses in VPD outbreak management, to allow school nurses an opportunity to review guidelines without inundating them with tasks. In addition, School Nurse Summer Institute, which is currently an optional educational event for school nurses, could be a valuable platform for VPD outbreak management training.
Registration for Utah’s School Nurse Summer Institute can be accessed online at http://choosehealth.utah.gov/prek-12/school-nurses/trainings/events.php and offers in-person workshops on various subjects each year. Workshops generally cost participants between $15-$30 and counts towards Continuing Nursing Education (CNE). Attendance to the School Nurse Summer Institute may improve networking among new school nurses and provide an educational foundation for VPD outbreak management.
Nurses also noted the need for specific training on how to deal with the issues that come from social media, like community panic and upset parents during VPD outbreaks. Improving communication requires that school nurses have access to updated evidenced-based information to address parental concerns. Effectively communicating with parents using updated guidelines, especially parents who are upset or angry, would also be helpful to include in this training. Currently, the Utah Department of Health’s EPPIC program, which stands for “Healthy Living through Environment, Policy, and Improved Clinical Care” (emphasis added), has a communicable disease handout that includes basic communication strategies with parents and school administration regarding vaccinations. While the handout does not specifically address how to communicate via social media, the approach (e.g., listen, welcome questions, address parent using evidence-based research, base approach on knowledge of family, etc.) can be a useful tool for any school nurse addressing parental concerns. The handout entitled, “Communicable Disease,” can be found at: http://choosehealth.utah.gov/documents/pdfs/school- nurses/School_Nurse_Seminar_Handouts/Communicable _Disease_Handout.pdf.
This study had several limitations. The sample size was relatively small, with only 24 school nurses participating overall. In addition, data from one focus group audio recording was damaged and irretrievable. Field notes were taken during all focus group sessions as both a safeguard against technology failure, as well as an adjunct to transcribed data. While key findings can be discovered within two to three focus groups. The loss of one recording may impede saturation potential. The study was also based on a convenience sample rather than a random sample of nurses. The sample of nurses was restricted because only members of the USNA who were attending the 2017 conference had the opportunity to participate in the focus groups. The study was also limited in that not every Utah school district was able to be represented in a focus group, though the state’s largest districts were represented.
RECOMMENDATIONS FOR FUTURE RESEARCH
Understanding how school nurses address disease outbreaks in each school district would be helpful to identify the best path for outbreak containment. Additionally, differences in policy implementation between school district-employed and local health department-employed nurses should be investigated. Furthermore, establishing policies in the state for handling teacher and staff reporting of immunization records would allow for better management of an outbreak. Finally, while policies for medically fragile students are unclear, future research would also be beneficial to develop better management plans for this population.
School nurses are essential in managing disease outbreaks, yet nurses voice concerns that prevent them from working effectively. Many of the concerns school nurses face in managing disease outbreaks are due to missing staff records, high student-to-nursing ratios, communication difficulties, and a lack of training for school nurses. Communication among nurses, school staff, LHD, PCPs, and parents is often disrupted and could be improved by training and policy changes. Managing outbreaks would also be improved if each school district or local health department had clearly defined guidelines for disease outbreaks and policies required teachers, administrators, and staff to report their immunization records. Finally, lowering the student-to-nurse ratio would also assist school nurses to more effectively manage disease outbreaks in the school.