1492
Views & Citations492
Likes & Shares
Major MDR bacteria associated with infections in burn wounds include Pseudomonas bacteria that are Pseudomonas aeruginosa: A highly adaptable pathogen often resistant to multiple antibiotics, making infections difficult to treat.
Methicillin-resistant Staphylococcus aureus (MRSA): A category of Staphylococcus aureus that is resistant to methicillin and other antibiotics in the beta-lactam class. Klebsiella pneumonia another pathogen that founded in the hospital. Acinetobacter baumannii, the bacteria that may because many diseases are resistant to several antibiotic classes, treating them is challenging [3].
The development of resistance to antibiotics is made possible through both use and misuse, presenting serious challenges for physicians. Because these bacteria are resistant to multiple different types of antibiotics, they are especially difficult to treat. Antibiotic resistance became a problem due to overuse and misuse of antibiotics, which presents serious difficulties for healthcare providers that should be careful antibiotic selection, strict adherence to infection control guidelines, and frequently the use of combination medicines are necessary for effective therapy [4].
Burn treatment is challenging due to multidrug-resistant bacteria, such as Pseudomonas aeruginosa and methicillin-resistant Staphylococcus aureus (MRSA). These bacteria are resistant to various antibiotics, making treatment more difficult. Burn care is also impacted by the presence of other resistant bacteria, such as Acinetobacter baumannii and Klebsiella pneumoniae. Addressing antibiotic resistance involves implementing stewardship programs, using combination therapies, and exploring alternative treatments [5].
The purpose of this cross-sectional study was to determine the microorganisms that were isolated from patients with burns and to evaluate how susceptible they were to antibiotics. The study was carried out in Mosul Specialized Center for Burns and Plastic Surgery.
MATERIAL AND METHODS
Ethical appreciation: Ethical approval for current work was obtained from Nineveh Health Directorate, Training and Human Development Centre. To the Mosul Specialized Center for Burns and Plastic Surgery Based on his approval of the new Scientific and Ethical Committee in its session numbered (256) and held in our house on June 5, 2024, on the research project numbered (2024081).
Study design: Current study was conducted to evaluate antibiotic resistance designs in bacteria isolated from burn wound infections in Mosul City, across section study.
Sample Collection: Patients who were admitted with burn injuries provided burn wound swabs. A total of 75 patients from both sexes, ages varying from five weeks to sixty years of age, with third-, second-, and third-degree burns for the period from 3-July-2024 until 5 August 2024.
Procedure of Collection: Sterile try to prevent contamination, sterile techniques were used to remove swabs from the infected burn wounds. Every sample was properly labeled and promptly brought in a sterile container to the microbiology lab. dry cotton swabs were used, then immersed in a sterile natural table salt solution with a concentration of 8.5 mg/L before taking the sample from the mentioned areas. The swabs were placed in tubes containing sterile Stuart carrier medium Reality 5 cm, and then transferred to the laboratory [6].
Bacterial Isolation
Culturing: Following being inoculated into selective media (such as Blood Agar or MacConkey Agar), swabs were incubated for 24 h at 37°C [7].
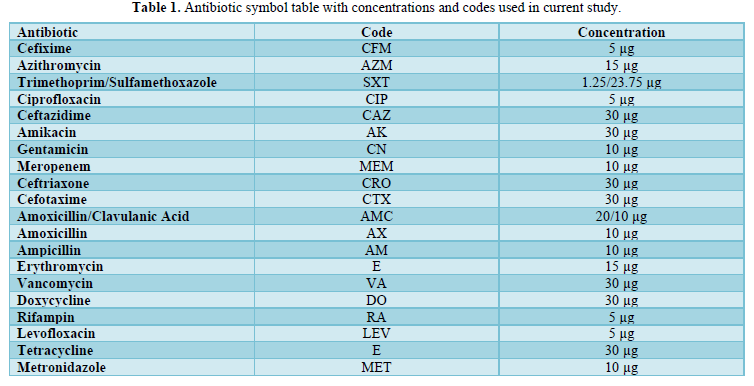
Identification: Isolates identified through culture, staining, and biochemical assays such as oxidase, lactose and maltose fermentation, catalase, and their antibiotic susceptibility assessed via the Kirby Bauer disc diffusion method [8]. sensitivity of antibiotic used as Table 1 that used in present study. Antibiotic sensitivity testing was conducted. Results were evaluated based on NCCLS guidelines [9].
RESULTS
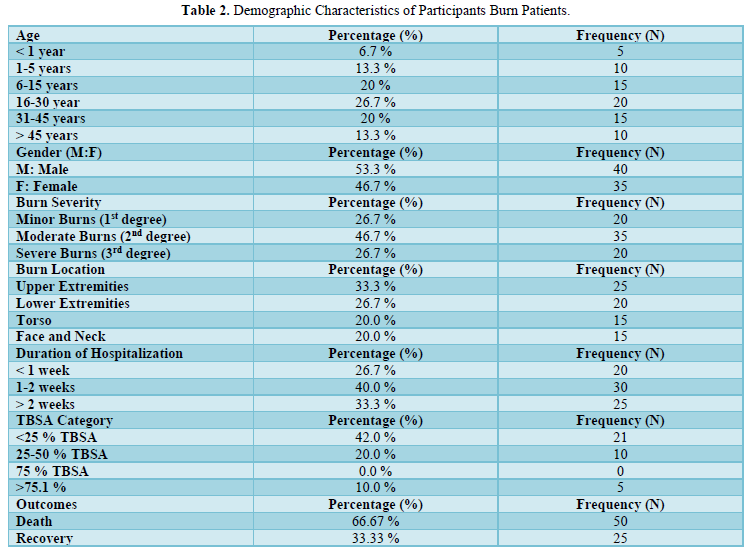
Patients' ages vary widely, and each one of these age groups reflects a different burn injury risk factor: < 1 year (6.7%, 5 patients): Because of their restricted movement and reliance on caregivers, factor related to burn injuries: A broad spectrum of age groups are affected by burn injuries, according to the demographic data. 6.7% of patients are under one year old, and 13.3% are between one and five years old. Twenty percent are older children and adolescents (6-15 years old), with young adults (16-30 years old) making up the largest group (26.7%). Twenty percent of adults are between the ages of 31 and 45, while thirteen percent are above 45. The distribution of genders is about equal, with 46.7% of women and 53.3% of men. Regarding the degree of burns, 26.7% of patients have first-degree light burns, 46.7% have second-degree moderate burns, and 26.7% have third-degree severe burns. The torso (20%), face/neck (20%), lower extremities (26.7%), and upper extremities (33.3%) are among the areas that sustain burns. According to the length of hospital stay, patients spend less than one week in 26.7% of cases, one to two weeks in 40% of cases, and more than two weeks in 33.3% of cases. According to Total Body Surface Area (TBSA) coverage, 42% of patients have burns that cover less than 25% of their body, 20% have burns that cover 25% to 50% of their body, and 10% have burns that cover more than 75% of their body. The results are dire, with 33.33% of patients healing and 66.67% of patients dying from their wounds as showed in Table 2.
Descriptive Statistics
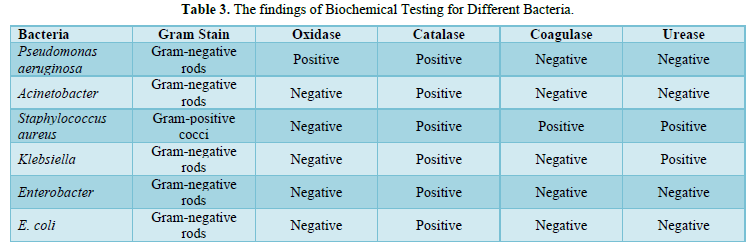
Table 3 presents the biochemical examination results. All isolates were catalase positive. All isolates, except P. aeruginosa, were oxidase negative. Most isolates were urease negative, except K. pneumoniae and S. aureus, which produced urease, altering the media color from yellow to pink. Table 3 further indicates that all S. aureus isolates were catalase positive and oxidase negative. Also, positive coagulase for S. aureus.
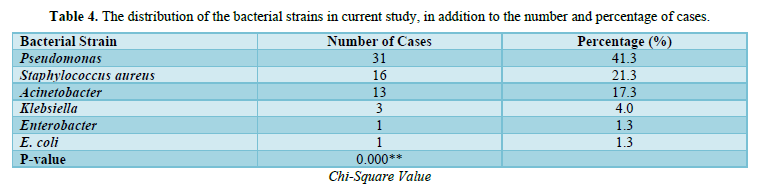
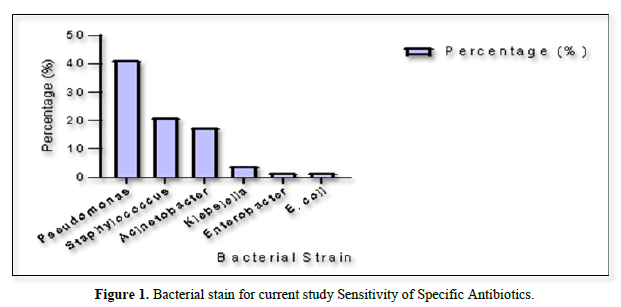
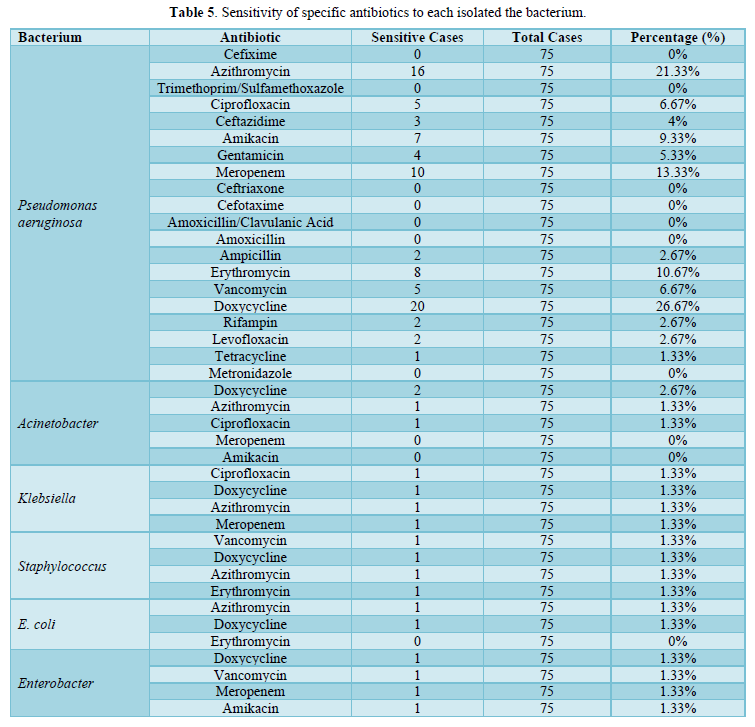
The prevalence of Gram-negative bacteria (GNB) surpasses that of Gram-positive cocci (GPC). The predominant isolate identified was Pseudomonas aeruginosa (41.3%), followed by Staphylococcus aureus (21.3%), Acinetobacter (17.3%), Klebsiella (4%), Enterobacter (1.3%), and Escherichia coli (1.3%) as showed in Table 4 & Figure 1. Various antibiotics were assessed against GNB and GPC. The majority of Gram-negative isolates exhibited sensitivity, with Pseudomonas aeruginosa showing 26.67% sensitivity to doxycycline and 21.33% to azithromycin, while all strains demonstrated resistance to most antibiotics. A comprehensive list of tested antibiotics and their corresponding resistance patterns is documented in Table 5.
DISCUSSION
The age range of 16 to 30 accounts for 26.7% of burn patients, indicating the susceptibility of young people to burn injuries. Due to increasing exposure to work-related dangers, risky behaviors, or household accidents, this age group may be more vulnerable. Children between the ages of 1 and 5 and 6 and 15 also exhibit notable rates of burn injuries, making up 13.3% and 20% of the total, respectively. This demonstrates the greater risk that young children face, possibly as a result of their inexperience with danger and curious nature [10].
A little gender advantage (53.3%) corresponds with an international increase in burns, as men are more likely to participate in jobs with elevated risks such as physical labor and work. A substantial percentage of patients are female (46.7%), possibly due to home accidents in environments where women are largely responsible for cooking or other heating-related tasks [11].
Since of the severity of their damage, the majority of patients (40%) requested longer hospital stays, indicating a need for specialized treatment. A third of the patients (33.3%) needed to stay in the hospital for more than two weeks, most likely as a result of skin grafting procedures, subsequent infections, or complications from severe burns. This highlights the significant strain on healthcare systems and the requirement for sufficient burn care facilities to handle extended medical interventions [12].
With regard to the severity of their injuries, most patients (40%) required longer hospital stays, indicating a need for specialized treatment. A third of the patients (33.3%) needed to stay in the hospital for more than two weeks, most likely as a result of skin grafting procedures, subsequent infections, or complications from severe burns. This highlights the significant strain on healthcare systems and the requirement for sufficient burn care facilities to handle extended medical interventions [13].
Less than 25% of the patients' TBSA was impacted in 42% of them, according to the findings, which is generally associated with better recovery rates. But 10% of patients had burns that affected more than 75% of their TBSA, and a sizable portion of patients (20%) had burns that covered 25-50% of their body surface area. Higher death rates are linked to more TBSA participation because of the elevated risk of complications such infections, fluid loss, and multi-organ failure. The high fatality rate in the study is indicative of this [14]. The high death rate of 66.67% in this demographic is due to burn injuries, highlighting the need for better medical treatments and specialized care. However, a 33.33% recovery rate suggests early-stage therapies can improve mild burn outcomes [13].
The burn wound represents a significant global health issue, with infection being a common and serious complication in burn patients [15]. The biochemical results of this study showed all isolates are catalase positive, crucial for hydrogen peroxide breakdown. All isolates, except P. aeruginosa, are oxidase negative, lacking key O2 receptors found in P. aeruginosa this agree with Tille [16]. Most isolates are urease negative, with K. pneumoniae and S. aureus being exceptions, changing media color from yellow to pink. All S. aureus isolates exhibit catalase positivity and oxidase negativity. The positive coagulase result proves the organism's ability to generate coagulase, aiding in fibrinogen to fibrin conversion. The coagulase test is a reliable method to distinguish S. aureus from other staphylococci like S. epidermidis. This consistent with Brooks [17].
The study's results found that P. aeruginosa is the predominant isolate agree with study conducted in Pakistan by Azam [18] but contradicts retrospective study in turkey by Özkaçmaz [19] which identify S. aureus as the leading organism. The prevalence of Pseudomonas spp. in burn wards is likely attributed to its preference for moist environments. The second most prevalent isolate was S. aureus this finding consistent with Akelma, Yiğit and Yiğit [20]. While disagree with study conducted in Baghdad by Khudhair and AlAubydi [21]. This study demonstrates that P. aeruginosa and S. aureus are the primary isolates in burn injuries, with Acinetobacter spp. as the third most common, followed by Klebsiella spp. These results agree with Khudhair and AlAubydi [21] found that Acinetobacter spp was identified in 1.3% of cases in Baghdad indicated its lower prevalence than other bacteria.
Antibiotic sensitivity patterns guide antibiotic selection effectively. Analysis of burn isolates showed Pseudomonas, the most common isolate, was highly sensitive to Doxycycline (26.67%), followed by Azithromycin. However, other study by Raza [22] reported Pseudomonas as highly sensitive to imipenem and piperacillin this disagree with the present study. In this study meropenem shows low effectiveness (13.33%) against Pseudomonas. This agree with study conducted in Babylon by Alghreri, Alsaadi and Al-Dahmoshi [23] found that 26% sensitive to meropenem.
While disagree with study by Fadhil, Saeed and Saleh [24] in Salah al-din hospital reported that Pseudomonas sensitive 100% to meropenem. Other Gram-negative organisms show high antibiotic resistance, making them less effective against GNB. This result of current study agrees with Haider [25].
Regarding to gram positive bacteria there is no antibiotic sensitive to Staphylococcus Nwankwo and Nasiru [26]. The common gram-positive bacteria Staphylococcus aureus has variable antibiotic sensitivity. Amoxil had little effect on Staphylococcus aureus, whereas streptomycin demonstrated a large zone of inhibition, suggesting sensitivity. This implies that some medicines, such as streptomycin, may be useful against Staphylococcus aureus while other antibiotics are not [19].
CONCLUSION
The study shows that Pseudomonas aeruginosa is the most prevalent infection and that multidrug-resistant bacteria are significantly more common when isolated from burn patients. Pseudomonas spp. shown susceptibility to doxycycline despite being resistant to other antibiotics, indicating that it may be a viable therapy choice for infections brought on by this bacterium in burn victims. The lack of efficacious antibiotics to combat the Gram-positive bacterium Staphylococcus aureus, however, is a significant obstacle in the management of burn-related infections. These results highlight the necessity of continuing to monitor patterns of antibiotic resistance and to develop new therapeutic approaches to effectively manage infections in burn patients.
- Mehta K, Arega H, Smith NL, Gause E, Lee J, et al. (2022) Gender-based disparities in burn injuries, care and outcomes: A World Health Organization (WHO) Global Burn Registry cohort study. Am J Surg 223(1): 157-163.
- Rasool AMA, Karmoosh AS (2024) Multiple Drug Resistance in Burn Patients. J Adv Med Pharm Sci 26(7): 21-34.
- Parrett BM, Pomahac B, Demling RH, Orgill DP (2006) Fourth-degree burns to the lower extremity with exposed tendon and bone: A ten-year experience. J Burn Care Res 27(1): 34-39.
- Alghamdi BA, Al-Johani I, Al-Shamrani JM, Alshamrani HM, Al-Otaibi BG, et al. (2023) Antimicrobial resistance in methicillin-resistant staphylococcus aureus. Saudi J Biol Sci 30(4): 103604.
- Nițescu B, Pițigoi D, Tălăpan D, Nițescu M, Aramă SS, et al. (2023) Etiology and Multi-Drug Resistant Profile of Bacterial Infections in Severe Burn Patients, Romania 2018-2022. Medicina (Kaunas, Lithuania) 59(6): 1143.
- Jain A, Jain R, Jain S (2020) Sterilization of Glassware; Preparation and Sterilization of Media. Basic Techniques in Biochemistry, Microbiology and Molecular Biology: Principles and Techniques; pp: 93-99.
- Abbas ZH, Al-Ethari AYH (2024) Isolation and Identification of Pseudomonas aeruginosa common among microorganisms causing ear infections in Karbala Governorate. J Uni Kerbala 2(1): 32-41.
- Masi C, Gemechu G, Tafesse M (2021) Isolation, screening, characterization, and identification of alkaline protease-producing bacteria from leather industry effluent. Ann Microbiol 71: 1-11.
- Standards NC, for C.L. and Barry AL (1999) Methods for determining bactericidal activity of antimicrobial agents: Approved guideline. National Committee for Clinical Laboratory Standards Wayne, PA.
- Mulatu D, Zewdie A, Zewdie B, Terefe B, Liyew B (2022) Outcome of burn injury and associated factor among patient visited at Addis Ababa burn, emergency and trauma hospital: A two years hospital-based cross-sectional study. BMC Emerg Med 22(1): 199.
- Blom L, Klingberg A, Laflamme L, Wallis L, Hasselberg M (2016) Gender differences in burns: A study from emergency centres in the Western Cape, South Africa. Burns 42(7): 1600-1608.
- Pavoni V, Gianesello L, Paparella L, Buoninsegni LT, Barboni E, et al. (2010) Outcome predictors and quality of life of severe burn patients admitted to intensive care unit. Scand J Trauma Resusc Emerg Med 18: 1-8.
- Yuan, Y, Zhong X, Zhang J, Shen C, Huang G (2023) Artificial dermis combined with split-thickness skin autograft in the treatment of hand thermal compression wounds: A single center case-control study. Front Surg 10: 1304333.
- Żwierełło W, Piorun K, Skórka-Majewicz M, Maruszewska A, Antoniewski J, et al. (2023) Burns: Classification, Pathophysiology, and Treatment: A Review. Int J Mol Sci 24(4): 3749.
- Markiewicz-Gospodarek A, Kozioł M, Tobiasz M, Baj J, Radzikowska-Büchne E, et al. (2022) Burn wound healing: Clinical complications, medical care, treatment, and dressing types: The current state of knowledge for clinical practice. Int J Environ Res Public Health 19(3): 1338.
- Tille P (2015) Bailey & Scott’s diagnostic microbiology-E-Book. Elsevier Health Sciences.
- Brooks GF, Carroll KC, Butel JS, Morse SA (2010) Medical Microbiology. Jawetz, Melnick and Adelbergs. M cGraw-Hill Companies.
- Azam S, Mustafa MZ, Taj MK, Mengal MA, Hussain A, et al. (2024) Drug susceptibility, Prevalence and effect of Pseudomonas aeruginosa on wound healing of burn patients. J Pak Med Assoc 74(1): 67.
- Ozkaçmaz A, Dicle Y, Bayram Y, Parlak M, Akis F, et al. (2024) The Distribution and the Antimicrobial Susceptibility Features of Microorganisms Isolated From the Burn Wounds: A 10-Year Retrospective Analysis. J Burn Care Res 45(2): 384-397.
- Akelma H, Yiğit YD, Yiğit E (2023) Bacterial Isolation and Antibiotic Susceptibility Test Results from Burn Wound Infection in the Southeastern Anatolia Region of Turkey. Artuklu Int J of Health Sci [Preprint].
- Khudhair MK, AlAubydi MA (2023) Determination the prevalence and antimicrobial susceptibility of bacteria isolated from burns and wounds. Iraqi J Agric Sci 54(1): 93-99.
- Raza AA, Ibrahim M, Ishfaq R, Saleem I, Altaf MA, et al. (2022) Incidence, Clinical Evaluation and Antibiogram of Bacterial Isolates Obtained from Burn Patients. Pak J Med Health Sci 16(10): 282.
- Alghreri AAA, Alsaadi KA, Al-Dahmoshi HOM (2022) Prevalence of blaIMP-1 among aeruginosa isolated from patients with burn infections. J Appl Nat Sci 14(3): 1062-1066.
- Fadhil KB, Saeed IO, Saleh MK (2024) Study of the Effect of some Antibiotics on Pseudomonas Aeruginosa Isolated from Wound and Burn Abscesses. Pak J Life Soc Sci 22(1): 2522-2526.
- Haider MH, McHugh TD, Roulston K, Arruda LB, Sadouki Z (2022) Correction: Detection of carbapenemases blaOXA48-blaKPC-blaNDM-blaVIM and extended-spectrum-β-lactamase blaOXA1-blaSHV-blaTEM genes in Gram-negative bacterial isolates from ICU burns patients. Ann Clin Microbiol Antimicrob 21(1): 34.
- Nwankwo EO, Nasiru MS (2011) Antibiotic sensitivity pattern of Staphylococcus aureus from clinical isolates in a tertiary health institution in Kano, Northwestern Nigeria. Pan Afr Med J 8: 4.



