4008
Views & Citations3008
Likes & Shares
Worldwide O A is the most common form of arthritis affecting 3.3% of world population [9,10]. Among those over 65 years approx. 10% male and 18% female are affected [3].
Risk factors: - Primary cause of Osteoarthritis is stress (mechanical) on joints and inadequate self-repair of joints [11]. Stress source can be misalignment of bones due to congenital and pathogenic reasons, mechanical injury, overweight and loss of strength supporting joints, disability of nerves which may cause sudden or unconditioned movement.
- Previous history of joint injury is a major cause of Osteoarthritis, especially with respect to knees OA [12].
- OA is prevalent among postmenopausal women than men of similar age group; this may indicate the role of sex hormone level as one of the causes of development of OA [13,14].
Occupational:- Increased risk of developing knee and hip Osteoarthritis was found among those who work with physically demanding work, lifting, walk at work and have climbing task at work like climbing stairs or ladders [4]. With hip OA in particular, increased risk of developing OA overtime was found among those who work in bent or twisted position. For knee OA in particular, increased risk of development OA was found among those who work in a bow-down or genuflect or curvy position. Those who engage in heavy object lifting specially in kneeling position or work standing up for prolong hour are more prone to OA. Male and female have same occupational risk of having OA.
Systemic risk factors
Age: Aging make changes in musculoskeletal structure of human being and with age bone becomes less dense and more fragile. Composition and properties of cartilage also change with age. Water content in the cartilage is less with age. When degeneration of cartilage takes place OA develop. Most people develop OA by the time they reach 70 years. However, OA does not restricted to old people; young adults can also suffer from OA like morning stiffness, aching pain, tender joints, and decrease range of motion.
Gender: Women are more prone to pain and disability than men and a hospital-based study showed rates of OA is as high as 68% in women and then 58% in men of aged 65 and above.
Genetic factor: Genetic factor may have important role in development of OA in general population. Those having identical gene, namely monozygotic teens (MZ) showed greater role of genetic factors in development of OA. Osteocalcin, a marker of bone turnover is lower in women with OA.
Physical activity / Sports: Sports like gymnastic, Kungfu (A traditional Chinese martial arts) may have risk of knee injury. Other sports activity involving more pressure on knee, hip may increase chance of OA in knee or hip joints.
Secondary Causes of OA: Here Secondary causes have same pathology like primary O.A. (i) Obesity (ii) Congenital disorders of joints (iii) diabetes (IV) Joint injury or ligament injury (v) Ligaments degeneration (vi) Joint infection [15].
Inherited causes:
- Alkaptonuria: A rare inherited disease where body prevents breaking down two protein building blocks amino acid tyrosine and phenylalanine.
- Ehlers-Danlos Syndrome (EDS): A rare inherited disease affecting connecting tissue.
- Hemochromatosis (Iron overload in the body), Wilson’s disease: Also a rare disease which causes too much accumulation of copper in different organs.
- Inflammatory diseases: It may be termed as chromic autoimmune diseases, e.g. Costochondritis, Rheumatoid arthritis.
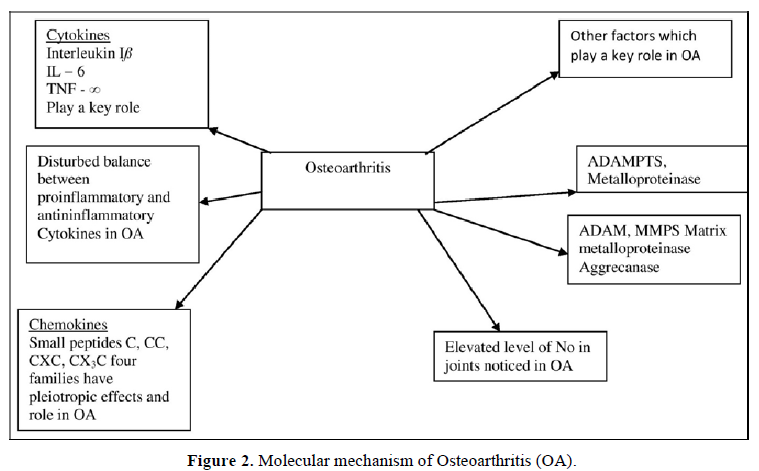
- Marfan Syndrome: A rare inherited disease due to genetic mutation results in body’s ability for building connective tissue is reduced (Figures 1 & 2).
Treatment of OA: OA can’t be reversed but treatment can reduce pain and help patients live better, improvement in quality of life.
- Acetaminophen (N-acetyl-p-aminophenol): It raises the threshold to pain stimuli and thereby exerting analgesic effect. It is considered as first line analgesic in OA. But high dose of acetaminophen can cause liver damage.
- NSAIDS (Non-Steroidal Anti-inflammatory Drugs) Over the counter (OTC) NSAIDS, such as ibuprofen and naproxen sodium (both propionic acid derivative) taken at the recommended doses typically relieve OA pain. Stronger NSAIDS are available as prescription drugs. NSAIDS have adverse effects e.g. GI Ulceration, GI bleeding, can damage hepatic and renal function also cause cardiovascular side effects. Topical application of NSAIDS to the affected area cause fewer adverse effects may also have analgesic action equally well.
Diacerein (Semi synthetic anthraquinone): it is used in osteoarthritis as anti-inflammatory, anti-arthritic drug. It also has chndroprotective action, it can reduce cartilage breakdown and also relives pain in OA. 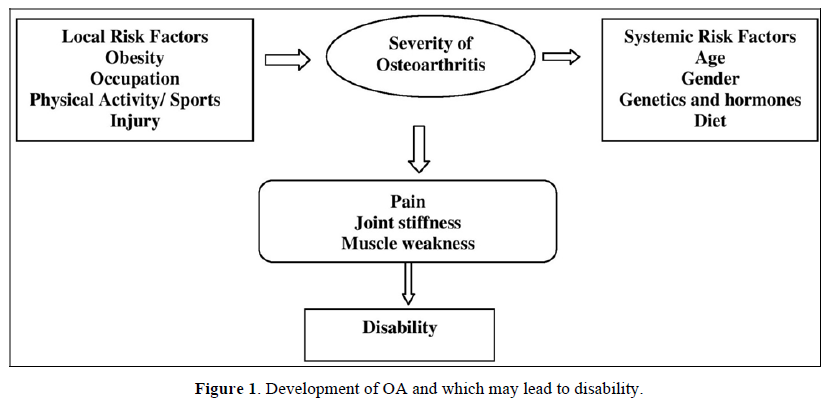
- Duloxetine (Serotonin- Norepinephrine reuptake inhibitor). It is an antidepressant used also in chronic pain in OA.
- Hydrocortisone (glucocorticoids): It is used for short term pain relief which may last for few weeks to few months.
- Alternative medicine: Glucosamine, Chondroitin. Other remedies like Avocado- Soybean unsaponifiables (ASU). Which is a dietary supplement; Phytoformulations, Ayush treatments also claim pain relief and improvement of mobility of OA patients in some cases, but large scale clinical trial data is not available.
- Sprifemin (a recombinant form of human fibroblast growth factor 18) and Strontium renelate have some action in OA whereas second one may reduce degeneration in case of OA (but EMA cautioned on its use because of adverse action).
- In some cases search for disease modifying agent in treatment of OA is going on in pre Osteoarthritis condition. Further research is needed to detect the change in that condition with biological, mechanical and imaging markers. Other strategies like gene transfer having aim to target the disease process. This will be used in place of symptomatic treatment. One version of cell medicated gene therapy is approved in South Korea.
- Knee gel injection: Another form treatment is Hyalurnate injection to knee joints, but some percentage patient do not respond to this form of treatment as their pain due to OA do not come down.
- Acupuncture and other interventions: This form of treatment gives pain relief in OA, but the effect is short term.
- Joint replacement surgery: When conservative form of treatment become ineffective in such severe cases joint replacement surgery is recommended.
CONCLUSION
In India approximately one crore people are suffering from OA. Wearing down of cartilage is the main cause. Whereas other types of arthritis are not caused by wear and tear of bones. People with an immune disorder or a chemical imbalance are in more risk of other form of arthritis. Different other types of arthritis are Rheumatoid arthritis (RA), Psoriatic arthritis, Lupus (SLE), fibromyalgia, gout, viral arthritis (Rubella, Parvovirus, Hepatitis B & C can lead to short term arthritis which is similar to RA).
Scientists of China have developed one hydro gel injection which can repair damaged cartilage. Studies on animal models like mice and pigs, the drug showed very good result. The study showed repair of torn or eroded cartilage. Scientists now learned to grow chondrocyte in formation of new cartilage; probably this may be a new discovery of OA treatment.
- Arden N, Blanco F, Cooper C, Guermazi A, Hayashi D, et al. (2015) Atlas of osteoarthritis. Springer; pp: 21. Available online at: https://www.esceo.org/sites/esceo/files/pdf/OA%20ESCEO%20Atlas%20of%20Osteoarthritis%202nd%20Edition%202018.pdf
- Osteoarthritis (2015) National Institute of Arthritis and Musculoskeletal and Shin Disease. Accessed on: May 18, 2015.
- Glyn-Jones S, Polymer AJ, Agricola R, Price AJ, Vincent TL, et al. (2015) Osteoarthritis. Lancet 386(9991): 376-387.
- Swedish Council on Health Technology Assessment (SBU) (2016) Occupational Exposures and osteoarthritis; A systemic review and assessment of medical, social and ethical aspects.
- Berenbaum F (2013) Osteoarthritis as an inflammatory (osteoarthritis is not osteoarthrosis). Osteoarthritis Cartilage. 21(1): 16-21.
- Conaghan P (2014) Osteoarthritis-care and management in adults. Available online at: http://www.nice.org.uk/guidance/cg177/evidence/full-guideline-191761309
- Brandt KD, Dieppe P, Radin E (2009) Etiopathogenesis of Osteoarthritis. Med Clin North Am 93(1): 1-24.
- March L, Smith EU, Hox DG, Cross MJ, Sanchoz-Riera, et al. (2014) Burden of disability due to musculoskeletal (MSK) disorders. Best Pract Res Clin Rheumatol 28(3): 353-366.
- GBD 2015 Disease and Injury incidence and prevalence collaborators (2016) Global, regional and national incidence prevalence and years lived with disability for 310 diseases and injuries, 1990-2015: A systemic analysis for Global Burden of Disease study 2015 Lancet 388(10053): 1545-1602.
- Sinus K (2012) Osteoarthritis: Diagnosis and treatment. Am Fam Physician 85(1): 49-56.
- Linn S, Murtaugh B, Casey E (2012) Role of Sex hormones in the development of osteoarthritis. PM R 4(5 suppl): S169-S173.
- Opentsax CNS (2016) Available online at: http://cnx.org/contains/14fb4ad7-39a/4eee-ab6e-3ef248e3e22@7.30:59/synovial-joints
- Sanchez-Adams J, Leddy HA, Mc Nulty AL, O’conor CJ, Guilak F (2014) The Mechanobiology of articular cartilage: bearing the burden of osteoarthritis. Curr Rheumatol Rep 16(10): 451.
- Maroudas A (1976) Balance between swelling pressure and collagen tension in normal and degenerate cartilage. Nature 260(5554): 808-809.
- King KB, Rosenthal AK (2015) The adverse effects of diabetes on osteoarthritis: update on clinical evidence and molecular mechanism. Osteoarthritis Cartilage 23(6): 841-850.
- Mc Alindon TE, Bannurn RR, Sullivan MC, Arden NK, Berenbaum F, et al. (2014) OARSI guidelines for the nonsurgical management of Knee Osteoarthritis. Osteoarthritis Cartilage 22(3): 363-388.
- Tanamas SK, Wijethilake P, Wluke AE, Davies-Tuck ML, Urquhart DM, et al. (2011) Sex hormones and structures changes in osteoarthritis: A systemic review. Maturitas 69(2): 141-156.




