3368
Views & Citations2368
Likes & Shares
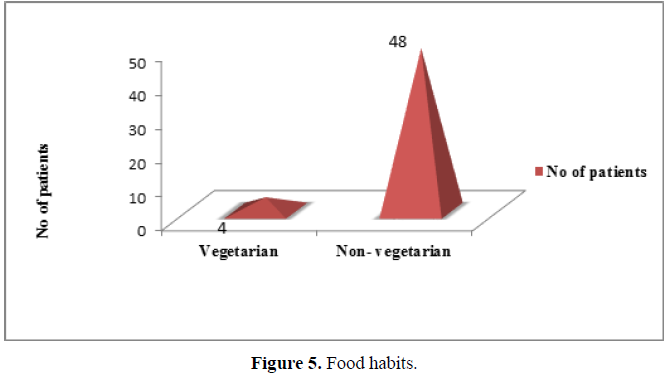
Food habits: Non-vegetarians were significantly higher (92.30%) in number than vegetarians (Figure 5).(χ2 =37.231,df=1,p<0.001).
Personal habits: Significantly higher numbers of patients (13 patients = 25%) in the sample had a habit of tobacco smoking when compared to alcohol consumption (11.50%), and only 3.80% chew pan masala (Figure 8). (χ2 =22.870,df=4,p<0.01).
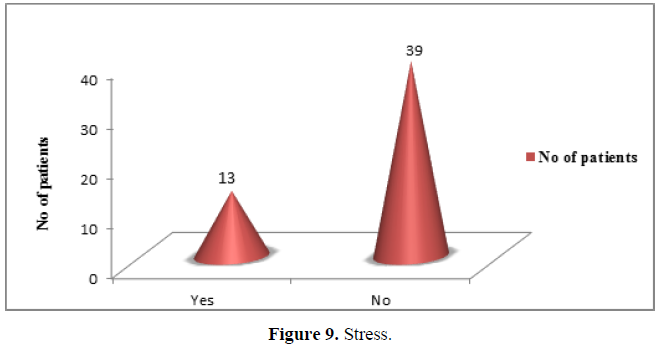
Stress: Stress was not experienced by significantly higher number of patients. Only 13 patients (25%) reported with stress out of the 52 samples of patient (Figure 9). (χ2 =13.000,df=1,p<0.01).
Investigations
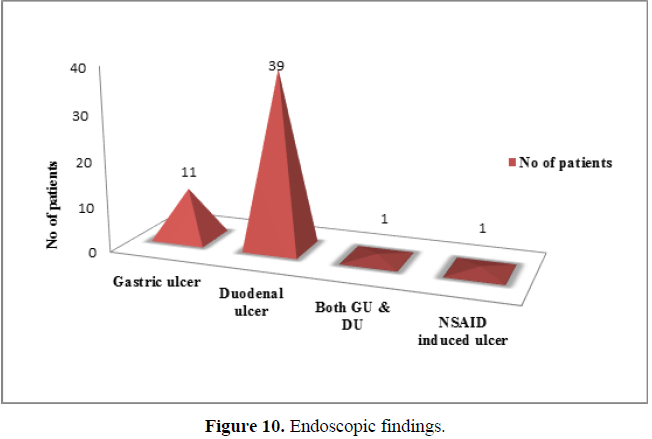
Out of all the 52 patients selected for the study, 39 patients (75%) were significantly diagnosed with duodenal ulcer, 11 (21.16%) with gastric ulcer, 1 (1.92%) with duodenal ulcer as well as gastric ulcer and another 1 patient (1.92%) with NSAID induced ulcer (Figure 10). (χ2 =74.462,df=3,p<0.001).
RUT: No significant difference in the number of patients with positive and negative RUT could be detected from the sample observation (Figure 11).(χ2 =1.231,df=1 ,p<0.05).
Treatment
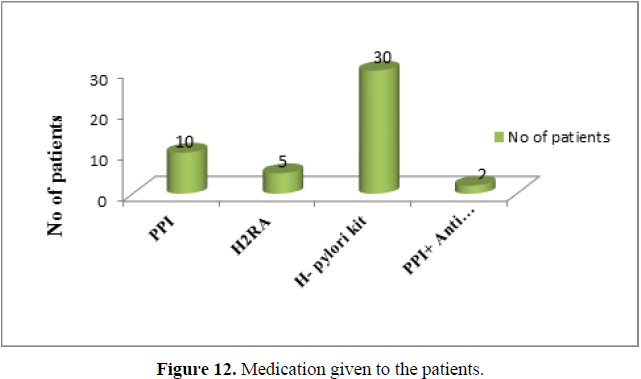
The results of medication given to the patients are shown in figure 19. Out of 52 patients, 30 patients (57.60%) were treated with H. pylori kit, 20 patients (38.50%) were prescribed with Proton pump inhibitors (PPI), 5 patients (9.60%) with histamine receptor antagonist and 2 (3.85%) patients treated with a combination of PPI and anti-emetic. Among different medications, significantly higher number of patients received H. pylori kit.(χ2 =36.263,df=3,p<0.001) (Figure 12).
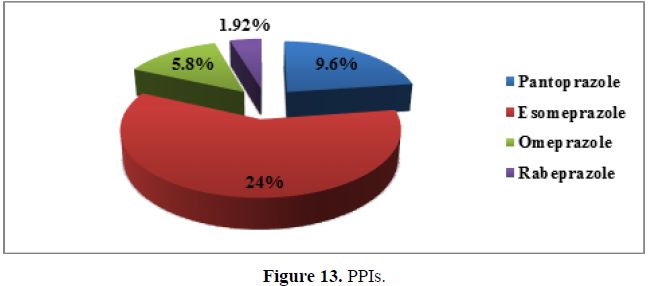
Out of all PPIs, significantly higher number (13 patients) of patients in the sample were given esomeprazole (25%), 5 patients (9.60%) treated with pantoprazole and 3 patients (5.80%) were provided with omeprazole. Only one patient (1.92%) received rabeprazole for treating peptic ulcer (Figure 13).(χ2 =19.964,df=3 ,p<0.001).
Follow up
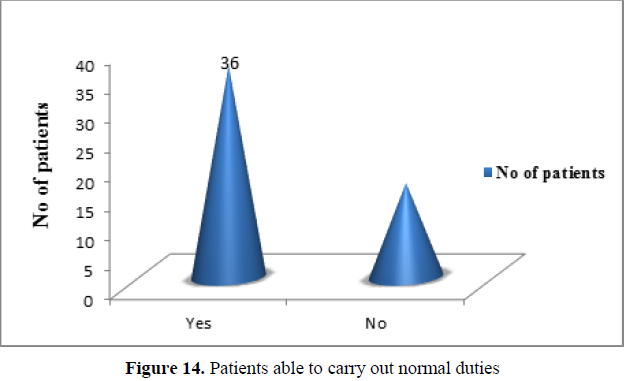
Able to carry normal duties: Significantly higher number of patients were able to perform normal duties after initial treatment (69.24%) (Figure 14).(χ2 =7.692,df=1 ,p<0.01).
Only 16 patients (30.76%) found difficulty in carrying out their normal duties even after initial course of therapy due to new or existing symptoms of peptic ulcer. (χ2 =7.692,df=1 ,p<0.01).
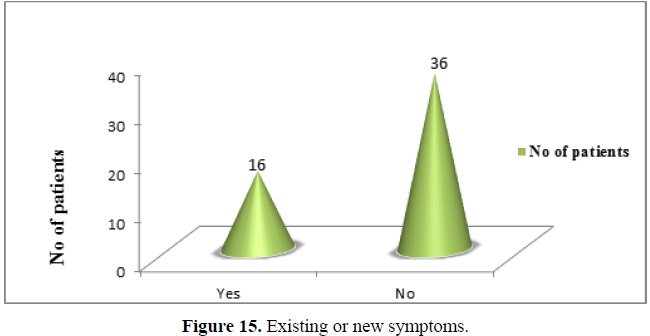
Existing or new symptoms: Significantly higher number of patients (36 patients = 69.24%) has no new/existing symptoms. Only 16 patients (30.76%) out of total 52 patients, shown new / existing symptoms of peptic ulcer (Figure 15).(χ2 =7.692,df=1,p<0.01).
Follow up treatment: There was no statistically significant difference exists between the number of patients who received maintenance therapy and new PPI treatment (Figure 16).(χ2 =0.040,df=1 ,p>0.05).
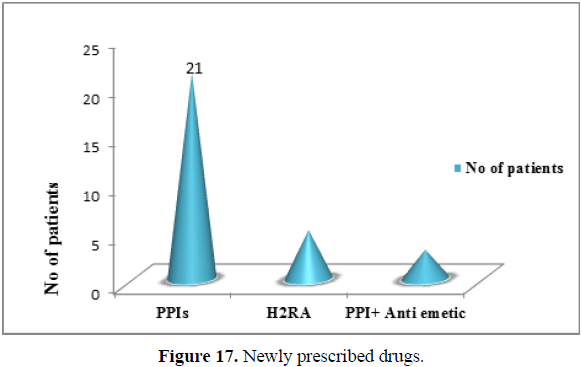
Newly prescribed drugs: During follow up, significantly large numbers of patients were prescribed with PPI’s compare to other class of drug. 21 patients (40.38%) were received new dose of PPIs, 5 patients (9.60%) treated with H2RAs and 3 patients (5.80%) with combination of PPIs and Anti emetics (Figure 17).(χ2 =20.069,df=2,p<0.001).
DISCUSSION
This current study evaluated the prevalence of peptic ulcer among those patients undergone UGI endoscopic examination. Out of a total of 388 endoscopy patients, 52 cases were peptic ulcer. The study indicates that DU was more prevalent in our region. Thus, the total prevalence of PUD in endoscoped patients was 13.4%. This study is comparable with an endoscopic series study involving 1022 volunteers from Shanghai, China (average age 48 years). In their study the prevalence of PUD was found to be 17.2%, of whom 93% were infected with H. pylori [4].
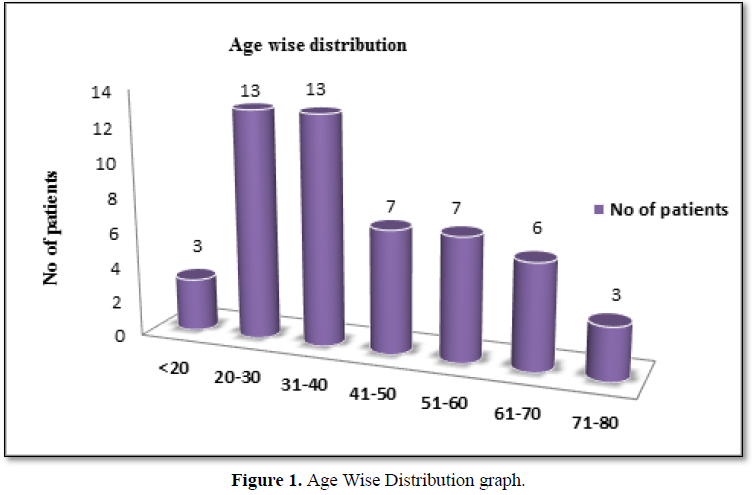
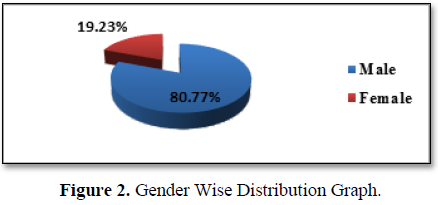
In this present study the demographic characteristics showed that 50% of the peptic ulcer patients belong to the age group 21 – 40 years, 26.9% belongs to the age group 41 – 60 years, 11.5 % coming under age group 61 – 70 years and 3% each under less than 20 years and 71 – 80 year age groups respectively, with mean age of 41.45 and SD of 16.54 (mean age Mean ± SD = 41.65 ± 16.54). This result is exactly similar to the study conducted by Jonathan O. Kadiri et al, in Nigeria [5]. This study also reveals that PUD was more prevalent among males (80.77%) than females (19.23%). A study conducted by Dr. Rafi Abul Hasanath Siddique in Dhaka medical hospital, Bangladesh, has similar result [2]. Incontrast, this is different from what some researcher got as their male to female ratio. A study conducted by Jonathan O. Kadiri et al, showed that females suffer more from PUD than males [5]. Peptic ulcer disease is a worldwide common disease, but the incidence of peptic ulcer disease in different countries and regions are obviously different. This may be the reason for variation in the ratio.
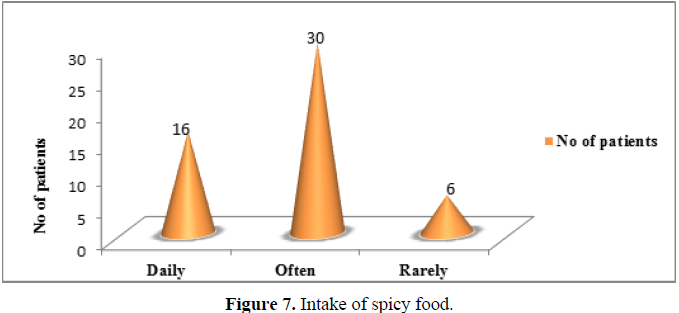
When we look at the co-morbidities, we found that more than half of the patients with PUD had an associated co-morbidity for which they would require treatment. 25% of the total respondents had hypertension and 19.23% with diabetes mellitus as co-morbid condition. According to a nationwide population-based cohort study conducted in Taiwan, diabetic patients have a higher incidence of peptic ulcer disease. Age, chronic renal disease, history of PUD, and use of NSAIDs were risk factors for PUD in diabetic patients [6]. Certain life style factors such as consumption of tobacco, alcohol, tea, coffee and spicy foods are believed to stimulate gastric acid secretion.
According to a study conducted in Hawaii, the risk of both gastric and duodenal ulcers progressively increased with increased use of cigarette smoking [2]. In this study 25% of the participant was having a habit of smoking and found that alcohol consumption was less (11.50%) among them when compared to smoking. Other important cause for PUD is usage of NSAID’s, but information regarding the history of NSAID usage was not obtainable from the medical records. Only 1 patient (1.92%) presented with the history of NSAID consumption and related ulcer incident in the OPD during this 6 month period. The current study revealed that only smoking independently predict the development of PUD. A Japanese study of men aged 45 years and older revealed that current smokers were at higher risk of both gastric (OR, 3.4, 95% CI: 2.4- 4.7) and duodenal ulcers (OR, 3.0, 95% CI: 1.9- 4.7), compared with nonsmokers. However, another study failed to confirm these findings for PUD risk in smokers compared with nonsmokers. Recent studies have suggested that tobacco smoking causes peptic ulcer only if H. pylori infection is present. A prospective cohort study in Denmark and another prospective study conducted by Fu-Wei Wang et al among general Taiwanese population showed that tobacco smoking remained an independent risk factor for PUD [7]. Hence, we believe that ulcer patients should be advised to cease smoking. Majority participants were free of stress (75%), only 25% had stress (psychological stress) which may lead to stress ulcer and it is not significant in nature.
Significantly higher number of patients suffers from duodenal ulcer in the sample. No statistically significant difference in the number of patients with positive and negative RUT could be detected from the sample observation. Even though the number of peptic ulcer patients with positive RUT test were higher (57.70%) than RUT negative cases (42.30%). Which indicates that majority of the patients were H. pylori infected.
Thus, this study concluded that the main risk factor of PUD were H. pylori infection and tobacco smoking. These findings have resemblance with the result obtained from a study conducted by S. Rosenstock et al, for identifying the risk factor for PUD among 2416 Danish adults [8].
In this study, while considering pharmacological therapy the most frequent anti-ulcer drugs prescribed as monotherapy and combination therapy belong to the class of PPIs (42.35%) and are no doubt effective agents, while H2RAs (9.60%) were the less frequently used anti-ulcer drugs as mono therapy as well as in combination therapy. This result was consistent with the study report of Jonathan O. Kadiri et al, in which they reported that PPIs were the most widely prescribed category of peptic ulcer medication [5]. This study was in contrast with a cross sectional retrospective study conducted by Ahmed Almeman et al., [9] which preferred H2RAs as anti-ulcer drugs. Although H2RAs are having a definite advantage over PPIs from the economic point of view, but physician choosing it only for treating very few patients. The PPIs are more superior to the H2RAs and thus in our study PPIs were more preferred than H2RAs. Gastric acid suppressant therapy in the form of an H2 blocker or proton pump inhibitor for four weeks induces healing in most duodenal ulcers. Majority of guidelines and reviews recommend PPI as first line for eradication therapy in PUD [9]. A systematic review of randomized controlled trials by Vakil N et al, showed that proton pump inhibitors healed duodenal ulcers in more than 95 % of patients at four weeks and gastric ulcers in 80 to 90 percent of patients at eight weeks [10].
Even though Omeprazole is the traditional and more available cheaper PPI when compared to Esomeprazole, but in this study the physician chooses Esomeprazole due to its greater efficiency.
It was observed that most PUD patients with peptic H. pylori infection were started on a fixed combination of H. pylori kit. In this present study also Esomeprazole based HP kit was more commonly prescribed eradication regimen. In a meta-analysis conducted by McNichollet al, it was found that Esomeprazole was more efficacious in the eradication of H. pylori infection than the first generation proton pump inhibitors. This result was also consistent with the study conducted by Veeksha Jayaram et al., [1].
CONCLUSION
This is the first observational study performed in our setting about Peptic ulcer disease; therefore, no previous results available from the public and/or private hospitals related to this study for comparison. From this study it is evident that the duodenal ulcer was more prevalent among the study population when compared to gastric ulcer. This study identified that the predominant reason for the development of peptic ulcer was H. Pylori infection followed by smoking.
One of the major factors identified from this study is that majority of the patients and care givers were unaware about the role of H. pylori and smoking in the development of peptic ulcer disease. Thus, there is an evident need for making the patient and their care givers aware about their disease more clearly. In order to overcome this problem, we designed a clear, brief patient information leaflets and distributed among ulcer patients.
A detailed analysis of pharmacological agents used in PUD showed that PPIs were the most preferred drugs by physicians and among PPIs, esomeprazole was the predominant one. The treatment strategy practiced in India is primarily to start an empirical treatment for Helicobacter pylori eradication. But in our institution RUT test were performed in all patients along with endoscopy and choice of drug therapy is finalized based on RUT result. Need of conducting RUT test for all ulcer patients are questionable. It has added an extra unnecessary economic burden over the patients.
The current guidelines strongly recommend eradication therapy for H. pylori in all patients with duodenal or gastric ulcers, which will result in cure for over 90% of these patients, so that treatment is cost-effective as well as clinically beneficial. Eradication also decreases the need for continued treatment and PUD recurrence. A comparison between H2RAs and PPIs and making a choice between them are quite difficult task. The inclusion of proton pump inhibitors with appropriate antibiotics has proven to maintain high eradication rates. Shorter courses of therapy with fixed combinations of H. pylori kits can improve compliance and decrease treatment failures. However the implication of such widespread use of antibiotics on antibiotic resistance needs to be borne in mind.
CONFLICTS OF INTEREST
The authors have none to declare.
FUNDING SOURCE
Funding for the research project was provided by Al shifa college of pharmacy, Shifa institute of medical sciences, Shifa medicare trust, Perinthalmanna, Kerala.
ACKNOWLEDGEMENTS
We acknowledge the valuable comments and suggestions by Dr, Saju Xavier during this project. The authors would like to thank the staff, Department of Gastroenterology, Al shifa hospital, and Department of Pharmacy Practice, Al Shifa College of pharmacy for supporting this work.
- Siddique RAH (2014) Prevalence of peptic ulcer disease among the patients with abdominal pain attending the department of medicine in dhaka medical college hospital, Bangladesh. IOSR Journal of Dental and Medical Sciences 13(1): 05-20.
-
Mark F, Lawrence S, Friedman, Brand LJ (2015) Sleisenger, frodtran’s gastroenterology and liver disease. Saunders Publisher, 10th edition. 2015: 884-899.
-
Kadiri JO, Wannang NN, Adeniyi MA, David S, Dangiwa DA (2015) Peptic ulcer treatment evaluation in tertiary and secondary hospitals in north central Nigeria. World J Pharm Sci 3(8): 1539-1545.
-
Ling PY, Bang LH, Chyuan LJ, Chou HC, Chih HM, et al, (2013) Diabetes is an independent risk factor for peptic ulcer bleeding. Journal of Gastroenterology and Hepatology 28(8): 1295-1299.
-
Wang FW, Tu MS, Mar GY, Chuang HY, Yu HC, et al, (2011) Lung-Chih Cheng, Ping-I Hsu. Prevalence and risk factors of asymptomatic peptic ulcer disease in Taiwan. World J Gastroenterol 17(9): 1199-1203.
-
Rosenstock S, Jorgensen T, Bonnevie O, Andersen L (2003) Risk factors for peptic ulcer disease: A population based prospective cohort study comprising 2416 Danish adults. Gut 52: 186–193.
-
Ahmad A, Saleh AA, Seemab R (2013) Prescribing practices and cost of drugs for peptic ulcer in a primary health center in pulau penang, Malaysia. Tropical Journal of Pharmaceutical Research 12(4): 629-634.
-
Vakil N, Fennerty MB (2003) Direct comparative trials of the efficacy of proton pump inhibitors in the management of gastroesophageal reflux disease and peptic ulcer disease. Aliment Pharmacol Ther 18(6): 559-568