2032
Views & Citations1032
Likes & Shares
The first successful kidney
transplantation was performed between twins in 1954. That established kidney
transplant as a key step in the treatment of end-stage kidney disease to
improve the quality of life and prolong the life of patients who are fit for
this procedure. However, the timely recognition, precise diagnosis, and
well-timed treatment of post-operative complications are crucial in the successful
management of these patients. A delay in the diagnosis or management of these
complications can result in significant morbidity to the recipient leading to
graft loss and mortality in spite of significant advances. Careful preoperative
evaluation, proactive pre-emptive approach and careful postoperative monitoring
are critical at all the stages of the transplant process: (a) donor
nephrectomy, (b) bench work preparation, and (c) implantation of the allograft.
Renal transplant recipients should be managed in specialised units to guarantee
optimal graft survival and graft function.
Keywords: Kidney
transplantation, Urinary complications, Lymphocele, Vesicoureteral reflux,
Morbidity, Investigations, Complications, Diagnosis
INTRODUCTION
Post-renal transplant complications can be due to either surgical or
medical issues. In some patients, it may be due to both. Safe and effective
management of kidney transplant recipients commences with scrupulous
pre-operative assessment and correction of risk factors. Meticulous surgical
practice, strict sterile procedure and haemostasis are crucial. Nephrologists
should be aware of the medical as well as surgical complications and be skilled
in the prompt diagnosis of medical and surgical complications.
Early post-kidney
transplant surgical complications
Surgical complications after kidney transplantation are categorized as
vascular (arterial and venous thrombosis, transplant renal arterial stenosis,
lymphocele, hemorrhage, graft’s rupture, hematoma) and urologic (ureteral
obstruction, vesicoureteral reflux, urinary fistula) (Table1).
Urologic problems are the dominant surgical complication subsequently to
kidney transplantation, triggering substantial morbidity and mortality. The
prevalence of urologic problems after renal transplantation has reduced to 2.5%
from 12.5%. The common urological problems post kidney transplantation
incriminates the ureterovesical anastomosis (reflux, fistula and stenosis).
Medical problems in
post kidney transplantation
·
Delayed graft
function (DGF)
·
Acute transplant
graft rejection
·
Acute tubular
necrosis
·
Coagulation
syndromes
·
Infections due
to various causes
Vascular, urinary,
lymphocele and post-operative bleeding are surgical complications which are
carefully watched in the early course of the post-operative period in kidney
transplantation.
Timely radiological
assessments would go a long way in spotting vascular and urological
complications. Prompt investigations and evaluations will help to reduce
delayed graft function. Early radiological assessments are enlightened in Table 2.
Mild hydronephrosis and
dilatation of the transplant collecting system on ultrasonography may be seen
without the presence of an actual urinary obstruction. There is a need to have
a close watch on worsening hydronephrosis that is pathological.
After kidney transplantation,
there could be vascular [1-5] or urologic [6,7] complications. Surgical
problems have an occurrence of 5-10% and continue to be an important source of
graft loss. They usually present early after transplantation.
VASCULAR COMPLICATIONS
Renal vein thrombosis
Renal vein thrombosis happens in
the first postoperative week in 0.3%-6.1% of kidney recipients [8]. Abruptly
loss of urine output, the presence of blood in the urine and ache in the graft
site are observed. Potential threats are the technique of transplantation
surgery, hyper coagulopathy, and severe volume depletion and right donor
kidney, compression of the renal vein by a localised collection of blood or
collection of lymphatic fluid. With short right renal vein, venous thrombosis
is an added risk [9].
Renal artery stenosis
In less than 1% of renal
transplant recipient’s arterial thrombosis (TRAS) may be a cause of graft loss
[8,10] though has been reported as high as 23% [11,12]. It can present as
worsening renal function, flash pulmonary edema and the rapid start of uncontrollable
blood pressure [13]. Several recipients show no symptoms with transplant renal
artery stenosis (TRAS). Using regular duplex assessment (grey scale as well as
Doppler), TRAS is seen in 2.4% of symptomatic and 12.4% in asymptomatic
recipients [14]. TRAS most frequently happens in the anastomotic area at 3 to
24 months, though it may occur in the post or pre-anastomotic sites as well. In
patients with end-to-end anastomosis, TRAS is more likely to happen.
Urological problems cause
noteworthy graft injury and death. The incidence of urologic complications
varies from 2.5% to 30% [15-20]. Among them, the ureteral leakage
manifestations may be minor or major. Usually, a substantial decrease in output
happens with an increase in drainage. The incidence of urine leakage identified
about 1% and 4.3%. The frequency of lymphatic fluid collection ranges from 0.6%
to 18.1%. After introducing check ultrasonograms for regular inspection of the
renal graft, the pickup rate may be excessive around 50%. Blood clots can be
spotted and cured swiftly [21].
Differential diagnosis of
post-kidney transplant fluid collection in this given scenario:
•
Hematoma/Bleeding
•
Lymphocele
•
Peri-renal
abscesses
•
Urinoma due to
urine leak
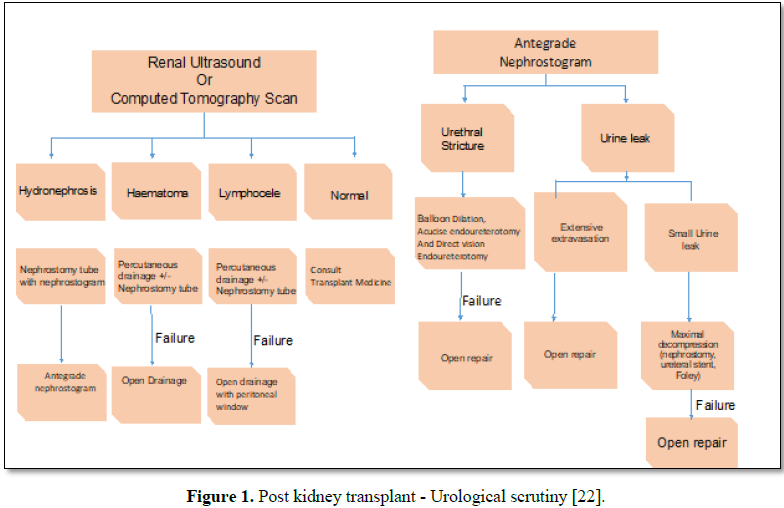
Work-up and dealing with acute transplant
kidney injury post-transplantation and transplant ureteral dilemmas are shown
in Figure 1.
Hematoma/hemorrhage
Hematoma presents as bloodstained
leakage of blood associated with tachycardia, hypotension and drop in
hemoglobin. Sometimes clots may block the drain. The urgent scan is vital and
may be followed by immediate re-exploration if there is any doubt.
Lymphocele
Even large lymphocele could be
asymptomatic if it is far from hilum and is not squeezing the ureter. Reduced
urine output and DGF can be caused by lymphocele if ureter is blocked.
Intervention is not indicated if there is no graft dysfunction and no
hydronephrosis [23,24]. Biochemical studies can aid in diagnosis. Elevated
creatinine and potassium values in drained or aspirated fluid would give an
answer.
Perinephric abscesses
Gram stain and culture and
sensitivity should be sent to the lab to discover the organisms as abscesses
may be a complication of hematoma, urinoma and lymphocele.
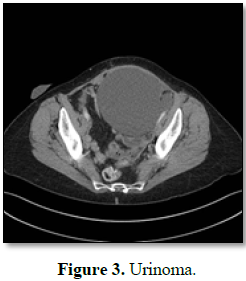
Urinoma
With the use of the double-J
ureteric stent, urine leak is less common. Urine leak may be instant or late.
It can present as increased drainage, DGF or leaking from the wound.
CASE SCENARIO
Recipient age: 28 years, CKD
stage 5, Pre-emptive kidney transplantation
Donor: Brother
Post-operative drainage: Day
2:820 ml and Day 3:750 ml. Subsequent Table
3 shows the laboratory values of fluid and serum.
Biochemical studies of fluid and serum together can
assist in diagnosis. High creatinine and potassium levels in the drained or
aspirated fluid indicate urinoma. Therefore, this patient has a urine leak.
Biochemical analysis of the drainage fluid will display high creatinine and
potassium levels on drainage or removed fluid equated with a simultaneous
serum. If the drained fluid biochemistry is similar to serum sample, it means
that the liquid is either seroma or lymphocele.
METHODOLOGY TO DIAGNOSE AND RESOLVE THE PROBLEMS
Urologic complications are
common in post kidney transplantation, equated with vascular difficulties.
Maximum urologic issues happen in the first two weeks. Anastomotic leaks are
common [25]. Leaks are occurring instantly typically due to technical problems
[24]. After one week, it may be caused by ureteral necrosis. Catheter blocks
must be excluded [20,26]. Suture dehiscence, caliceal leak, ureteric kinking,
ureteric ischemia and bladder perforation are to be considered [27,28]. If a
polar artery is tied off, it may cause a localized infarction. This may lead to
a caliceal leak [29].
DISTINCTIVE FEATURES
Disproportionate drain fluid
(volume and biochemistry) throughout the initial postoperative days reduced
urine through the catheter, impaired graft function and pain over the graft are
scrutinised. The timing of the removal of the double-J stent may give a clue to
urine leakage [30,31]. It could present with an insidious start. Urinoma is
typically anechoic, lacking septations and happening in less than two weeks of
post kidney transplantation surgery. Table
4 assesses the clinical issues and management specificities according to
the mechanism of urine leak.
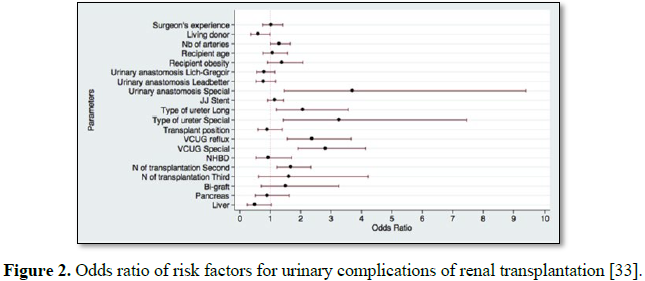
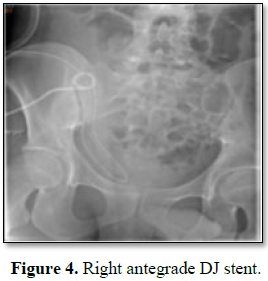
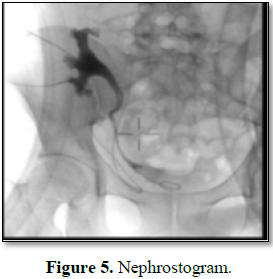
Few radiological investigations and managements like CT
scan, antegrade DJ stent insertion and nephrostogram are shown in Figures 2-5.
Avoidance of post-operative
complications:
1. Ureteric
ischemia is avoided by unnecessary dissection around donor ureter
2. Shorter
ureter usage lessens ureteric ischemia.
3. Routine
usage of the ureteric stent at the time of ureterovesical anastomosis is
recommended though there is an association with a higher possibility of urinary
tract infections in transplanted kidneys [34].
Conservative approach is
justifiable if there is no hydronephrosis. If the patient did not have a double
J stent, retrograde insertion of the stent is never an option in postoperative
transplant period.
PERCUTANEOUS MANAGEMENT
When there is a small leak with
hydronephrosis, ureteral fistula can be treated with percutaneous nephrostomy.
If there is a delay in surgery for managing more significant leaks, the
collections should be drained to reduce the risk of infection [24,35-37].
Complete decompression with percutaneous nephrostomy and double J stent
placement is crucial. Surgical exploration is indicated when conservative
management fails.
Main urinary complications and surgical management
Ureteric leak: At the time of re-implantation, one must make sure
that ureter is well perfused. If there is not enough length of a well-perfused
transplanted ureter, then the native ureter rather than the urinary bladder is
used for anastomosis. By using the ipsilateral native ureter, ureteropyelostomy
is the right decision. Cystopyelostomy repairs necrotic ureter [38-42].
Bladder leak: In meaningful leaks, bladder-mending surgery is
suggested. This should be followed by extended bladder drainage, a minimum of
two weeks.
Calyceal leak: Calyceal leakage can be caused by segmental
transplanted graft infarction by ligature of a polar artery. If conservative
action does not work, then partial nephrectomy can be used earlier to rescue
the allograft in a rather rare situation. The location of the leak and the
grade should be evaluated at the earliest.
Vesicoureteral reflux: Vesicoureteral reflux after kidney
transplantation is not very uncommon. The occurrence may be as high as 50%-86% [22,43].
This may be due to surgical practice. To lessen the risk of ureteral stricture
several surgeons support a patulous ureteroneocystostomy procedure rather than
a tunneled implantation of the ureter. Open reconstruction desirable for
high-grade VUR.
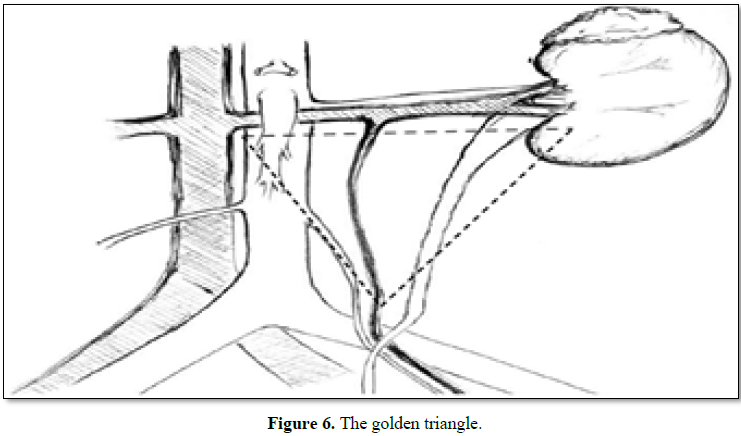
Surgical procedures [44]
Urological complications range
from 5-10%. Unlike native ureters that derive their blood supply from renal
arteries, aorta, iliac arteries and vesicle arteries, the transplanted ureter
depends solely on the blood supplied by the branches of the renal artery that
traverse through peri-ureteric tissues. To preserve transplant ureter’s blood
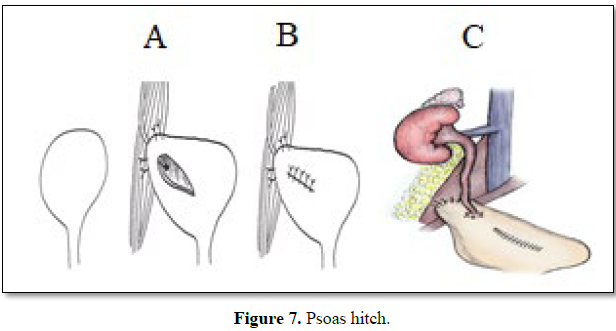
supply, one must be careful to protect the “golden triangle” (Figure 6). Hitching of a mobilised
bladder (Figure 7) and Boari flap (Figure 8) are surgical procedures. Use
of ileum as a neo-ureter, in the absence of native ureter, is an option in rare
instances (past two-sided nephroureterectomy). A small anastomotic leak can be
cured with resection and re-implantation of distal ureter.
CONCLUSION
Urine leak, ureteric necrosis,
VUR and obstruction are common urological hurdles. Post-transplant urine leak
management is vital. Biochemical scrutiny of emptied fluid is the necessary
choice of investigation and must be matched with the sample of serum.
Historically these difficulties have been handled by extensive restoration. Now
conservative action or by percutaneous drainage ought to be pondered as the
first choice of treatment in recipients with minor urine leaks. But in the
absence of any response to conservative action or if the leak is ominously
huge, then surgical exploration must be executed. Surgical handling varies on
leak cause, anastomosis style, and perfusion of the ureter. Innovations in
endourological techniques with modern-day types of equipment have been
acceptable in numerous kidney recipients and done with caution.
1.
Expert Panel on Urologic Imaging, Taffel MT, Nikolaidis
P, Beland MD, Blaufox MD, et al. (2017)
ACR
appropriateness criteria: Renal transplant dysfunction. J Am Coll Radiol 14: S272-S281.
2.
Osman Y, Shokeir A, Ali-el-Din B, Tantawy M, Wafa EW, et al. (2003)
Vascular
complications after live donor renal transplantation: study of risk factors and
effects on graft and patient survival. J Urol 169: 859-862.
3.
Englesbe MJ, Punch JD, Armstrong DR, Arenas JD, Sung RS, et al. (2004) Single-center
study of technical graft
loss
in 714 consecutive renal transplants. Transplantation 78: 623-626.
4.
Fervenza FC, Lafayette RA, Alfrey EJ, Petersen J (1998) Renal artery stenosis in kidney transplants. Am J Kidney
Dis 31: 142-148.
5.
Odland MD
(1998) Surgical technique/post-transplant surgical complications. Surg Clin North Am 78: 55-60.
6.
Streeter EH, Little DM, Cranston DW, Morris PJ (2002) The urological
complications of renal transplantation: A series of 1535 patients. BJU Int 90: 627-634.
7.
Kocak T, Nane I, Ander H, Ziylan O, Oktar T, et al. (2004) Urological and surgical complications in 362 consecutive living
related donor kidney transplantations. Urol Int 72: 252-256.
8.
Obed A, Uihlein DC, Zorger N, Farkas S, Scherer MN, et al. (2008) Severe renal vein
stenosis of a kidney transplant with beneficial clinical course after successful percutaneous stenting. Am
J Transplant 8: 2173-2176.
9.
Takahashi M, Humke U, Girndt M, Kramann B, Uder M (2003) Early posttransplantation renal allograft perfusion failure due to
dissection: Diagnosis and interventional treatment. AJR Am J Roentgenol 180: 759-763.
10.
Melamed ML, Kim HS, Jaar BG,
Molmenti E, Atta MG, et al.
(2005) Combined percutaneous mechanical and chemical thrombectomy for renal vein thrombosis in kidney transplant recipients. Am J Transplant 5: 621-626.
11.
Osman Y, Shokeir A, Ali el Dein B, et al. Tantawy M, Wafa EW (2003) Vascular complications after live donor renal transplantation:
study of risk factors and effects on graft and patient survival. J Urol 169:
859-862.
12.
Patel NH, Jindal RM, Wilkin T, Rose S, Johnson MS, et al. (2001) Renal arterial stenosis
in renal allografts: retrospective study of predisposing factors and outcome
after percutaneous transluminal angioplasty. Radiology 219: 663-667.
13.
Garovic VD, Textor SC (2005) Renovascular hypertension and ischemic nephropathy. Circulation 112: 1362-1374.
14.
Wong W, Fynn SP, Higgings RM, Walters H, Evans S, et al. (1996) Transplant renal artery stenosis in 77 patients: Does
it have an immunological cause? Transplantation 61: 215-219.
15.
Slagt IK, Ijzermans JN, Visser LJ, Weimar W, Roodnat JI, et al. (2014)
Independent risk factors for
urological complications after deceased donor kidney transplantation. PLoS One 9: e91211.
16.
Dalgic A, Boyvat F, Karakayali H, Moray G, Emiroglu R, et al.
(2006) Urologic complications in 1523 renal transplantations: The Baskent
University experience. Transplant Proc 38: 543-547.
17.
Moray G, Yagmurdur MC, Sevmis S, Ayvaz I, Haberal M (2005) Effect of routine
insertion of a double-J stent after living related renal transplantation.
Transplant Proc 37: 1052-1053.
18.
Ali-Asgari M, Dadkhah F, Ghadian A, Nourbala MH (2013) Impact of ureteral length on urological
complications and patient survival after kidney transplantation. Nephrourol Mon 5: 878-883.
19.
Kumar S, Ameli-Renani S, Hakim A, Jeon JH, Shrivastava S,
et al. (2014) Ureteral
obstruction following renal transplantation: Causes, diagnosis and management.
Br J Radiol 87: 20140169.
20.
Dinckan A, Tekin A, Turkyilmaz S, Kocak H, Gurkan A, et al. (2007) Early and late urological complications corrected surgically
following renal transplantation. Transpl Int 20: 702-707.
21.
Zhao J, Gao Z, Wang
K
(2011) The transplantation operation and its surgical complications. Understanding
the Complexities of Kidney Transplantation. ISBN: 978-953-307-819-9.
22.
Duty BD, Barry
JM (2015) Diagnosis and management of ureteral complications following renal transplantation. Asian J Urol 2: 202-207.
23.
Singer J, Gritsch HA, Rosenthal JT (2005) The transplant operation and its surgical
complications. Danovitch GM, ed. Handbook of Kidney Transplantation. 5th Edn. Philadelphia, PA, Lippincott Williams &
Wilkins, pp: 193-212.
24.
Mah TJ, Mallon DH, Brewster O, Saeb-Parsy K, Butler AJ, et al. (2017) Ureteric complications in recipients of kidneys
from donation after circulatory death donors. Clin Transplant 31.
25.
Shoskes D, Jiménez JA (2013) Urological complications after kidney transplantation.
In: Morris PJ,
Knechtle SJ, eds. Kidney Transplantation: Principles and Practice. 7th Edn. Oxford, UK:
Saunders, pp: 464-471.
26.
Mahdavi-Zafarghani R, Taghavi R (2002) Urological complications following renal transplantation: Assessment
in 500 recipients. Transplant Proc 34: 2109-2110.
27.
Nie ZL, Zhang KQ, Li QS, Jin FS, Zhu FQ, et al. (2009)
Treatment
of urinary fistula after kidney
transplantation. Transplant Proc 41: 1624-1626.
28.
Wilson CH, Bhatti AA, Rix DA, Manas DM (2005) Routine intraoperative ureteric stenting for kidney transplant recipients.
Cochrane Database Syst Rev 4: CD004925.
29.
Hricko GM, Birtch AG, Bennett AH, Wilson RE (1973) Factors
responsible for urinary fistula in the
renal transplant recipient. Ann Surg 178: 609-615.
30.
Neri F, Tsivian M, Coccolini F, Bertelli R, Cavallari G, et al. (2009) Urological complications after kidney transplantation: Experience
of more than 1,000 transplantations. Transplant Proc 41: 1224-1226.
31.
Sui W, Lipsky MJ, Matulay JT, Robins DJ, Onyeji IC, et al. (2017) Timing and predictors of early urologic and
infectious complications after renal transplant: An analysis of a New York
state wide database. Exp
Clin Transplant 16: 665-670.
32.
Hamouda M, Sharma A, Halawa A (2018) Urine leak after kidney transplant: A review of the
literature. Exp Clin Transplant 1: 90-95.
33.
Bessede T,
Hammoudi Y, Bedretdinova D, Parier B, Francois H, et al. (2017) Preoperative risk factors associated with urinary
complications after kidney transplantation. Transplantation Proceedings 49: 2018-2024.
34.
Mastrosimone S, Pignata G, Maresca MC, Calconi G,
Rabassini A, et al. (1993) Clinical
significance of vesicoureteral reflux after kidney transplantation. Clin
Nephrol 40: 38e45.
35.
Duty BD, Conlin MJ, Fuchs EF, Barry JM (2013) The current role of endourologic management of
renal transplantation complications. Adv Urol 2013: 246520.
36.
Campbell SC, Streem SB, Zelch M, Hodge E, Novick AC (1993) Percutaneous management of transplant ureteral fistulas: Patient
selection and long-term results. J Urol 150: 1115-1117.
37.
Emiroğlu R, Karakayall H, Sevmiş S, Akkoç H, Bilgin N, et al.
(2001) Urologic complications in
1275 consecutive renal transplantations. Transplant Proc 33: 2016-2017.
38.
Haberal M, Boyvat F, Akdur A, Kırnap M, Özçelik Ü, et al.
(2016) Surgical complications
after kidney transplantation. Exp Clin Transplant 14: 587-595.
39.
Gallentine ML, Wright FH Jr. (2002) Ligation of the native ureter in renal
transplantation. J Urol 167: 29-30.
40.
Shokeir AA, Shamaa MA, Bakr MA, el-Diasty TA, Ghoneim MA (1993) Salvage of difficult transplant urinary fistulae
by ileal substitution of the ureter. Scand J Urol Nephrol 27: 537-540.
41.
French CG, Acott PD, Crocker JF, Bitter-Suermann H, Lawen
JG (2001) Extra vesical
ureteroneocystostomy with and without internalized ureteric stents in pediatric
renal transplantation. PediatricTransplant 5: 21-26.
42.
Gutierrez-Calzada JL, Ramos-Titos J, Gonzalez-Bonilla JA,
Garcia-Vaquero AS, Martin-Morales A, et al. (1995) Caliceal
fistula formation following renal transplantation: Management with partial
nephrectomy and ureteral replacement. J Urol 153: 612-614.
43.
Ostrowski M, Wlodarczyk Z, Wesolowski T, Gracz H, Sluzar
T, et al. (1999) Influence of
ureterovesical anastomosis technique on the incidence of vesicoureteral reflux
in renal transplant recipients. Ann Transplant 4: 54e8.
44.
Buttigieg
J,
Agius-Anasatasi A, Sharma A, Halawa
A (2018) Early urological complications after kidney transplantation: An overview.
World J Transplant 8: 142-149.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- Journal of Alcoholism Clinical Research
- International Journal of AIDS (ISSN: 2644-3023)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)