777
Views & Citations10
Likes & Shares
Introduction: In severe upper limb
injuries, which leave extensive and deep wounds with significant damage to
vascular and nervous structures and bone exposure, surgical options are often
limited. In these cases, when patients present severe vascular damage,
comorbidities or they are in a center that does not count with the conditions
for a microsurgical reconstruction; the internal mammary artery perforator flap
is a great option for coverage.
In this work we
describe the use of the Internal Mammary Artery Perforator (IMAP) flap for
coverage of a wound in the forearm in a non candidate patient for
reconstruction with microsurgical flaps.
Discussion: The internal mammary
artery perforating flap is a widely known flap in its vascular anatomy,
technically simple, safe, versatile, with a good arc of rotation and with low
morbidity.
Conclusion: Due to all the virtues that this flap offers
and its low morbidity it is an excellent option to cover not only local and
regional wounds, but also distant wounds as in the case described, interpolating
it to the upper extremities with excellent results.
Keywords: Internal mammary artery,
Flap, Perforator
INTRODUCTION
The
internal mammary artery perforator flap is a good option for these cases given
its well known anatomy, technical ease to perform, due to the size and
thickness of the tissue that can be interpolated and its low morbidity [2].
This flap is a modification of the medially based deltopectoral flap which was
described in 1965. It is a very versatile fasciocutaneous flap, of good thickness,
easily foldable, with a large arc of rotation and with low morbidity since the
donor area can be primarily closed. It is based on perforating arteries of the
internal mammary artery and its main use is described for reconstruction of the
head and neck [3,4].
Different
clinical applications exist for the IMAP flaps. The flaps based on IMAP 1 or 2
may be rotated cranially for tracheostoma or anterior neck reconstruction. The
flaps based on IMAP 4 or 5 supplying the skin of the inframammary fold could be
used for reconstruction of the contralateral thoracic wall, breast or thoracic
limb. The harvest site of IMAP 1 and 2 can be closed directly if the width of
the flap is less than 6 cm. The IMAP 4 and 5 harvest site could be closed via a
reduction mammaplasty technique, thus minimising donor-site morbidity [5].
In
this work we describe the use of this versatile flap for coverage of the
forearm in a patient who suffer an extensive
TECHNIQUE
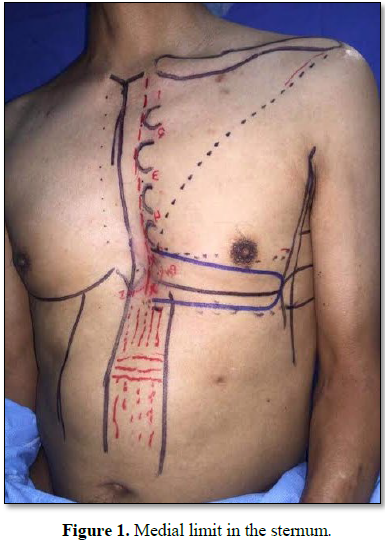
With the patient in a decubitus position, the
flap is marked at the level of the 4th or 5th intercostal
space, once de perforator was identified with the help of a Doppler, the flap
is drawn transversely. The medial limit was the sternum (midline), the length
was just at the anterior axillary line and the width was based on the coverage
required (8 cm to obtain a primarily closure of the defect) (Figure 1). The superior and inferior
incisions were first made down to the pectoralis fascia and subfascial
dissection was carried out from lateral to medial using monopolar diathermy,
until 4-5 cm from the sternal border. At this point, dissection was performed
using tenotomy scissors until the perforator vessels were identified. After
that, the flap onset in the forearm was made (Figure 2) and an on layer primarily closure of the donor defect
was done after undermining and a suction drain placement [6].
DISCUSSION
Different clinical applications exist for the
IMAP flaps. The flaps based on IMAP 1 or 2 may be rotated cranially for
tracheostoma or anterior neck reconstruction. The flaps based on IMAP 4 or 5
supplying the skin of the inframammary fold could be used for reconstruction of
the contralateral thoracic wall, breast or thoracic limb.
The internal mammary artery perforating flap
is a widely known flap in its vascular anatomy, technically simple, safe,
versatile, with a good arc of rotation and with low morbidity.
For all these features this flap is a great
option for the coverage of wounds in patients that are not candidates for
microsurgical flaps.
CONCLUSION
Due to all the virtues that this flap offers
and its low morbidity it is an excellent option to cover not only local and
regional wounds, but also distant wounds as in the case described,
interpolating it to the upper extremities with excellent results.
1.
Gillis JA, Prasad V, Morris SF
(2011) Three-dimensional analysis of the internal mammary artery perforator
flap. Plast Reconstr Surg 128: 419e.
2.
Vesely MJ, Murray DJ, Novak CB,
Gullane PJ, Neligan PC (2007) The internal mammary artery perforator flap. An
anatomical study and a case report. Ann Plast Surg 58: 156-161.
3.
Yu BT, Hsieh CH, Feng GM, Jeng
SF (2013) Clinical application of the internal mammary artery perforator flap
in head and neck reconstruction. Plast Reconstr Surg 131: 520e.
4.
Hanasono MM, Butler CE (2009)
Three- and four-dimensional arterial and venous perforasomes of the internal
mammary artery perforator flap. Plast Reconstr Surg 2009: 1770-1771.
5.
Schmidt M, Aszmann OC, Beck H,
Frey M (2010) The anatomic basis of the internal mammary artery perforator
flap: A cadaver study. J Plast Reconstr Aesthet Surg 63: 191-196.
6.
Iyer NG, Clark JR, Ashford BG
(2009) Internal mammary artery perforator flap for head and neck
reconstruction. ANZ J Surg 79: 799-803.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Pathology and Toxicology Research
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Allergy Research (ISSN:2642-326X)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)