969
Views & Citations10
Likes & Shares
There is a high incidence of pressure sore in
patients with prolonged periods of prostration, being the sacral region a very
frequent site for the appearance of these lesions.
Multiple surgical options to solve these ulcers have
been described; a myocutaneous flap using the gluteus muscles or a
fasciocutaneous flap are the most popular options.
In this work we describe the use of a double V-Y
advancement myocutaneous gluteal flap for the coverage of a chronic sacral
ulcer in a paraplegic patient.
As it has been described since 1970, this flap has
been used to cover this type of ulcers because it offers adequate tissue
quality, with good vasculature and plentiful thickness to prevent recurrences.
Keywords: Myocutaneous flap, Sacral ulcer, Gluteal flap
INTRODUCTION
Pressure ulcers continue to be a major medical-surgical problem, due to their frequency, their multidisciplinary treatment requirement and their high cost [1]. Pressure ulcers are classified according to their severity in stages I to IV (Figure 1) [2]. Stage I and II ulcers usually evolve well with conservative treatment, while those in stages III and IV require surgical treatment for healing.
The patients who most frequently suffer
ulcers from sacral pressure are those who have problems to mobilize, which
generates prolonged prostration periods, generating constant pressure in the
affected region. The causes are multifactorial and respond to intrinsic and
extrinsic factors. Among the former are the neuropathic, altered autonomic
control, infection, age, sensory deficit, mobility, altered mental status,
fecal/urinary incontinence, occlusion of small vessels, anemia and malnutrition.
Among the extrinsic factors, pressure, shear, friction and humidity are
mentioned. Both play an important role in ulcer formation [3].
Gluteal flaps have been used for treating
sacral sores since 1970. Since then, diverse treatment methods have been
developed; the most popular methods are a myocutaneous and fasciocutaneous
flaps being the former the one with more advantages and benefits in paraplegic
patients because although there is total or partial loss of gluteus maximus
muscle function, this deficit has no relevance [4].
TECHNIQUE
Under
general anesthesia, the patient is placed in a prone position. Antisepsis
protocol and sterile field placement are
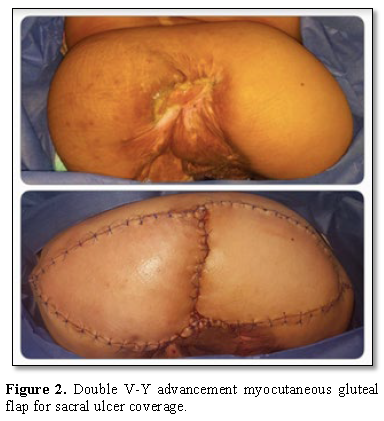
Large triangular skin islands were marked and
incised with the medial side being slightly larger than the residual defect and
lying adjacent to it. The superolateral border of the gluteus maximus muscle
was isolated and divided. The muscle was elevated away from the underlying
gluteus medium muscle, beginning laterally and proceeding medially, with
careful to identify and preserve de gluteal vessels. Then, the rest of the
origin of the muscle and its inferior portion are divided. After that, the
muscle and its skin island were advanced as a unit to the midline and sutured
with the contralateral flap. The defect is the closed as a V-Y advancement flap
and the donor site closed primarily (Figure 2) [5].
DISCUSSION
Local and regional flaps are the first option
for coverage of sacral ulcers. Although multiple flaps of this type have been
described, we believe that double V-Y advancement myocutaneous gluteal flap is
the best option in this kind of patients because of its multiple advantages:
1. Easy
design
2. Technically
simple
3. Great
mobility that allows covering large areas
4. Low
rate of complications
5. Adequate
vascularity
6. Plentiful
thickness that allows to cover deep areas and that avoids recurrences
7. Preservation
of the reconstructive principle like to like
8. Although
there is total or partial loss of gluteus maximus muscle function, this deficit
has no relevance
This flap have the disadvantage of the muscle
function lost because of the disruption of its origin and insertion, however,
in paraplegic patients, like in this case, this have no consequences.
1.
Reddy M, Gill SS, Rochon PA
(2006) Preventing pressure ulcers: A systematic review. JAMA 296: 974-984.
2.
Cushing CA, Phillips LG (2013)
Evidence-based medicine: Pressure sores. Plast Reconstr Surg 132: 1720-1732.
3.
Brandeis GH, Ooi WL, Hossain M,
Morris JN, Lipsitz LA (1994) A longitudinal study of risk factors associated
with the formation of pressure ulcers in nursing homes. J Am Geriatr Soc 42:
388-393.
4.
Ger R (1971) The surgical
management of decubitus ulcers by muscle transposition. Surgery 69: 106-110.
5.
Fisher J, Arnold PG, Waldorf J,
Woods JE (1983) The gluteus maximus musculocutaneous V-Y advancement flap for
large sacral defects. Ann Plast Surg 11: 518-519.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Rheumatology Research (ISSN:2641-6999)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)