2753
Views & Citations1753
Likes & Shares
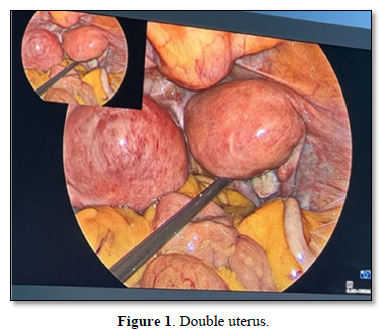
Bicornuate uterus is a common type of uterine malformation, taking the form of a double uterus with a single cervix and vagina. In this journal, we report a case of 43 year old who presented with complaints of heavy menstrual bleeding and was diagnosed to have bicornuate uterus with multiple small fibroids. Here we highlight the surgical techniques performed during laparoscopic hysterectomy to prevent complications and overcome the unique challenges associated with this case in a tertiary care center.
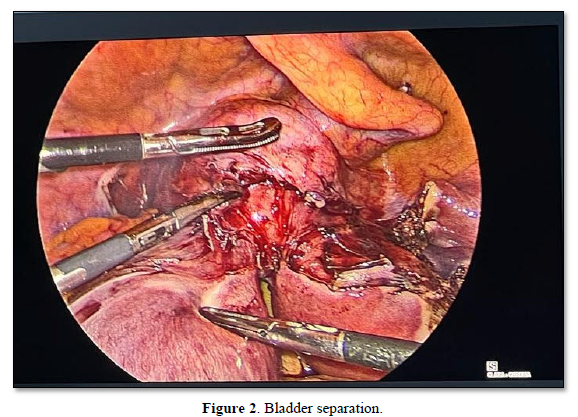
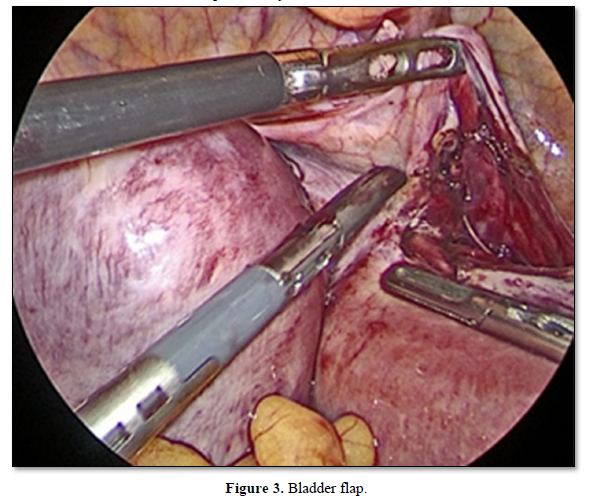
We proceeded with step by step dissection by carefully identifying the anatomy and dissecting through the planes. Bilateral ureters were identified and dissected to prevent any ureter injury and a wider bladder flap was separated for ease (Figure 3).
The specimen was removed through the vagina with two distinct horns of uterus separately and vault sutured (Figure 4).
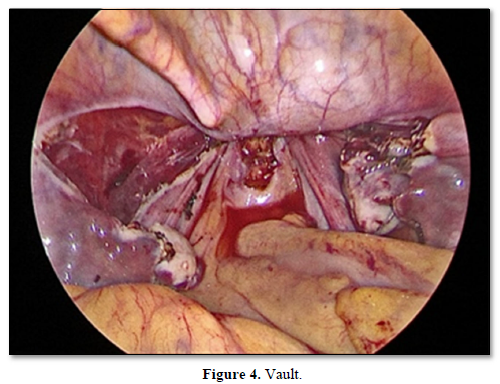
Cut section of the specimen showed, two separate horns of the uterus with two distinct endometrial cavities with single cervix (Figure 5).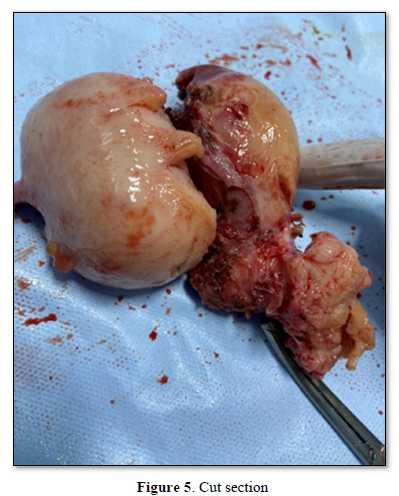
DISCUSSION
Laparoscopic hysterectomy in a double uterus is quite challenging as the anatomy is a bit different from the normal uterus. In the cases of mullerian anamolies, dedicated preoperative imaging of the renal tract to ruled out urinary tract abnormalities that may be associated with congenital Müllerian duct anomalies (MDAs). Renal agenesis is seen in 30% of mullerian anomalies. Hence accurate diagnosis should be made and proper planning prior to surgery should be undertaken to avoid intraoperative complications.
Accurate knowledge of the course of ureter is required for surgeons starting on complex laparoscopic, open and vaginal surgery.
Both the ureters are identified in the pelvic side walls and marked down throughout the course. Then the surgery is begun. Along with dissection of side walls, bladder flap is dissected widely to facilitate a wider colpotomy. To separate the bladder we can retro fill with co2, methylene blue to delineate the plane and create a wider bladder flap. Then after identifying proper course and uterine anatomy we can proceed with step wise cutting of uterine supports making sure that we are closer to uterus.
The Key points of surgical safety are identification of ureter (Bilateral ureterolyis), and ligating the uterine arteries at their origin, which would be done only after proper placement of colpotomy cup which would allow proper division of uterine arteries.
CONCLUSION
Minimally invasive procedure is ideal for patients with Mullerian duct anomalies. Identifying the ureters and additional renal anomalies is the foremost step to complete hysterectomy safely in these patients. Planning and mental preparedness is required while approaching complex surgical cases which are the key to successful management of the cases that deviate from the “norm”.
- Ng'ang'a N, Ratzersdorfer J, Abdelhak Y (2017) Vaginal birth after two previous caesarean deliveries in a patient with uterus didelphys and an interuterine septal defect. BMJ Case Rep 2017: bcr2016219149.
- Agu PU, Okaro JM, Mbagwu UK, Obi SN, Ugwu EOV (2012) Spontaneous rupture of gravid horn of bicornuate uterus at mid trimester--a case report. Niger J Med 21(1): 106-107.
- Chan YY, Jayaprakasan K, Zamora J, Thornton JG, Raine-Fenning N, et al. (2011) The prevalence of congenital uterine anomalies in unselected and high-risk populations: A systematic review. Hum Reprod Update 17(6): 761-771.
- Jayaprakash S, Muralidhar L, Sampathkumar G, Sexsena R (2011) Rupture of bicornuate uterus.BMJ Case Rep 2011: bcr0820114633.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- BioMed Research Journal (ISSN:2578-8892)
- Journal of Allergy Research (ISSN:2642-326X)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)






