2846
Views & Citations1846
Likes & Shares
An
incidental dural tear is a well-known complication in both open and
percutaneous lumbar spine surgery. Several techniques have been described for
surgical repair of dural tears in open lumbar spine surgery. However, the
treatment of iatrogenic dural tears in endoscopic spinal surgery remains
challenging. The objective of this report is to describe a technique for
endoscopic dural closure using a collagenous patch derived from bovine
pericardium (Tutopatch) which is simple and effective.
Keywords: Dural tear, Percutaneous endoscopic lumbar
discectomy, Tutopatch
Abbreviations: PELD:
Percutaneous endoscopic lumbar discectomy; CSF: Cerebro-spinal fluid; MRI:
Magnetic resonance imaging
INTRODUCTION
An incidental
dural tear is a relatively common complication of spine surgery. Its prevalence
ranges from 1% to 17% in open microsurgical techniques [1]. The incidence of a
dural tear in percutaneous endoscopic techniques is considered to be relatively
low. In a review of 816 consecutive patients who underwent Percutaneous
Endoscopic Lumbar Discectomy (PELD), Ahn et al. reported an incidence of 1.1%
[2]. In case of a dural tear in open lumbar spine surgery, several techniques
have been described for surgical repair. However, the standard technique of
suturing the tear is difficult, if not impossible, in PELD because of the
limited working space and the difficulty in handling the surgical instruments
within the narrow working channel of the endoscope. In these cases, the surgeon
is usually obliged to terminate the endoscopic procedure and convert to open
technique to be able to repair the dural tear and prevent its complications.
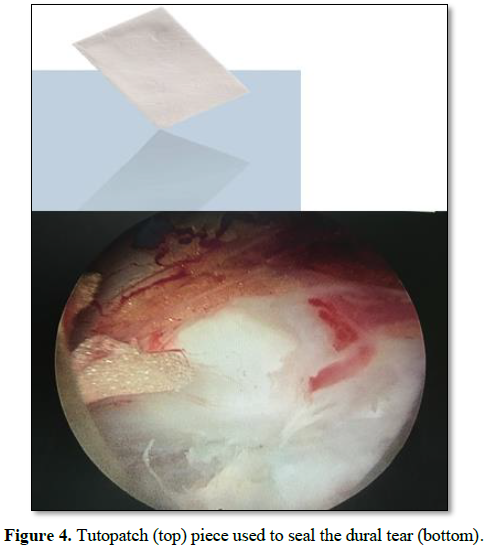
In this report, we describe a case of
incidental dural tear during percutaneous endoscopic interlaminar discectomy
that was treated successfully using a collagenous patch derived from bovine
pericardium (Tutopatch).
CASE REPORT AND TECHNICAL NOTES
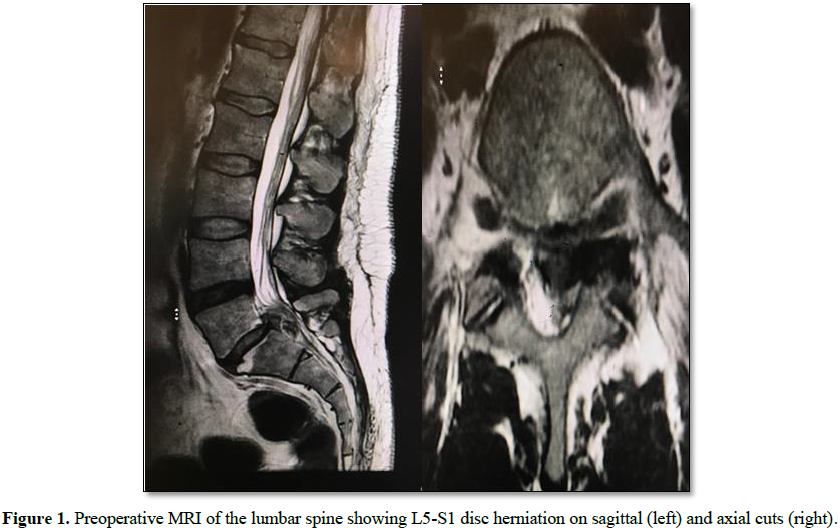
A 45 years old male patient presented
with a large, left-sided, L5-S1 disc herniation associated with bilateral pars
defect and low grade spondylolisthesis resulting in severe radical pain in the
left leg that failed to respond to conservative treatment (Figure 1). Dynamic X-rays of the lumbar spine did not show significant
movement of L5 over S1 (Figure 2).
Surgical options were discussed fully
with the patient including the possibility of fusion and instrumentation at
L5-S1 level. Patient elected to undergo percutaneous endoscopic discectomy to
relieve his sciatic pain and delay fusion at this level. The procedure was done
in the prone position under general anesthesia using the interlaminar approach
from the left side. After removal of the herniated disc fragments, a dural tear
affecting the S1 nerve root sleeve was noted in Figure 3.
The patient was kept on flat bed rest for 24 h after which
he was allowed to ambulate freely. He did not report any symptoms related to
CSF leakage like headache, nausea, vomiting or neck pain and stiffness. A
two-week follow up MRI of the lumbar spine showed no signs related to CSF
leakage (Figure 5).
Regular follow up of the patient at 2
weeks, 6 weeks and 3 months showed complete resolution of his symptoms except for
mild numbness along the dermatomal distribution of the S1 nerve root.
DISCUSSION
An incidental dural tear is a well-known
complication in any spine surgery. Its treatment in open techniques is well
described in the literature. However, treatment of dural tears in percutaneous
endoscopic lumbar discectomy is still considered a challenging problem, even
for highly experienced endoscopic spine surgeons. As the use of this endoscopic
technique increases, the risk of having incidental dural tears also increases.
The incidence of dural tears in PELD is
relatively low.
Chumnanvej et al. [3] described 60
patients who had full endoscopic lumbar discectomy via interlaminar approach.
There were no serious neurological complications or dural tears. Ahn et al. [2]
reported on 816 consecutive patients who underwent PELD using the
transforaminal approach for treatment of symptomatic lumbar disc herniation.
Only nine patients (1.1%) experienced symptomatic dural tears.
Dural tears during PELD might be recognized either intraoperatively or
might be missed and diagnosed postoperatively. The postoperative clinical
manifestations of dural tears in PELD are different from those of open lumbar
discectomy. In open techniques, patients with dural tears usually present with
signs and symptoms related to cerebrospinal fluid leakage like postural
headache, nausea, vomiting, dizziness and photophobia. In addition, these patients might present with large fluid
collection at the surgical site.
However, in PELD, there is no dead space for collection of
CSF and as such fluid collection in the wound or CSF leakage through the wound
is rare and most of these patients usually present with recurrence of the
radicular pain, with or without neurological deficit. According to Ahn et al.
[2], these signs and symptoms may be due either to nerve root irritation
secondary to exposed nerve rootlets or to nerve root herniation through the
dural defect. Patients with nerve root irritation usually present with
intractable leg pain without neurological deficit while patients with nerve
root herniation usually present with leg pain associated with neurological
deficit.
The management protocol of dural tears in
PELD has not been well described in the literature. Direct suture repair, like
in open surgeries, is technically difficult, if not impossible due to the
limited working space. When an iatrogenic dural tear is recognized
intraoperatively, the surgeon is usually forced to convert to open technique
and perform direct repair under microscopic visualization. Ahn et al. [2] stated
that the intraoperative attempt to repair the defect by shielding materials is
ineffective and the proper management option is immediate open conversion and
direct repair of the dural tear.
However, surgical repair of the dural defect
without direct suturing is also a well-known technique in open spine surgery.
Several studies in the literature reported good clinical results with dural
repair using fat or muscle graft, fascia graft, various sealants materials like
fibrin glue, or other closure adjuncts such as dural grafts and patches [4,5,6].
The technique described above is simple
and does not require the use of any suturing materials. It entails the use of
intradural and epidural patch to repair the dural defect (double-layered
duraplasty). Using only an epidural patch will not resist the pressure of a CSF
leak. If an intradural patch is added, then the CSF pressure will push the
patch against the dural wall defect and prevent any CSF leakage or rootlets
herniation. Hence, this method will provide a more watertight dural repair than
a one-layer dural patch. In addition, the collagen matrix initiates clot
formation, resulting in a chemical seal. It also provides a chemical signal for
fibroblasts infiltration which deposit new collagen, thereby reconstituting new
dura.
It is well known that dural tears
involving the nerve root sleeves are difficult to be repaired by primary
suturing as this may theoretically result in stenosis of the a affected root.
As such, they are managed without suture repair. The technique described above
avoids this complication by closing the dural defect without narrowing the
nerve root sleeve. Our aim is not to prevent CSF leakage as this rarely occurs
in percutaneous endoscopic procedures but to prevent nerve rootlets irritation
or herniation.
CONCLUSION
Dural tears in percutaneous endoscopic lumbar discectomy is
considered a challenging complication. There is no golden standard for
treatment of dural tears in endoscopic spine surgery. We propose a simple
surgical technique for repair of dural defects in PELD using a collagen patch
(Tutopatch) and the regular endoscopic instruments.
CONFLICT OF INTERESTS
1. Deyo
RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA (1992) Morbidity and mortality in
association with operations on the lumbar spine. The influence of age,
diagnosis, and procedure. J Bone Joint Surg Am 74: 536-543.
2. Ahn
Y, Lee HY, Lee S-H, Lee JH (2011) Dural tears in percutaneous endoscopic lumbar
discectomy. Eur Spine J 20: 58-64.
3. Chumnanvej
S, Kesornsak W, Sarnvivad P, Paiboonsirijit S, Kuansongthum V (2011) Full
endoscopic lumbar discectomy via interlaminar approach: 2-year results in
Ramathibodi Hospital. J Med Assoc Thai 94: 1465-1470.
4. Gautschi
OP, Stienen MN, Smoll NR, Corniola MV, Tessitore E, et al. (2014) Incidental
durotomy in lumbar spine surgery - A three-nation survey to evaluate its
management. Acta Neurochir (Wien) 156: 1813-1820.
5. Grannum
S, Patel MS, Attar F, Newey M (2014) Dural tears in primary decompressive
lumbar surgery. Is primary repair necessary for a good outcome? Eur Spine J 23:
904-908.
6. Shibayama
M, Mizutani J, Takahashi I, Nagao S, Ohta H, et al. (2008) Patch technique for
repair of a dural tear in micro endoscopic spinal surgery. J Bone Joint Surg Br
90: 1066-1067.
7. Choi
G, Lee SH, Raiturker PP, Lee S, Chae YS (2006) Percutaneous endoscopic
interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a
rigid working channel endoscope. Neurosurgery 58: ONS59-68.
8. Chen
HT, Tsai CH, Chao SC (2011) Endoscopic discectomy of L5-S1 disc herniation via
an interlaminar approach: Prospective controlled study under local and general
anesthesia. Surg Neurol Int 2: 93.
9. Oertel
JM, Burkhardt BW (2017) Full endoscopic treatment of dural tears in lumbar
spine surgery. Eur Spine J 26: 2496-2503.
10. Sencer
A, Yorukoglu AG, Akcakaya MO (2014) Fully endoscopic inter laminar and
transforaminal lumbar discectomy: Short-term clinical results of 163 surgically
treated patients. World Neurosurg 82: 884-890.
11. Shin
JK, Youn MS, Seong YJ, Goh TS, Lee JS, et al. (2018) Iatrogenic dural tear in
endoscopic lumbar spinal surgery: Full endoscopic dural suture repair (Youn’s
technique). Eur Spine J 27: 544-548.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Pathology and Toxicology Research