872
Views & Citations10
Likes & Shares
Purpose: A
spinal angiolipoma is a rare benign tumor of the spinal axis. It is most common
in the mid-thoracic spine and found predominantly in females. Pure lumbar
epidural angiolipomas are very rare. We report three cases of epidural
angiolipomas involving solely the lumbar region and review the associated
literature.
Methods: We
reviewed three cases of lumbar angiolipomas from two academic centers from 2012
to 2016. The tumor character was confirmed by the preoperative imaging study
and pathological report. All had similar clinical manifestations, lower back
discomfort or bilateral lower limb radicular symptoms and characteristic
presentation in magnetic resonance imaging (MRI).
Results: From
2012 to 2016, there were three cases included for analysis, including two males
and one female. All cases presented with symptomatic spinal pain, and MRI study
showed the tumors were located at lumbar spine level. We performed laminectomy
according to the locations of the tumors to achieve grossly total tumor
excision or en bloc resection. All patients recovered uneventfully with fair
post-operative neurological outcomes.
Conclusion: Spinal
angiolipomas are rare benign tumors. For the patients with symptomatic
presentation, MRI provides pre-operative clues for such tumor. En bloc
resection should be considered in the symptomatic patients to relieve the
compression of spinal cord or nerves.
Keywords: Spinal tumor, Spinal angiolipoma,
En bloc resection
INTRODUCTION
Spinal angiolipomas are rare benign tumors,
and they account for 0.14-1.2% of all spinal axis tumors [1]. The lesions are
most common in the mid-thoracic spine and found predominantly in females [1,2].
The pathological presentation is mature adipose tissue and abnormal vessels
[1,3-5]. The two subtypes of spinal angiolipomas are non-infiltrating and
infiltrating [5]. We report three cases of epidural non-infiltrating
angiolipomas, located solely at the lumbar spine, which is a rare occurrence,
and discuss the clinical presentations, pathogenesis, radiography and
management of the lesions.
CASE REPORT 1
A 79 year old man presented with a 2 year
history of progressive pain, numbness and weakness in the bilateral lower
extremities. The pain was improved by medication in the beginning but not
resolved in recent months. Physical examination revealed intermittent
claudication such that he was able to walk for 5 min or 200 m only.
Neurological examination revealed bilateral positive straight leg rising of 45°
and paresthesia below the L4 dermatome. The muscle strength of bilateral ankle
dorsiflexion was 4/5. No urinary incontinence was noted during this period. The
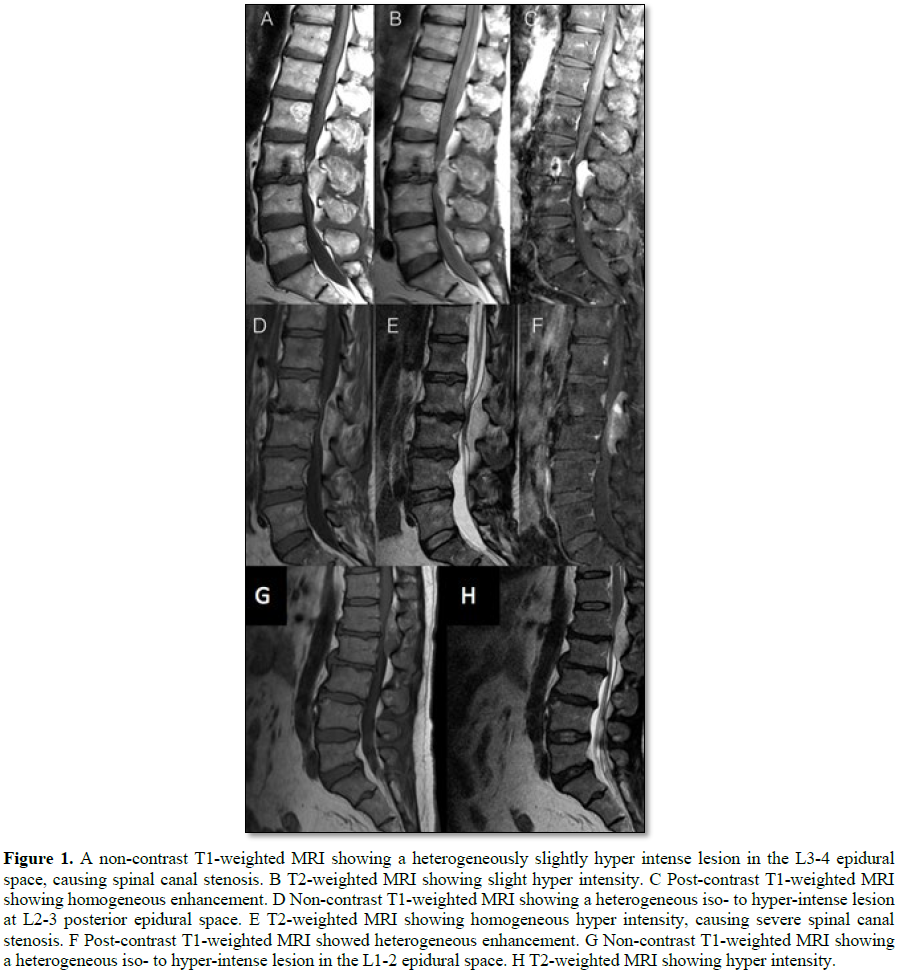
lesion was heterogeneous and slightly hyperintense in T1-weighted images (T1WI) and T2-weighted images (T2WI) of
We performed L2-4 laminectomy and tumor
excision. The operative findings revealed severe L2-4 thecal sac compression by
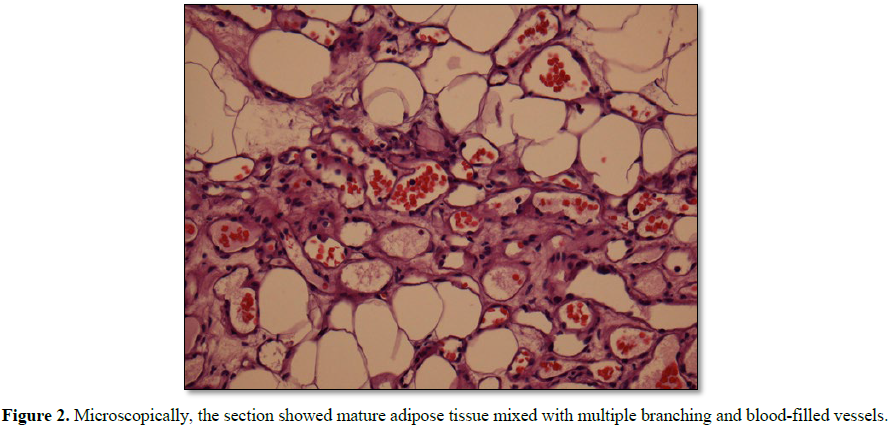
a well-demarcated neoplasm of about 2.5 × 1.5 cm in size. The pathological
presentation was an angiolipoma composed of a collection of mature adipose
tissue with varying numbers of vascular structures (Figure 2). The patient recovered well and had no further neurological
complaints. There was no recurrence on follow-up MRI 2 years after the
operation.
CASE REPORT 2
A 45 year old female had complained of
progressive bilateral lateral thigh pain and numbness for two years prior to
her visit to the hospital. Progressive claudication had developed rapidly in
recent months and she could not walk more than 100 m when she visited the
clinic. There was no urinary or stool incontinence. MRI showed a fusiform mass
of about 53 mm in cranio-caudal diameter, with extension to the bilateral
neural foramen, in the posterior epidural space of the L2-3 level, with
heterogeneous but predominant high T1W and T2W signal intensities. There was
enhancement in the post-contrast series (Figures
1D-1F).
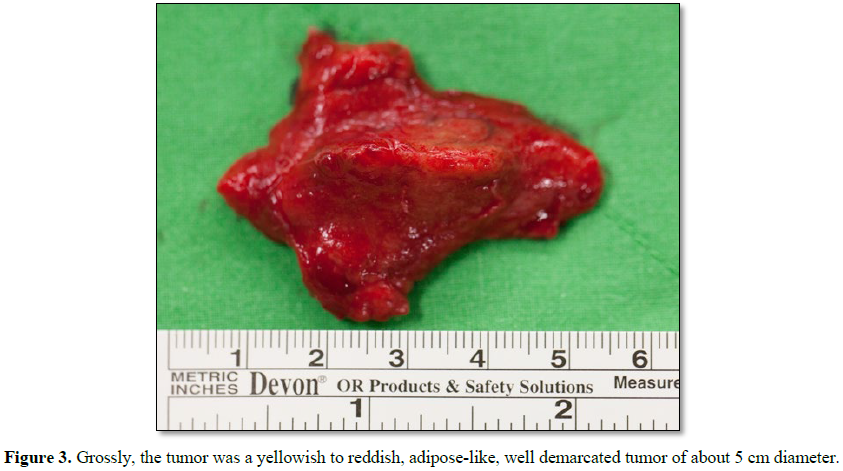
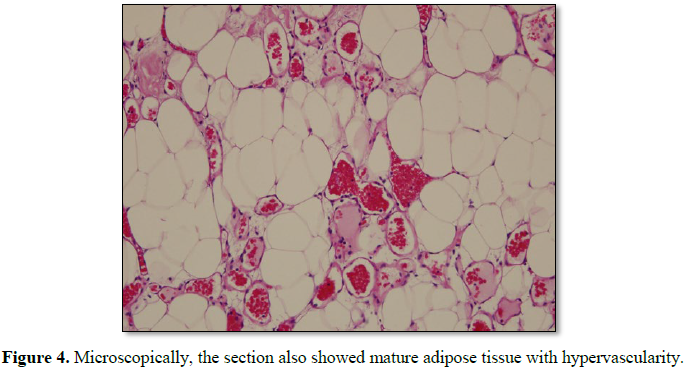
We performed L2 laminectomy for en bloc tumor
excision. One adipose-like, well-demarcated neoplasm with profound vascularity
was noted in the epidural space of L2-3 (Figure
3). The neoplasm was located on the dorsal side of the thecal sac with
extension to the bilateral neural foramen of L2-3. The thecal sac and bilateral
L2 roots were deviated anteriorly. The pathology indicated angiolipoma as well (Figure 4).
CASE REPORT 3
A 53 year old man presented with severe lower
back soreness and pain with bilateral lower leg numbness for more than six
months. Later intermittent claudication caused him to seek medical assistance
in the clinic. MRI showed a 4 × 1.5 cm epidural lesion at L1-2 causing severe
thecal sac compression, which was to hyper intense in TIWI and hyperintense in
T2WI (Figures 1G and 1H). He received
conservative treatment but the effect was limited. We performed T12-L2
laminectomy for tumor excision. Operative findings showed a 4 × 1.5 × 1 cm
yellowish and elastic-soft tumor in the epidural space with thecal sac
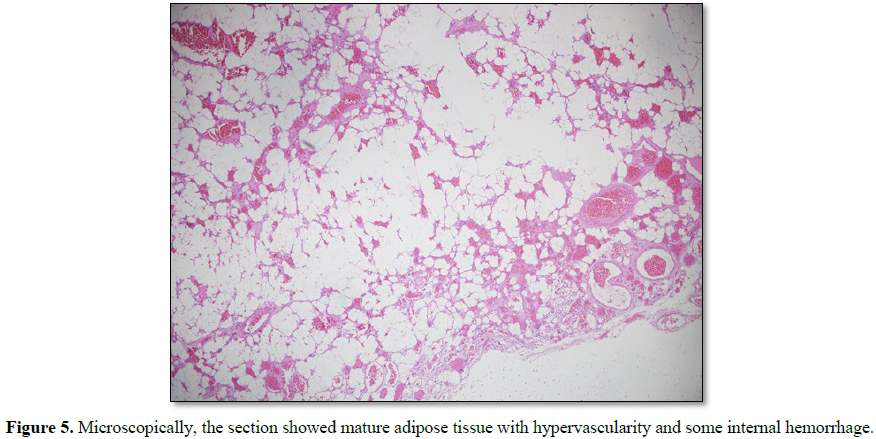
compression. Post-operatively, he recovered well. The pathology represented
typical characteristics of angiolipomas (Figure
5).
DISCUSSION
Angiolipomas are benign tumors that usually
appear in the forearm, trunk or neck and rarely in the spinal canal [6]. The
first case of spinal angiolipoma was reported by Berenbruch in 1890 [7] in an
autopsy of a 16 year old boy after an unsuccessful operation. Spinal
angiolipomas are predominantly located in the mid-thoracic region and are more
common in females. Lumbar spinal angiolipomas are extremely rare and the first
was reported by Kasper and Cowan in 1931 [8].
The typical pathology presentation of an
angiolipoma is a benign neoplasm composed of mature adipose tissue and abnormal
vessels [9]. It may be classified within the spectrum between lipoma and
hemangioma [10]. The ratio of fat to vessels is variable, ranging from 1:3 to
2:3 [11]. In 1974, Lin and Lin [5] classified spinal angiolipomas into two
types: non-infiltrating and infiltrating. The non-infiltrating subtype is more
common. Both subtypes are benign tumors; however, the infiltrating subtype
invades surrounding tissues, such as the vertebral body. Non-infiltrating
lesions are almost always located in the posterior epidural space, while
infiltrating lesions appear mostly in the anterior or anterolateral space with
vertebral body and pedicle invasion [12,13].
Spinal angiolipomas cause a slow progressive
clinical neurological presentation according to the level of the spinal canal
compromised [1]. Common subjective complaints include back pain and progressive
motor and sensory deficits below the affected spine level, with possible
progression to sphincter dysfunction in the late stage [14]. The symptoms tend
to develop slowly over months to years. However, sudden deterioration can occur
as a result of tumor thrombosis or hemorrhage, as reported in two different cases
by Labram et al. [15] and Anson et al. [16] Pregnancy is an aggravating factor,
and pregnancy termination may cause regression of symptoms, as reported by Cull
et al. [17] for two cases presenting paraparesis during pregnancy but remission
after parturition. Pregnancy may interfere with the drainage of venous blood
and increase epidural venous pressure due to compression of abdominal and major
veins, resulting in increased extracellular fluid, and the forceful Valsalva
maneuvers associated with vaginal delivery may acutely aggravate symptoms [18].
Other suggested possible factors, including vascular steal, could be a cause of
spinal cord ischemia, as well as pulsatile compression on the adjacent cord
because of its high vascularity [2].
In most cases, spine radiography is useful in
detecting vertebral bony destruction; i.e., erosion of the pedicles or
vertebral body, trabeculation, widened pedicles and foraminal widening [19].
Computed tomography will show a hypodense signal and can help in the assessment
of the involved bony lesion. Magnetic resonance imaging (MRI), considered the
best modality for diagnosing spinal angiolipomas, typically shows hyperintense
signals in a T1-weighted image without contrast, owing to their fatty content.
Provenzale and Mclendon [18] showed that large hypointense foci observed within
spinal angiolipomas on non-contrast T1-weighted images are correlated with
increased vascularity and most lesions are enhanced with gadolinium
administration. T2-weighted imaging can be variable but is usually
hyperintense.
Total surgical resection of the tumor is an
ideal treatment, depending on the location [20]. The non-infiltrating type is
located mainly in the posterior epidural space, so it can be removed through
posterior laminectomy approach. The infiltrating type is located mainly
anterior to the spinal canal and it is likely to affect the vertebral body, so
it can be approached through anterior, lateral, or mixed approach methods [21]
and sometimes, instrumentation of the involved vertebral body may be required.
The prognosis is excellent for both
non-infiltrating and infiltrating types. Although the infiltrating type is
difficult to remove completely with surgery, adjuvant or neoadjuvant
radiotherapy is not recommended, even when complete removal cannot be achieved,
because of the benign pathology.
CONCLUSION
Spinal angiolipomas are rare benign tumors
that cause slow progressive neurological deficit according to the level of the
spinal cord affected. MRI is the best modality for diagnosing spinal
angiolipomas. MRI shows heterogeneous hypo intensity in T1-weighted images and
hyperintensity in T2-weighted images, and most lesions are enhanced with
contrast administration. Total surgical resection is an ideal treatment.
Whether or not resection is complete, no adjuvant or neoadjuvant radiotherapy
is needed. The prognosis of both types of spinal angiolipomas is good.
1.
Preul MC, Leblanc R,
Tampieri D, Robitaille Y, Pokrupa R (1993) Spinal angiolipomas. Report of three
cases. J Neurosurg 78: 280-286.
2.
Turgut M (1996) Spinal
angiolipomas: Report of a case and review of the cases published since the
discovery of the tumour in 1890. Br J Neurosurg 13: 30-40.
3.
von Hanwehr R, Apuzzo
ML, Ahmadi J, Chandrasoma P (1985) Thoracic spinal angiomyolipoma: Case report
and literature review. Neurosurgery 16: 406-411.
4.
Gonzalez-Crussi F,
Enneking WF, Arean VM (1966) Infiltrating angiolipoma. J Bone Joint Surg Am 48:
1111-1124.
5.
Lin JJ, Lin F (1974)
Two entities in angiolipoma. A study of 459 cases of lipoma with review of
literature on infiltrating angiolipoma. Cancer 34: 720-727.
6.
Kuroda S, Abe H, Akino
M, Iwasaki Y, Nagashima K (1990) Infiltrating spinal angiolipoma causing
myelopathy: Case report. Neurosurgery 27: 315-318.
7.
Berenvruch K (1890) Ein
fall von multiplen Angiolipomen kombiniert mit einem Angiom des Rückenmarks..
8.
Kasper JAC (1931)
Extradural lipoma of the spinal canal. J Nervous Ment Dis 74: 564.
9.
Ehni G, Love JG (1945)
Intraspinal lipomas: Report of cases; review of the literature and clinical and
pathologic study. Arch NeurPsych 53: 1-28.
10.
Fourney DR, Tong KA,
Macaulay RJ, Griebel RW (2001) Spinal angiolipoma. Can J Neurol Sci 28: 82-88.
11.
Gelabert-Gonzalez M,
Garcia-Allut A (2009) Spinal extradural angiolipoma: Report of two cases and
review of the literature. Eur Spine J 18: 324-335.
12.
Guzey FK, Bas NS, Ozkan
N, Karabulut C, Bas SC, et al. (2007) Lumbar extradural infiltrating
angiolipoma: A case report and review of 17 previously reported cases with
infiltrating spinal angiolipomas. Spine J 7: 739-744.
13.
Leu NH, Chen CY, Shy
CG, Lu CY, Wu CS, et al. (2003) MR imaging of an infiltrating spinal epidural
angiolipoma. AJNR Am J Neuroradiol 24: 1008-1011.
14.
Miki T, Oka M, Shima M,
Hirofuji E, Tanaka S (1981) Spinal angiolipoma. A case report. Acta Neurochir
(Wien) 58: 115-119.
15.
Labram EK, el-Shunnar
K, Hilton DA, Robertson NJ (1999) Revisited: Spinal angiolipoma--three
additional cases. Br J Neurosurg 13: 25-29.
16.
Anson JA, Cybulski GR,
Reyes M (1990) Spinal extradural angiolipoma: A report of two cases and review
of the literature. Surg Neurol 34: 173-178.
17.
Cull DJ, Erdohazi M,
Symon L (1978) Extradural haemangiolipoma in the spinal canal. Two cases
presenting during pregnancy. Acta Neurochir (Wien) 45: 187-193.
18.
Provenzale JM, McLendon
RE (1996) Spinal angiolipomas: MR features. AJNR Am J Neuroradiol 17: 713-719.
19.
Si Y, Wang Z, Pan Y,
Lin G, Yu T (2014) Spinal angiolipoma: Etiology, imaging findings,
classification, treatment and prognosis. Eur Spine J 23: 417-425.
20.
Mohammed ZI, Ahmed MM
(2016) Spinal extradural angiolipoma manifested after normal vaginal delivery.
BMC Res Notes 9: 132.
21.
Turgut M (2011)
Thoracic epidural angiolipoma with extraspinal extension. Neurol India 59:
654-655.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- International Journal of AIDS (ISSN: 2644-3023)
- Journal of Spine Diseases
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Oncology Clinics and Research (ISSN: 2643-055X)
- Dermatology Clinics and Research (ISSN:2380-5609)