2383
Views & Citations1383
Likes & Shares
CASE REPORT
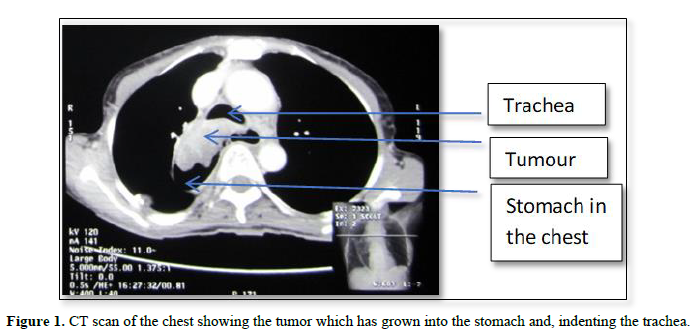
A 31-year-old lady had symptoms of achalasia. A couple of months later she had modified Heller’s operation. Ten years later, she presented with recurrence of the achalasia, complicated by a sigmoid esophagus. She then had esophagectomy with esophagogastrostomy (Ivor-Lewis). Fifteen years after the esophagectomy, she presented with severe weight loss and difficulty in breathing. The chest CT scan Figure 1 showed a tumor in the remnant (intrathoracic) esophagus infiltrating the trachea. There was no dysphagia. esophagoscopy confirmed the tumor, and the biopsy came out as squamous cell carcinoma of the esophagus. She passed away within a few days before radiotherapy could be commenced.
DISCUSSION
Achalasia of the cardia has long been known as a pre-malignant condition, with the esophageal carcinoma developing several years after the onset of symptoms of the achalasia. Durations varying from 5 to 24 years have been reported [1-4]. Although the prevalence of patients with achalasia developing an esophageal carcinoma is low the risk is nearly 140-fold; there is no difference in prognosis between patients with achalasia-carcinoma and those with esophageal cancer without achalasia [5]. Our patient developed the esophageal carcinoma 25 years after the initial presentation of the achalasia.
The chronic food stasis over the years affects the distal and mid-esophagus. This leads to irritation of the mucosa, which then leads to metaplasia, dysplasia and finally the carcinoma of the esophagus. Since the food stasis does not usually affect the cervical esophagus, it is often spared from the malignant change. At the second surgery, the patient had transthoracic esophagectomy, leaving behind part of the thoracic esophagus. This is the part that developed the carcinoma several years later. If the esophagectomy had involved the whole of the abdominal and thoracic esophagus, leaving behind only the cervical esophagus, it is unlikely that a malignancy would have developed later, since the cervical esophagus is often not involved with the chronic food stasis and irritation. It is therefore our opinion that when esophagectomy is considered for recurrent achalasia or failed modified Heller’s operation, the whole of the thoracic esophagus be removed, and the anastomosis done at the level of the cervical esophagus (with the colon or the stomach), to forestall malignant change in the remnant thoracic esophagus. There must also be long-term surveillance of achalasia patients.
CONCLUSION
Malignant transformation in the esophagus occurs several years after the initial diagnosis of achalasia. When esophagectomy is considered in the course of management of the achalasia, the whole of the thoracic esophagus must be removed and the anastomosis done with the cervical esophagus.
- Leeuwenburgh I, Scholten P, Alderliesten J, Tilanus HW, Looman CW, et al. (2010) Long-term esophageal cancer risk in patients with primary achalasia: A prospective study. Am J Gastroenterol 105(10): 2144-2149.
- Brücher BL, Stein HJ, Bartels H, Feussner H, Siewert JR (2001) Achalasia and esophageal cancer: Incidence, prevalence, and prognosis. World J Surg 25(6): 745-749.
- Peracchia A, Segalin A, Bardini R, Ruol A, Bonavina L, et al. (1991) Esophageal carcinoma and achalasia: Prevalence, incidence and results of treatment. Hepatogastroenterology 38(6): 514-516.
- Sandler RS, Nyrén O, Ekbom A, Eisen GM, Yuen J, et al. (1995) The risk of esophageal cancer in patients with achalasia. A population-based study. JAMA 274(17): 1359-1362.
- Brücher BL, Stein HJ, Feussner H, Bartels H, Siewert JR (1998) Achalasia and carcinoma of the esophagus: Incidence, prevalence and prognosis. Langenbecks Arch Chir Suppl Kongressbd 115: 1357-1359.
- Schlottmann F, Patti MG (2018) Esophageal achalasia: Current diagnosis and treatment. Expert Rev Gastroenterol Hepatol 12(7): 711-721.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Alcoholism Clinical Research
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Spine Diseases
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Journal of Renal Transplantation Science (ISSN:2640-0847)


