2309
Views & Citations1309
Likes & Shares
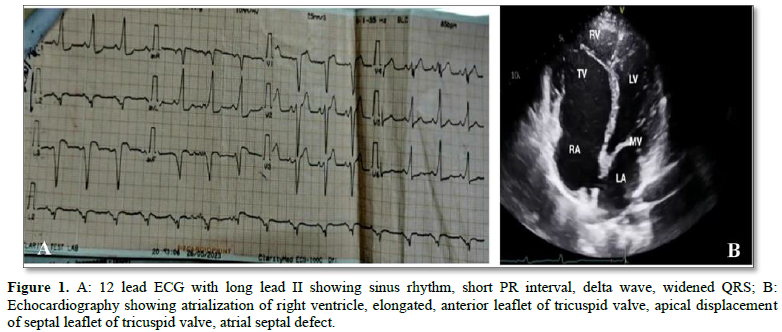
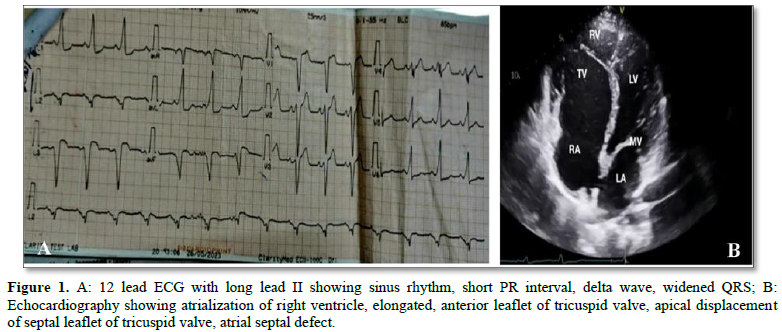
Abbreviations: RV: Right Ventricle; TV: Tricuspid Valve; RA: Right Atrium; LV: Left Ventricle; MV: Mitral Valve; LA: Left Atrium
CASE REPORT
Here we are presenting a case of a 28 years old man (Body mass index 23.89 Kg/mt2) diagnosed with Ebstein's Anomaly incidentally during pre-anesthetic checkup. He fell from a tree and got a fracture of both tibia and fibula (left leg) with eye injury scheduled for closed reduction and internal fixation with intramedullary interlocking tibia nail. He was completely asymptomatic since childhood. He had no complaints of exertional dyspnea, palpitations, tachyarrhythmias or chest pain. There were no signs of congestive cardiac failure on physical examination. On auscultation pan systolic murmur was heard at lower left sternal border suggestive of tricuspid reguirgitation. His laboratory investigations were normal except short PR interval, wide QRS, delta wave found in electrocardiogram and cardiomegaly in digital x-ray of chest (posterior - anterior view). These abnormalities lead to further detailed investigation and 2D Echo revealed a moderate size 18 mm ostium secundum Atrial septal defect with left to right shunt, elongated, sail like anterior leaflet of tricuspid valve, 3 mm apical displacement of septal leaflet of tricuspid valve (diagnostic of Ebstein’s anomaly), no evidence of Pulmonary artery hypertension at rest, Left ventricular ejection fraction - 58% and jerky septal wall motion. A 24 h Holter recording was started soon after diagnosis and ventricular ectopic beats with a total burden of 1.7%, which were of no significance were found. Patient was scheduled for surgery after getting fitness from a cardiological point of view. He was premedicated with oral alprazolam 0.25 mg on the night before and on the morning of surgery (Figure 1).
Monitoring on the operation table was done with electrocardiography (ECG), pulse oximetry, noninvasive blood pressure and urine output. One 18G intravenous line was established. Cardiologist was appointed for any adverse situation and emergency medications alongside antiarrhythmic medications (injection amiodarone) were kept ready. Prophylactic treatment for infective endocarditis with Injection (Inj) ceftriaxone 1g intravenous (IV) and antiemetic treatment with inj ondansetron 8 mg IV were given slowly. Precautions were taken to prevent air bubbles and paradoxical air embolism. For better analgesia distal sciatic nerve block in popliteal fossa and femoral nerve block in femoral triangle was performed under ultrasound guidance (E cube 8 ultra sound: probe L3-12T straight) with 100 mm 22g USG compatible nerve block needle with 0.2 % ropivacaine of 20 ml for distal sciatic nerve and 10 mL for femoral nerve. Supine position was maintained during surgery.
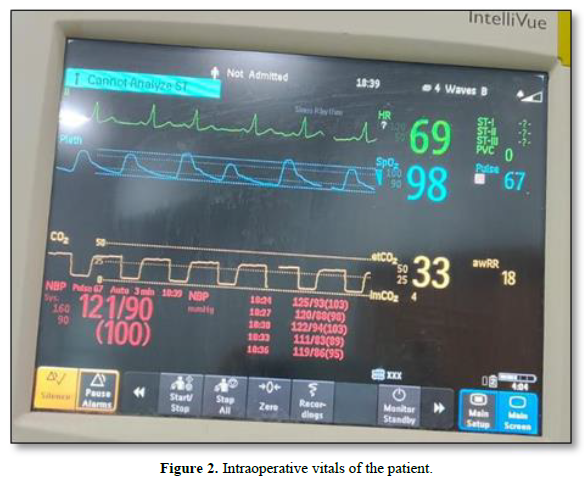
General anesthesia was given with inj Etomidate 24 mg IV after giving inj Fentanyl 150 mcg IV, inj midazolam 2 mg IV as premedication. Inj loxicard was administered to prevent laryngeal surge thereby reducing any chances of sympathetic stimulation. Inj Rocuronium 60 mg IV used as muscle relaxant induced agents. Direct laryngoscopy was done and intubated with an endotracheal tube with internal diameter of 8.5 mm and fixed at 22 cm. Patient was then put on a ventilator of following settings - Volume Control mode, Tidal volume 450 ml, I: E 1:2; No positive end expiratory pressure was used. End Tidal CO2 (EtCO2) maintained between 25 and 35 mmHg General anesthesia was maintained in closed circuit with inhalational agent sevoflurane and muscle relaxation maintained with inj vecuronium 1 mg at 30 minutes intervals. For analgesia infusion Paracetamol 1g was given through intravenous route before skin incision. The operation lasted for 150 minutes and in total 1.5 liters of ringer's lactate solution was transfused during the surgery after proper assessment of fluid status through inferior vena cava diameter which was maintained around 1.7 cm. Intraoperatively ECG showed short PR interval, delta wave, widened QRS and two episodes of tachycardia (HR 110-120 beats per minute) which reverted back to normal sinus rhythm without any intervention and was maintained till the end of the surgery. The patient remained hemodynamically stable with systolic blood pressure in the range of (110-130) mm of Hg and diastolic blood pressure (80-90) mm of Hg, with well-maintained saturation in the intraoperative period. Total urine output and blood loss during the intraoperative period was 500 mL and 600 mL respectively (Figure 2).
Patient was extubated with a stable arterial pressure, heart rate and a good urine output. Inj Loxicard and inj Neostigmine methyl sulfate 2.5 mg and inj glycopyrrolate 0.5 mg were administered during extubation. One episode of tachycardia was noted however no hypotension was observed even shortly after removal of the endotracheal tube. After the surgery the patient was shifted to the Post Anesthesia Care Unit (PACU) for 24 h for hemodynamic observation. Pain control was also assessed using Visual analogue scale (VAS) score in PACU and it was around 0-4 during the first 24 h of the postoperative period. No antiarrhythmic medication was used postoperatively however inj Tramadol 100 mg intravenous for three times was scheduled for better pain management. Patient was shifted from PACU to general ward after 24 h of close monitoring with stable hemodynamic condition.
DISCUSSION
The goal of anesthesia in this patient is to maintain sinus rhythm and both preload and afterload. The major problems associated with Anesthesia in Ebstein's anomaly are the risk of arrhythmias and the possibility of decreasing the arterial oxygen tension further by an increase of the right to left shunt. Subarachnoid blocks and general anesthesia can cause sudden decrease in systemic vascular resistance which can potentially worsen the right to left cardiac shunt. We avoid Spinal anesthesia as it can lead into sharp fall in systemic vascular resistance which causes sudden hypotension. Sudden hypotension has a major effect on cardiac output as well as contractility of the right atrium and RV. General anesthesia is also associated with increased catecholamine levels and intrathoracic pressure. These can increase intracardiac shunt [4]. However, precautions before surgery, reduced intubation time, inhibition of sympathetic stimulation like laryngeal surge, watchful monitoring, taking good care of fluid status, maintaining deep plane of anesthesia and adequate analgesia make general anesthesia effective for lower limb surgery in a case of Ebstein's Anomaly. Here in this case, we use ultrasound guided direct visualization of the needle, nerve, and any nearby vascular structures which minimizes the chance of nerve injury, local anesthetic toxicity, and accidental puncture of a blood vessel. By avoiding epidural analgesia, we minimize the chances of hypotension, nerve damage, epidural hematoma, spinal cord infection and accidental dural puncture.
Hannam [5] found that etomidate as an induction agent didn't cause reduction in mean arterial pressure (MAP) integral from baseline after induction of anesthesia and less frequent use of vasopressors [5]. Use of vasopressors with strong beta-adrenergic stimulant action is better to avoid in this context as they have direct effect on myocardium. Wierda, Schuringa and van den Broek [6] found that Rocuronium because of its weak vagolytic effect in its intubating dose apert from hemodynamic effects related to muscle paralysis, did not lead to increase in heart rate without change in MAP. We avoid Succinylcholine as muscle relaxant which further decreases any possibility of hyperkalemia induced arrhythmia. In this case central venous catheterization was not performed as it has higher propensity for tachyarrhythmias and paradoxical embolism [7]. Every effort was made to prevent any excess fluid administration which can lead to an increase in right to left shunt and hypoxia. Hypercapnea and hypercapnea induced hypotension inhibited by maintaining EtCO2 in the range of 25-35 mm of Hg.
Therefore, we conclude that anesthetic challenges in patients with Ebstein's anomaly depend on physical status of the patients, type of surgery, mode of analgesia and monitoring techniques [8].
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
- Fuchs MM, Connolly HM (2020) Ebstein Anomaly in the Adult Patient. Cardiol Clin 38(3): 353-363.
- Holst KA, Connolly HM, Dearani JA (2019) Ebstein’s Anomaly. Methodist Debakey Cardiovasc J 15(2): 138.
- Stephens EH, Dearani JA, Qureshi MY, Ammash N, Maleszewski JJ (2020) The Congenital Tricuspid Valve Spectrum: From Ebstein to Dysplasia. World J Pediatr Congenit Heart Surg 11(6): 783-791.
- Lobato EB, Florete OG, Paige GB, Morey TE (1998) Cross-sectional area and intravascular pressure of the right internal jugular vein during anesthesia: Effects of Trendelenburg position, positive intrathoracic pressure, and hepatic compression. J Clin Anesth 10(1): 1-5.
- Hannam J, Mitchell S, Cumin D, Frampton C, Merry A, et al. (2019) Haemodynamic profiles of etomidate vs propofol for induction of anesthesia: A randomized controlled trial in patients undergoing cardiac surgery. Br J Anaesth 122(2): 198-205.
- Wierda JM, Schuringa M, van den Broek L (1997) Cardiovascular effects of an intubating dose of rocuronium 0.6 mg kg-1 in anaesthetized patients, paralyzed with vecuronium. Br J Anaesth 78(5): 586-587.
- Horishita T, Minami K, Koga K, Ogata J, Sata T (2005) Anesthetic management using echocardiography for surgery of lower extremity in a patient with Ebstein's malformation. Anesth Analg 101: 606–615.
- Sinha P, Kumar B, Varma P (2010) Anesthetic management for surgical repair of Ebstein′s anomaly along with coexistent Wolff-Parkinson-White syndrome in a patient with severe mitral stenosis. Ann Card Anaesth 13(2): 154.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of AIDS (ISSN: 2644-3023)
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Alcoholism Clinical Research
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)