2529
Views & Citations1529
Likes & Shares
Purpose:
To test the effectiveness of eye muscle exercise (EME) for improvement of
vision acuities (VAs) and amelioration digital eye strain (DES) or computer
vision syndrome (CVS) and asthenopia in children.
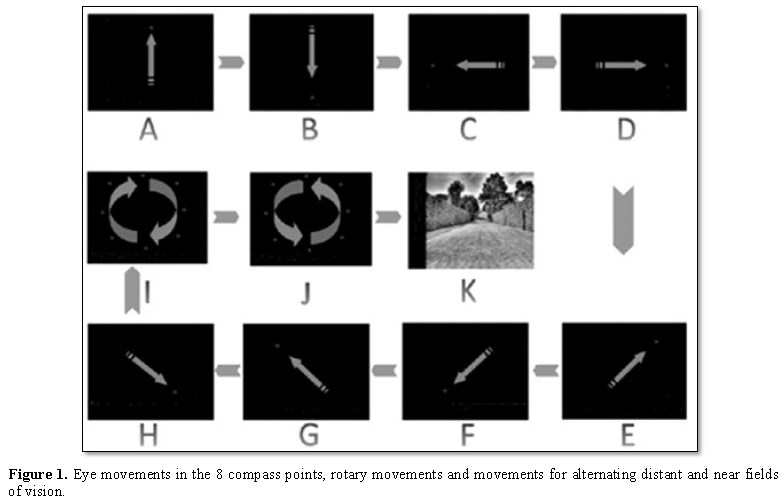
Methods: Prospective, comparative, non-invasive, pre-limited study was carried out in 30 DES children (12 females; mean age of 8.5 years old) with the VAs ranging from 0.1 to 1.0 decimal in right naked eyes; 0.5 to 1.5 decimal in left naked eyes. The device for EME utilizing eye movements in the 8 compass points, rotary movement and movements for alternating distant and near fields of vision to regulate and relax eyes was used for 10 min/time, 3 times/day in total 2 months.
Results:
VAs ranging from 0.3 to 1.2 decimal in right naked eyes (p=0.001); and
0.5 to 1.5 decimal in left naked eyes (p=0.004) were significantly improved
after EME for 2 months. Percentage of respondents reporting symptoms such as
blurred vision from 97% to 30%; difficulty or slowness in refocusing my eyes
from one distance to another from 70% to 33%; irritated or burning eyes from
37% to 17%; dry eyes from 60% to 20%; eye strain from 83% to 23%; headache from
7% to 3%; tired eyes from 67% to 30%; sensitivity to bright lights from 20% to
13%; eye discomfort from 90% to 27% and double vision from 13% to 0% were
reduced as well. Results revealed that EME ameliorate DES or CVS and
asthenopia.
Conclusion:
Daily EME improves VA of children with DES/CVS and asthenopia. Following
up 2 months, DES symptoms were ameliorated.
Keywords: Digital
eye strain, Computer vision syndrome, Asthenopia, Eye muscle exercise, Eyespa
Abbreviations: DES: Digital Eye Strain; CVS:
Computer Vision Symptoms; EME:
Eye Muscle Exercise; VA: Visual Acuity
INTRODUCTION
The
usage of digital device [1]
has been increased considerably in recent years [2,3]
in children [4,5],
so that extensive daily use for learning, homework and game purposes as well as
during leisure time is now normal at school and home. Digital eye strain (DES)
or computer vision symptoms (CVS) [6-8]
and asthenopia includes a range of ocular and visual symptoms [9,10].
Symptoms has two main categories: those linked to accommodative or binocular
vision stress [11,12]
and external symptoms linked to dry eye [13,14].
DES or CVS and asthenopia [15]
is identified using questionnaires [16]
or evaluations of parameters such as critical flicker-fusion frequency [17],
blink rate [18]
and completeness, accommodative function and pupil characteristics [19].
The management approaches for DES or CVS and asthenopia [20]
include correction of refractive error, management of dry eye, interaction
between accommodation and vergence [19],
regulating screen breaks [21]
and blue light-filtering spectacle lenses. New technology and developed method
of Eyespa give the possibility of amelioration to children with DES or CVS and
asthenopia. Eyespa utilizes
eye movements in the 8 compass points, rotary movement and movements for
alternating distant and near fields of vision to regulate and relax eyes.
This
prospective, comparative, non-invasive, prelimited study tests the hypothesis
of whether Eyespa is effective
in DES or CVS and asthenopia or not.
MATERIALS AND METHODS
Study design and patients
This prospective, comparative,
noninvasive, prelimited study,
supported by Asia Pediatric Ophthalmologist Association, was conducted by the Radiant
Children’s Hospital Group. The protocol and HIPAA compliant informed consent forms
were approved by the ethics committee of Radiant Children’s Hospital Group
(Beijing, China). The parent or the guardian of each study patient was given a
written informed consent.
Between
October 2018 and March 2019, 30 participants
(F=12, 40%) at the age 3 to 13 years old (mean age 8.5 ± 2.85) with DES
or CVS and their visual acuities ranging from 0.1 to 1.2 (mean 0.56 ± 0.196) decimal in naked eyes were enrolled
into this study at Beijing Radiant Children’s Hospital. DES or CVS was identified by accommodation parameters,
critical flicker-fusion frequency (CFF) and blinking characteristics.
Participates were excluded if they had any measurable heterotropia in primary
gaze at distance or near fixation in the prescribed spectacles or a documented
history of strabismus; other concomitant eye or other systemic diseases that
could impair vision. All participants had the parent or guardian maintain a
calendar on which EME received each day was logged. The calendars were reviewed
at follow up visits.
Ophthalmological
examinations
Before they took part in the experiment, a
comprehensive history was collected including the number and type of devices
being used (including desktop, laptop and tablet computers and smartphones),
viewing distance and gaze angle for each device, duration of use for each
device, monitor size (for a desktop computer, number of monitors being used),
the type of task being performed on each device, the size of the critical
detail being observed during the task. The participants were carefully
diagnosed for potential ocular pathological defects; and determined their
refraction through mydriasis optometry.
Accommodation testing and vergence testing were
performed including subjective amplitude of accommodation (minus lens),
accommodative response at preferred working distance (Cross-Nott retinoscopy),
monocular and binocular accommodative facility (± 2.00 lenses), negative and
positive relative accommodation, near point of convergence, distance and near
heterophoria (near to be performed at the preferred distance), presence of A-
and V-patterns horizontal fixation disparity/associated phoria at preferred
distance, vergence facility (using 12Δ base-out/3Δ base-in prisms), base-in and
base-out vergence ranges and stereopsis. The visual acuity (VA) was assessed by
crowded Chinese Tumbling E Chart. Imp. Improvement. The corneal light reflex
test, cover-uncover test and alternated cover test were performed to assess the
participants’ ocular alignment. Percentage of respondents (n=30) reporting
symptoms was showed in Table 1 and detailed characteristics of those participants
at the first day visiting was listed in Table 2. The VAs was recorded
before and after 2 month, respectively.
EME
TREATMENT
Daily EME by using Eyespa (model: DF-JY01, Beijing
Tuoda Laser Equipment Co. Ltd. China, produced in 2017; No. of Trademark:
31651609; No. of patents: HK1230002 and CN2018209130 58.9) was performed 3
times/day × 2 months. Eyespa includes a head-mounted virtual reality 3D
spectacle main body having a left eye camera and a right eye camera, and a
shelving board facing the left eye camera and the right eye camera. A control
circuit board is provided on the shelving board. The control circuit board is
provided with a control chip, and a first LED matrix and a second LED matrix
connected with the control chip. The first LED matrix and the second LED
matrix, under the control of the control chip, light up according to a certain
sequence in order to guide eye movements. Furthermore, a first
three-dimensional landscape and a second three-dimensional landscape are
provided in the spectacle main body, respectively facing the left eye camera
and the right eye camera. Eyespa utilizes eye movements
in the 8 compass points, clockwise and anticlockwise rotary movements and
movements for alternating distant and near fields of vision (Figure 1)
to regulate and relax eyes after reading and working in front of computers for
a long time, and to improve coordination ability of eyes, realizing the effects
of preventing myopia, improving vision and relieving visual fatigue. Eyespa can
be widely adapted to a variety of people.
DATA
ANALYSIS
For
each patient, the VA and symptoms were computed and assessed using analysis of
two sample test. All reported P values were two-tailed. SPSS version 22 was
used for analyses.
RESULTS AND DISCUSSION
Amelioration
of DES/CVS and asthenopia
After
2 month Eyespa daily treatment, blurred vision symptom was improved from 97% to
30%; the percentage of difficulty or slowness in refocusing eyes from one
distance to another was reduced from 70% to 33%; irritated or burning eyes were
ameliorated from 37% to 17%; dry eyes were improved from 60% to 20%; eye strain
was ameliorated from 83% to 23%; headache symptom was improved from 7% to 3%;
tired eye was improved from 67% to 30%; sensitivity to bright lights were
reduced from 20% to 13%; eye discomfort was improved from 90% to 27%; and
double vision was reduced from 13% to 0% (Table
1).
Visual acuity
The
outcome examination was completed by 30 (100%) subjects. Visual acuities were
significantly improved from average 0.52 ± 0.18 to 0.88 ± 0.26 decimal
(P=0.001) in right eyes; and from average 0.60 ± 0.21 to 0.93 ± 0.24 decimal
(P=0.004) in left eyes after 2 month Eyespa daily treatment (Table 1).
DISCUSSION
In
this prospective, observational study of 30 children with DES or CVS and
asthenopia aged from 3 to 13 years old, we found that Eyespa treatment improved visual acuities an
average of 0.52 ± 0.18 to 0.88 ± 0.26 decimal in right eyes; and from average
0.60 ± 0.21 to 0.93 ± 0.24 decimal in left eyes after 2 month Eyespa daily
treatment. DES or CVS and asthenopia was ameliorated such as blurred vision
symptom 97% to 30%; difficulty or slowness in refocusing eyes from one distance
to another from 70% to 33%; irritated or burning eyes from 37% to 17%; dry eyes
from 60% to 20%; eye strain 83% to 23%; headache from 7% to 3%; tired eye from
67% to 30%; sensitivity to bright lights from 20% to 13%; eye discomfort from
90% to 27%; and double vision from 13% to 0%. These results demonstrate that
Eyespa therapy is an effective DES or CVS and asthenopia therapy modality,
however, the sample size is not bigger enough. The double-blind clinic study is
performing.
Reports
on the application of EME daily treatment for the management of DES or CVS and
asthenopia have been limited. In most of the reports, blue light-filtering
spectacle lenses [22,23],
lubricating eye drops[24, 25],
correction of refractive error [26,27] the
20-20-20 rule [8], frequent
short breaks [28,29] stimulating an exo-associated phoria [20],
wraparound style of goggles [23] had been
used, but no report of the daily EME treatment improved DES or CVS and
asthenopia have been found according to our limited knowledge. The daily Eyespa
treatment ameliorated DES or CVS and asthenopia by sensory motor function,
however, we did not preclude that this therapy might also affect neuro-sensory
improvements in the visual cortex.
Eyespa utilizes eye movements in the 8 compass
points, clockwise and anticlockwise rotary movements, and movements for
alternating distant and near fields of vision to ameliorate DES or CVS and
asthenopia. With 3D imaging, binocular imaging and overlooking mitigation
technologies, Eyespa can maximize the mobilization of the eyeball in all
directions for enhancing the regulation and relaxation function as well as the
elasticity of lens, restoring the regulation of ciliary muscle and alleviating
visual fatigue.
This
is an era that everyone extensive daily use digital device, even for children.
They use digital device for learning, homework and game purposes as well as
during leisure time normally at school and home. The big challenge is the
prevention for DES or CVS and asthenopia. The strategy for management of DES or
CVS and asthenopia involves ensuring an
ergonomic learning environment [19,30]; patient education; visual examination; eye care;
maintaining normal blinking; using artificial tears; improving contact lens
comfort; using blue light filters; management of accommodation and vergence
anomalies. Currently strategy for management of DES or CVS and asthenopia is
great; and adding to use Eyespa in the strategy afterward is icing on the cake.
CONCLUSION
In the information age, digital devices have brought
convenience to people, but extensive daily usages of digital devices in
children are an impact on systemic and ocular health. Daily usages of Eyespa
would make significant improvements for DES
or CVS and asthenopia.
1.
T.V.C.a.M.
(2016) Eyes overexposed: The digital device dilemma. Digital Eye Strain Report.
2.
Sheppard
AL, Wolffsohn JS (2018) Digital eye strain: Prevalence, measurement and
amelioration. BMJ Open Ophthalmol 3: e000146.
3.
Media,
A.A.o.P.C.o.C.a. (2013) Children, adolescents and the media. Pediatrics 132:
958-961.
4.
Palaiologou
I (2016) Children under five and digital technologies: Implications for early
years pedagogy. Eur Early Childhood Educ Res 24: 5-24.
5.
Wick
B, Hall P (1987) Relation among accommodative facility, lag and amplitude in
elementary school children. Optom Vis Sci 64: 593-598.
6.
Blehm
C, Vishnu S, Khattak A, Mitra S, Yee RW (2005) Computer vision syndrome: A
review. Surv Ophthalmol 50: 253-262.
7.
Dain
SJ, McCarthy AK, Chan-Ling T (1988) Symptoms in VDU Operators. Am J Optom
Physiol Opt 65: 162-167.
8.
Association
A.O. (2017) Computer vision syndrome.
9.
Brennan
CC, Sulley A, Young G (2019) Management of digital eye strain. Clin Exp Optom
102: 18-29.
10.
Rosenfield
M (2016) Computer vision syndrome (a.k.a. digital eye strain). Optom Pract 17:
1-10.
11.
Rosenfield
M, Gurevich R, Wickware E, Lay M (2010) Computer vision syndrome: Accommodative
and vergence facility. J Behav Optom 21: 119-122.
12.
Saito
S, Sotoyama M, Saito S, Taptagaporn S (1994) Physiological indices of visual
fatigue due to VDT operation: Pupillary reflexes and accommodative responses.
Ind Health 32: 57-66.
13.
Courtin
R, Pereira B, Naughton G, Chamoux A, Chiambaretta F, et al. (2016) Prevalence
of dry eye disease in visual display terminal workers: A systematic review and
meta-analysis. BMJ Open Ophthalmol 5: e009675.
14.
(2007)
The epidemiology of dry eye disease: Report of the epidemiology subcommittee of
the international dry eye workshop. Ocular Surface 5: 93-107.
15.
Gowrisankaran
S, Nahar NK, Hayes JR, Sheedy JE (2012) Asthenopia and blink rate under visual
and cognitive loads. Optom Vis Sci 89: 97-104.
16.
Tsuchiya
K, Ukai K, Ishikawa S (1989) A quasistatic study of pupil and accommodation
after-effects following near vision. Ophthalmic Physiol Optics 9: 385-391.
17.
Maeda
E, Yoshikawa T, Hayashi N, Akai H, Hanaoka S, et al. (2011) Radiology
reading-caused fatigue and measurement of eye strain with critical flicker
fusion frequency. Jpn J Radiol 29: 483-487.
18.
Cardona
G, García C, Serés C, Vilaseca M, Gispets J (2011) Blink rate, blink amplitude
and tear film integrity during dynamic visual display terminal tasks. Curr Eye
Res 36: 190-197.
19.
Gray
LS, Gilmartin B, Winn B (2000) Accommodation microfluctuations and pupil size
during sustained viewing of visual display terminals. Ophthalmic Physiol Optics
20: 5-10.
20.
MR
(2011) Computer vision syndrome: A review of ocular causes and potential
treatments. Ophthalmic Physiol Optics 31: 502-515.
21.
Mclean
L, Tingley M, Scott RN, Rickards J (2011) Computer terminal work and the
benefit of microbreaks. Appl Ergon 32: 225-237.
22.
Cheng
HM, Chen ST, Jui LH, Cheng CY (2014) Does blue light filter improve computer
vision syndrome in patients with dry eye? Life Sci J 11: 612-615.
23.
Leung
TW, Li RW, Kee C (2017) Blue-light filtering spectacle lenses: Optical and
clinical performances. PLoS One 12: e0169114.
24.
Acosta
MC, Gallar J, Belmonte C (1999) The influence of eye solutions on blinking and
ocular comfort at rest and during work at video display terminals. Exp Eye Res
68: 663-669.
25.
Gayton
JL (2009) Etiology, prevalence and treatment of dry eye disease. Clin
Ophthalmol 3: 405-412.
26.
Wiggins
NP, Daum KM (1991) Visual discomfort and astigmatic refractive errors in VDT
use. J Am Optom Assoc 62: 680-684.
27.
Wiggins
NP, Daum KM, Snyder CA (1992) Effects of residual astigmatism in contact lens
wear on visual discomfort in VDT use. J Am Optom Assoc 63: 177-181.
28.
Galinsky
T, Swanson N, Sauter S, Dunkin R, Hurrell J, et al. (2007) Supplementary breaks
and stretching exercises for data entry operators: A follow-up field study. Am
J Ind Med 50: 519-527.
29.
Balci
R, Aghazadeh F (2003) The effect of work-rest schedules and type of task on the
discomfort and performance of VDT users. Ergonomics 46: 455-465.
30.
Bohr
PC (2000) Efficacy of office ergonomics education. J Occup Rehab 10: 243-255.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Alcoholism Clinical Research
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Dermatology Clinics and Research (ISSN:2380-5609)