Research Article
Scleral Tuck Lens: Simple and Cost-Effective Solution for Aphakia without Capsular Support
3310
Views & Citations2310
Likes & Shares
Visual rehabilitation in aphakia can be performed using several modalities. However, these modalities can be either technically difficult or expensive. In this study, we developed a scleral tuck lens to provide a simple and cost-effective solution for aphakia.
A specially designed posterior chamber self-sustaining lens was implanted in patients with aphakia without capsular support because of different etiologies. Visual outcomes as well as intraoperative and postoperative complications were examined.
A scleral tuck lens was successfully implanted for 10 eyes, resulting in satisfactory visual outcomes. 7 eyes regained >6/12 and 1 eye 6/60. The anatomically stable lens was placed in the posterior chamber, which is closer to ideal location.
Satisfactory visual outcomes were noted with minimal complications; however, long-term follow-up is required.
Keywords: Scleral tuck lens, Aphakia, Secondary lens implant
INTRODUCTION
Cataracts account for 47% of all cases of blindness worldwide. The epidemiological effect of cataracts is uneven among different countries, and the same is associated with economic conditions. Availability of health care facilities in developing countries, making cataracts a major public health problem and an obstacle to development [1].
Posterior capsular rent is one of the most common complications preventing satisfactory visual outcomes [2].
Rehabilitation of the aphakic eye is a crucial challenge. Aphakia is one of the common problems encountered in patients with trauma. Aphakia can be the end result of complete loss of the lens and capsular support during the trauma itself, or aphakia can be caused by zonular dialysis or lens subluxation beyond a few clock hours in which case capsular support or implantation of the posterior chamber lens can be inadequate. In some cases, performing intracapsular cataract extraction or pars plan lensectomy is required for managing the cataract. In these cases, the only treatment option is the implantation of a secondary lens. Secondary lens implantation can be performed by implanting an intraocular lens (IOL) on the remnant of the capsule, an iris-supported lens, an angle-supported anterior chamber IOL, or a scleral fixated IOL either with sutures, glue, or any other technique [2].
With advances in surgical techniques, the availability of vitrectomy machines in most medical centers, and the ready availability of scleral fixated lenses in the market, the trend is shifting toward implanting a scleral fixated IOL whenever possible.
In some cases, an angle-supported anterior chamber lens is not suitable when patients require a detailed posterior segment evaluation with fully dilated pupils, which is not possible with an angle-supported anterior chamber lens in- situ. This is important because patients with ocular trauma are prone to retinal detachment and require a detailed fundus evaluation with indentation. Furthermore, the use of an angle-supported anterior chamber lens is contraindicated in patients with glaucoma and narrow angles who frequently require gonioscopy, which can be difficult to perform with the haptics of an angle-supported anterior chamber lens in the angle. Associated angle recession can be present in the traumatized eyes, and an angle-supported anterior chamber lens can further aggravate the damage. An angle-supported anterior chamber lens is also not advisable in patients with corneas with low endothelial counts because this lens can lead to corneal decompensation and bullous keratopathy.
The advantage of a scleral fixated lens over an angle-supported anterior chamber lens is its placement in the anatomical location, with the placement being closest to the nodal point of the eye, resulting in favorable optical properties.
Studies have attempted implanting scleral fixated lenses with prolene sutures, iris-supported lenses, and glued lenses; however, the implantation of all these lens types have a long learning curve and is not cost effective [2,3].
In the current study, we designed a self-sustaining lens that does not require any suturing.
METHODS
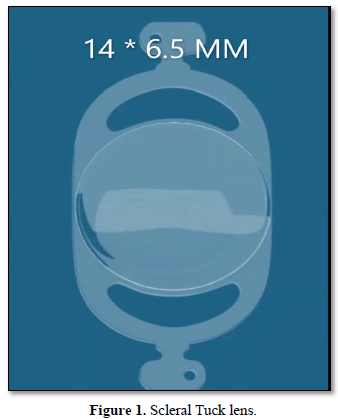
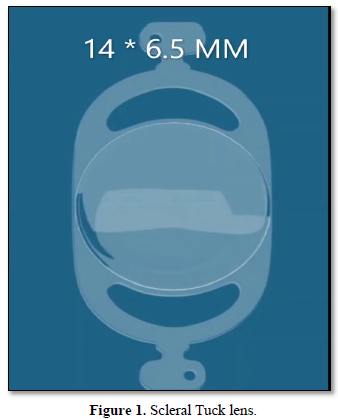
We designed an acrylic foldable lens, which would be suspended with the sclera without using any suture or glue. Figure 1 shows the current lens, having a horizontal size of 14 mm, an optical diameter of 6.5 mm, and acrylic tags connected with main optics with the neck. Tag size is 20 G (0.89 mm) with hole.
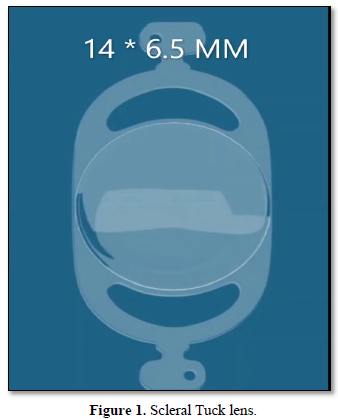
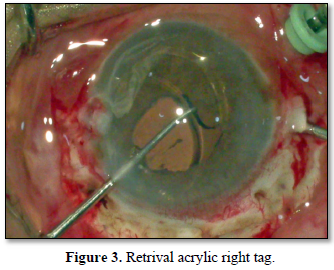
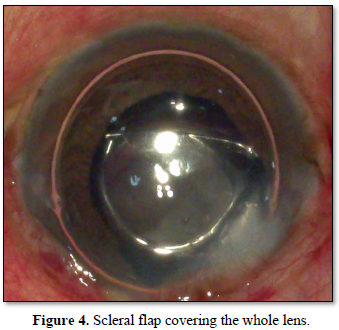
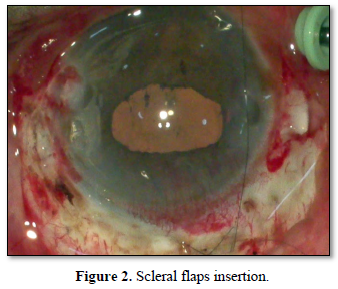
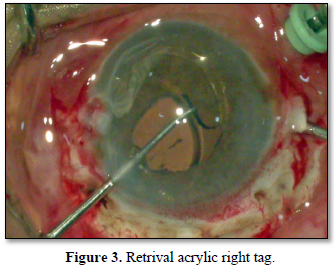
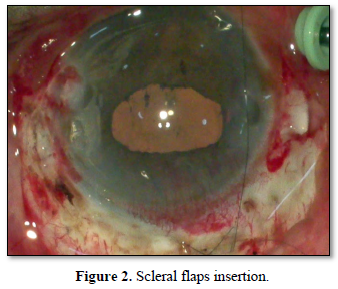
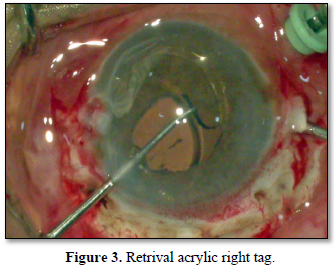
In aphakic eyes, following anterior vitrectomy, scleral flaps were created using a crescent blade after hemostasis. A 23G forceps was used to create an opening under both the flaps. The foldable lens was inserted into the anterior chamber. Then, acrylic tag was handed over by using 23G forceps, the tag was pulled out through the opening on both sides, (Figures 2 and 3) and the posterior chamber self-sustaining scleral fixated lens was implanted in place. The lens tag was covered by the scleral flap (Figure 4).
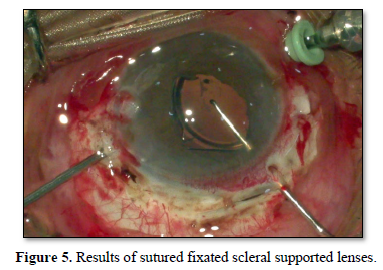
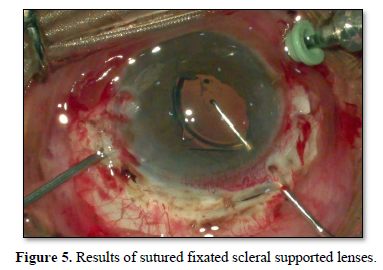
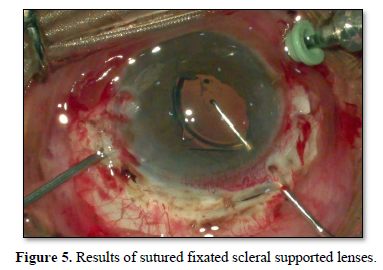
We compared the outcome results of sutured fixated scleral supported lenses according to etiology (Figure 5).


RESULT
Our cohort consisted of 10 eyes out of which 7 were male and 3 were female we performed this procedure in 2 aphakic eyes and eyes with post trauma nucleus drop. On following up, the best corrected visual acuity of the eyes was found to be good. Out of total 6 eyes regained >6/12 and one eye had 6/60 because of co morbidity following trauma.
Until now, no intraoperative or postoperative complications have been noted.
After comparing with suture-supported scleral fixated lens, we did not find a significant difference in the outcome. However, when the outcome was compared according to etiology traumatic or non-traumatic, we found significant difference.
DISCUSSION
Current technique presents a novel design lens for management of aphakia in absence of posterior capsule. We have observed many such studies it will be interesting to compare their results with current lens design.
Thouvenin et al. [3] reported that intracapsular lens implantation has more visual benefits and fewer complications than no implants.
Wood et al. [4] reported that secondary implants in aphakia results in minimal complications and favorable visual outcomes.
Nihalani’s [5] and Ahmadieh’s [6] reported satisfactory outcomes in pediatric aphakia. Dick’s [7] reported many options, such as angle-supported anterior chamber lens or scleral suture-supported posterior chamber IOL, for secondary implants in the absence of capsular support. Shah et al. [2] also reported similar findings. Slade et al. reported good visual outcomes in cases of posterior capsular complication [2,8-11]. Vangelova’s [12] reported good visual outcomes in cases of traumatic cataracts.
David et al. [13] studied the use of an angle-supported anterior chamber lens for long-term effects and suggested serious complications on long-term follow-up [14]. Many studies have reported regarding the use of iris-supported lenses to correct aphakia [15-17]. Other studies have also reported the efficacy of an artificial iris IOL in case of anorexia or traumatic conditions [18-20].
Dadeya’s [21] compared the results of the angle-supported anterior chamber lens and suture-supported scleral fixated lens and found that the angle-supported anterior chamber lens resulted in better outcomes.
Bellucci’s [22] also reported 6% complications in both cases, but more serious complications were found in scleral fixated lenses.
Shah et al. [2] did not find any significant difference if the secondary implant was placed either in the anterior chamber or sulcus following proper vitrectomy.
Lewis’s [23] reported that burying of knots inside the eye is associated with a low incidence of suture erosions. Elfiky’s [24] studied the role of ultrasound bio microscopy as a guide before performing a secondary implant [24].
Recently, many authors have reported promising results with minimal complications when using scleral fixated glued IOLs [25-29].
Kumar et al. [30] conducted a comparative study of various techniques of implanting scleral fixated secondary lenses and found it to be the most effective with minimal complications.
To the best of our knowledge, no study has used the lens design that we used in the current study. The self-retaining scleral supported lens used in the present study has many benefits including a small learning curve, easy to perform technique, and low cost owing to no requirement of glue. Moreover, the incidence of complications is minimal.
CONCLUSION
This novel technique can be useful to manage aphakia in absence of capsular support, Benefits are very cost effective, and it has smaller learning curve it has minimal intra and post-operative complications but needs longer follow up.
VALUE STATEMENT
Current lens has potential to provide perfect solution for optical rehabilitation of aphakia.
What was known
There are many options for scleral fixated lenses available.
This article adds value
This self-retaining lens without any addition suturing or support system, having low learning curve.
- Lawani R, Pommier S, Roux L, Chazalon E, Meyer F (2007) Magnitude and strategies of cataract management in the world. Med Trop (Mars) 67: 644‑650.
- Shah MA, Shreya MA, Upadhyay PKR, Appalwar AH, Gupta AS (2011) Final visual outcome following re-exploration of cataracts performed by trainee surgeons in India. Indian J Med Sci 65(9): 365-370.
- Thouvenin, D, Lesueur L, Arne JL (1995) Intercapsular implantation in the management of cataract in children. Study of 87 cases and comparison to 88 cases without implantation. J Fr Ophtalmol 18(11): 678-687.
- Wood KS, Tadros D, Trivedi RH, Wilson ME (2016) Secondary intraocular lens implantation following infantile cataract surgery: Intraoperative indications, postoperative outcomes. Eye (Lond) 30(9): 1182-1186.
- Nihalani BR, Vanderveen DK (2011) Secondary intraocular lens implantation after pediatric aphakia. J Aapos 15(5): 435-440.
- Ahmadieh H, Javadi MA (2001) Intra-ocular lens implantation in children. Curr Opin Ophthalmol 12(1): 30-34.
- Dick HB, Augustin AJ (2001) Lens implant selection with absence of capsular support. Curr Opin Ophthalmol 12(1): 47-57.
- Turut P (1988) Traumatic cataract and implantation J Fr Ophtalmol 11(5): 425-433.
- Slade JH (1978) Secondary intra-ocular lens implants-ten years’ experience. Adv Ophthalmol 37: 156-158.
- Hayward JM, Noble BA, George N (1990) Secondary intraocular lens implantation: Eight-year experience. Eye (Lond) 4(Pt 4): 548-556.
- Trinavarat A, Neerucha V (2012) Visual outcome after cataract surgery complicated by posterior capsule rupture. J Med Assoc Thai 95 Supp l4: S30-S35.
- Vangelova A (2001) Implantation microsurgery in traumatic cataract. Khirurgiia (Sofiia) 57(5-6): 38-40.
- David R, Yagev R, Schneck M, Briscoe D, Gilad E, et al. (1993) The fate of eyes with anterior chamber intra-ocular lenses. Eur J Ophthalmol 3(1): 42-46.
- Kohnen T, Hengerer FH (2014) Anterior chamber intraocular lenses for aphakia correction. Ophthalmologe 111(4): 310-314.
- Manning S, Lanigan B, Keefe MO (2016) Outcomes after lensectomy for children with Marfan syndrome. J AAPOS 20(3): 247-251.
- Hay A (2014) Secondary iris-fixated intra-ocular lens implantation combined with Pupilloplasty. J Fr Ophtalmol 37(10): 840.
- Zafar SN, Siddiqui SN, Khan A (2013) Effects of Artisan aphakic intraocular lens on central corneal thickness and intra ocular pressure in pediatric eyes with crystalline subluxated lenses. Oman J Ophthalmol 6(1): 44-47.
- Qiu X, Ji Y, Zheng T, Lu Y (2016) The efficacy and complications of black diaphragm intra-ocular lens implantation in patients with congenital aniridia. Acta Ophthalmol 94(5): e340-e344.
- Dong X, Yu B, Xie L (2003) Black diaphragm intraocular lens implantation in aphakic eyes with traumatic aniridia and previous pars plana vitrectomy. J Cataract Refract Surg 29(11): 2168-2173.
- De Grande V, Rosenthal K, Reibaldi M, Gentile RC (2012) Artificial iris-intraocular lens implantation for traumatic aniridia and aphakia assisted by silicone oil retention sutures. J Cataract Refract Surg 38(11): 2045-2048.
- Dadeya S, Kamlesh, Sodhi PK (2003) Secondary intraocular lens (IOL) implantation: Anterior chamber versus scleral fixation long-term comparative evaluation. Eur J Ophthalmol 13(7): 627-633.
- Bellucci R, Pucci V, Morselli S, Bonomi L (1996) Secondary implantation of angle-supported anterior chamber and scleral-fixated posterior chamber intraocular lenses. J Cataract Refract Surg 22(2): 247-252.
- Lewis JS (1993) Sulcus fixation without flaps. Ophthalmol 100(9): 1346-1350.
- Elfiky M, Saad H, Elseht R, Selima A (2015) Role of ultrasound bio microscopy in the planning for secondary implantation of intra ocular lens in aphakia. Int Ophthalmol 36(3): 391-400.
- Jacob S, Kumar DA, Rao NK (2020) Scleral fixation of intraocular lenses. Curr Opin Ophthalmol 31(1): 50-60.
- Verstappen M, Pion B (2019) Pion Glued intraocular lens implantation: A three-year retrospective analysis at two hospitals in Brussels, Belgium. J Fr Ophtalmol 42(9): 962-967.
- Kumar DA, Agarwal A, Packiyalakshmi S, Jacob S, Agarwal A (2013) Complications and visual outcomes after glued foldable intraocular lens implantation in eyes with inadequate capsules. J Cataract Refract Surg 39(8): 1211-1218.
- Narang P, Narang S (2013) Glue-assisted intrascleral fixation of posterior chamber intraocular lens. Indian J Ophthalmol 61(4): 163-167.
- Kumar DA, Agarwal A, Prakash D, Prakash G, Jacob S, et al. (2012) Glued intrascleral fixation of posterior chamber intraocular lens in children. Am J Ophthalmol 153(4): 594-601.
- Kumar S, Singh S, Singh G, Rajwade NS, Bhalerao SA, et al. (2017) Visual outcome and complications of various techniques of secondary intraocular lens. Oman J Ophthalmol 10(3): 198-204.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Alcoholism Clinical Research
- International Journal of AIDS (ISSN: 2644-3023)