994
Views & Citations10
Likes & Shares
One of the most serious problems is that the colon
is a perforation. Frequency of its occurrence fluctuates in wide limits - from
2.3 to 22.3% and postoperative lethality - 23.0-88.9%. A high percentage (up to
60%) of patients with colorectal cancer is hospitalized in an emergency order
due to complications such as intestinal obstruction, tumor perforation,
paracolitic inflammation, intestinal bleeding, anemia. Perforation of a
cancerous tumor is a consequence of the decay and seizure of tumor tissues, which
leads to the development of retroperitoneal phlegmon and sometimes to the
formation of intestinal fistula. Immediate results of surgical treatment,
including methods and means of postoperative complications, as well as delayed
and urgent measures of postoperative complications. Prevention and treatment of
complications associated with severe disorders of the musculoskeletal system.
It should be emphasized that the presence of a suppurative complication of
colon cancer is not a sign of tumor inoperability. Generally accepted standards
regarding the tactics and scope of surgical interventions for limited forms of
colon cancer are not available.
Keywords:
Colon tumor, Complications of cancer, Perforation
INTRODUCTION
One of the
extremely serious complications of a colon tumor is perforation. The frequency
of its occurrence, according to various authors, varies widely - from 2.3 to
22.3% and postoperative mortality reaches 23.0-88.9% [1]. A high percentage (up
to 60%) of patients with colorectal cancer is hospitalized on an emergency
basis due to complications of the disease, such as intestinal obstruction,
tumor perforation, paracolytic inflammation, intestinal bleeding and anemia
[2]. Paracancic inflammatory processes beyond the limits of the intestinal wall
amounted to 22.6%. In 38-76.5%, the tumor with perifocal inflammation was
localized in the right half of the colon [3]. The immediate results of surgical
treatment of patients with a complicated course of colon cancer are directly
dependent on the timely diagnosis of the underlying disease and its
complications, the validity of the surgical tactics, the choice of the method
and technique for performing surgical intervention, as well as the complete
prevention and treatment of postoperative complications [3]. The frequency of
postoperative complications in this category of patients is 31.5% and the
annual mortality rates reach 16.3% [4]. In 6% of patients, the inflammatory
process spread to the abdominal wall with the formation of cellulitis and fecal
fistula. After relief of the inflammatory process, 33.3% of patients routinely
perform traditional surgical interventions [5]. Perforation of a cancer is a
consequence of the disintegration and ulceration of tumor tissue that has
penetrated the entire depth of the intestinal wall, which leads to the
development of retroperitoneal phlegmon, and sometimes the formation of
intestinal fistula. The addition of the inflammatory process significantly
changes and complicates the course of the underlying disease, makes diagnosis
much more difficult and thereby delays the duration of the surgery and limits
the choice of the method of operation. It must be emphasized that the presence
of suppurative complications of colon cancer is not a sign of tumor
inoperability [6].
There are no generally accepted standards for
individual issues regarding tactics and the scope of surgical interventions for
complicated forms of colon cancer [5,7].
CASE STUDY
We present the clinical observation of a
patient with ascending colon cancer, complicated by retroperitoneal perforation
and phlegmon of various localization.
Patient C, 38 years old, 08/09/2016 delivered
to the reception room GBUZ NO “GKB №12” Nizhny Novgorod in a state of shock 3
tbsp. At the time of inspection: the state is extremely difficult, confused
consciousness. The position is passive, on a gurney. Peripheral lymph nodes are
not enlarged. The pharynx is clean, the tongue is dry. Breathing is weakened,
no wheezing, the frequency of respiratory movements 33/min. The skin and
visible mucous membranes pale cyanotic coloration. Heart sounds are muffled,
arrhythmic. Blood pressure 70/30 mm. Hg Art., pulse 110 beats/min, weak
filling. The abdomen is painful and rigid in the right half, the peristalsis is
sharply weakened. The liver, kidney, spleen are not palpated. Symptom of
Pasternack negative on both sides, urination is not difficult.
Locally: in the right lumbar region -
hyperemia, swelling, tenderness over an area of 20 × 15 cm. In the right
gluteal region - a fluctuating formation with skin flushing above it, sharply
painful during palpation, 15 × 15 × 15 cm in size. On the front surface of the
right thigh - hyperemia, swelling, infiltration, palpation tenderness in the
area of 15 × 20 cm. In the right popliteal fossa - fluctuating formation of 8 ×
8 × 8 cm. The right lower extremity is swollen, at the level of the thigh +8
cm, at the level of the tibia +6 cm. On the anterior, lateral and posterior
surfaces of the right the laziness - necrotic modified skin and subcutaneous
tissue over an area of 25 × 30 cm. Procalcitonin test (PCT) -> 2 ng l -
sepsis was diagnosed.
Given the history and objective status of the
diagnosis: cancer of the ascending colon. Perforation in the retroperitoneal
space. Phlegmon of the right lumbar, gluteus, popliteal areas, right thigh and
lower leg. Toxic shock III degree.
08/09/2016 year after preoperative
preparation in the conditions of PIT an emergency operation was performed -
opening of the phlegmon of the right lumbar, gluteus, popliteal areas, right
thigh and lower leg. Opening of phlegmon of the right lumbar region is
supplemented by extraperitoneal access along the right lateral flank of the
abdomen. Received up to 1.2 L of purulent discharge with odor (taken for
planting and determination of antibiotic sensitivity: August 15, 2016,
inoculated with E. cloacae 107 CFU/L,
sensitive to imipenem, amikacin, cefotaxime, ciprofloxacin, pefloxacin).
Separate cuts on the right gluteal region, right thigh, right popliteal fossa
and right lower leg revealed purulent drips (taken for seeding and
determination of sensitivity to antibiotics - 13.08.2016 sown: E. fecium 105 CFU/L, sensitive to
fosfomycin; C. albicans, sensitive to
nystatin). Cavities of wounds are sanitized with a 3% solution of hydrogen
peroxide and made with napkins with levomicol and boric acid. Aseptic
dressings.
Intensive care was performed in the intensive
care unit. Three days after admission, intestinal contents appeared in the
dressings, which supported the inflammatory infection of the soft tissues of
the lumbar region, the anterior abdominal wall and the right lower extremity.
The revealed circumstance required isolation of wounds from intestinal
contents. For this purpose, 7 days after admission, laparotomy was performed.
In the ascending part of the colon, a stony
density infiltrate was found, almost immobile, measuring 20 × 18 × 10 cm,
consisting of the specified section of the colon, retroperitoneal fat, great omentum
and vermiform process. Distant metastases were not detected.
It was decided to isolate the right half of
the colon and the terminal ileum from the passage of intestinal contents
through it, which would prevent it from entering the wounds of the retroperitoneal
space. The performance of right-sided hemicolectomy due to the severity of the
patient’s condition and pronounced inflammatory changes in the area of
operation is currently considered inappropriate. The ileum is crossed and
muffled at 10 cm from the ileocecal angle. The proximal and distal stumps are
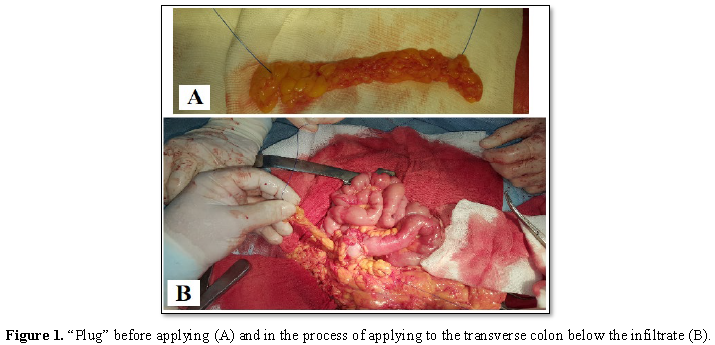
sutured with UKL-40, two half-net and Z-stitches. A “plug” (Figure 1) developed by the authors is applied below the infiltrate
by 15-20 cm onto the transverse colon, which excludes ischemia of the intestinal
wall and possible subsequent migration of the anti-reflux construct into the
intestinal lumen, which is observed during the formation of the “plug”
according to Shalimov (Patent number RF 2253379).
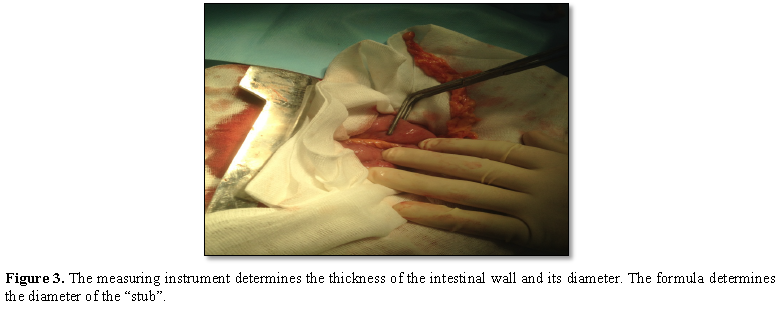
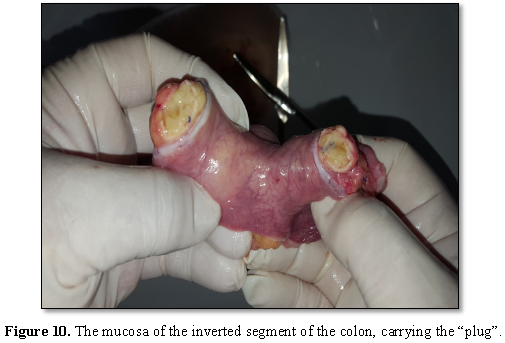
For the formation of the "plug"
according to the developed method, the thickness of the intestinal wall (d),
the diameter of the section of the intestine (D1), on which the implementation
of the “plug” is planned, is determined. When obtaining the desired parameters
using the formula D2=2√D1d, the required diameter of the corrugated part of the
small intestine (D2) is calculated. For intraoperative measurement of tissue
parameters in millimeters, as well as to control the circumference of the ring
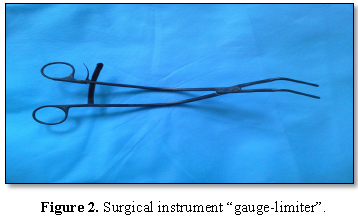
during its formation, we use a surgical instrument “gauge-limiter” (Figures 2 and 3).
With the help of a semicircular ruler
installed on the branches and fixed with a notched lock, the tool can measure
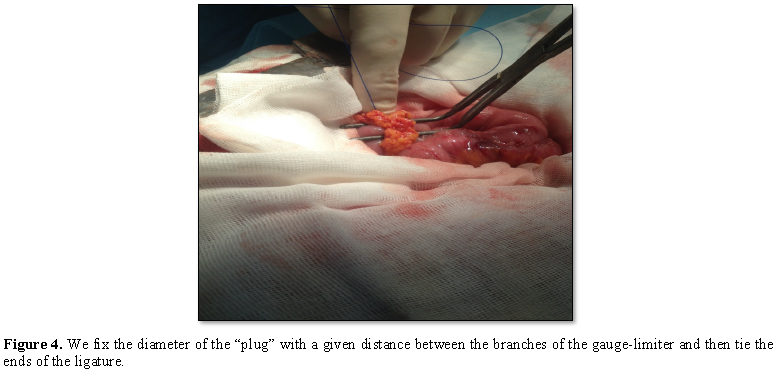
and fix the distance between the working surfaces. This feature allows on the
working surfaces to bind the ends of the ligature-omental tape and, thus, to
form a skeleton ring of a given circumference (Figure 4).
The data of the scientific calculation
substantiate the practical execution of the operation: the intestinal
antipyretic wall is brought closer to the mesenteric, the established situation
is fixed by 2-4 nodal sero-muscular sutures, on top of which a developed “cap”
is formed, tying the ends of the ligature.
At 10 cm below the “plug”, an isoperistaltic
two-row ileo-transverselyanastamose side to side is formed (Figure 5).
Catching drainage in the pelvis. Control of
hemostasis. Layer wound seam. Aseptic dressing. Sanitation of wounds, excision
of necrotic tissue of wounds of the right lumbar region, thigh, tibia to viable
tissues. Open flowed in the upper third of the inner surface of the right
thigh. From the moment of receipt of 09/08/2016 to 08/28/2016 (postponed the
opening of the abscesses, the first laparotomy) he received a course of antibiotic
therapy with ceftriaxone, meropenem, abactal and metrogylism.
According to the subsidence of the
inflammation of soft tissues 60 days after admission to the hospital on
10/06/2016, a second laparotomy was performed to remove a colon tumor — a
midline laparotomy with excision of the postoperative scar. Granulomas with
purulent contents are determined in the subcutaneous tissue - pus is taken for
seeding (10.10.2016 - the etiologically significant aerobic bacterial
microflora was not detected). Pronounced adhesions in the abdominal cavity. Viscerolysis.
A revision of the abdominal organs revealed a tumor of the ascending part of
the colon with a diameter of up to 10 cm.
The ileal stump is up to 12 cm in length, the
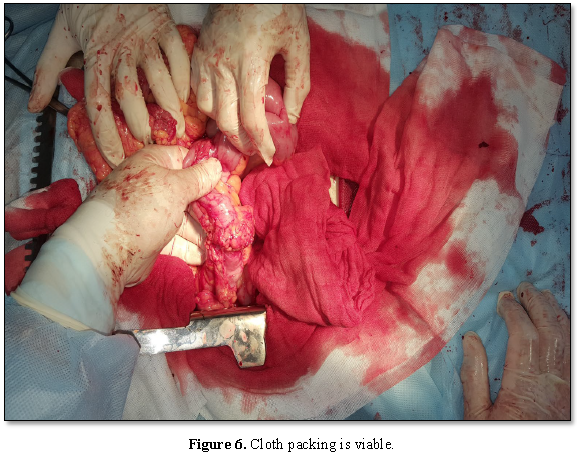
ileotransverse anastomosis is 3.5 cm in diameter. The “cap” is 10–9
cm above the anastomosis on the colon, viable: the great omentum tissue is
moderately infiltrated, pink; the peritoneum is shiny (Figure 6). The section of the right half of the colon without
intestinal contents - the “plug” has fulfilled its isolating function.
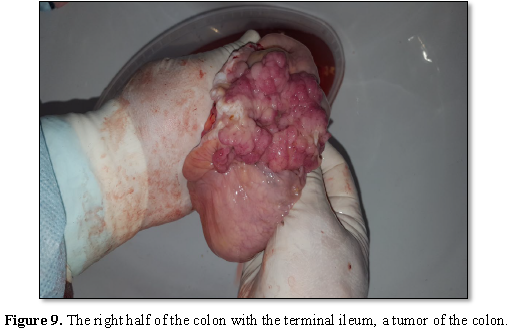
Produced mobilization of the right half of
the colon with a segment of the ileum. From the back wall of the ascending
colon with a tumor to the tissues of the lumbar region there is a dense
cicatricial cord - a consequence of a fistula from this section of the
intestine to the lumbar region. Cicatricial cord is crossed, the lumen in the
severity is not revealed. Performed right hemicolectomy. The stump of the colon
sutured apparatus UO-60, peritonized with two half-net stitches.
To make the ileotransverse anastomosis
arefluxic around the small and large intestine proximal to the 3 cm
anastomosis, a ring is formed from the free portion of the greater omentum (Figure 7) with a nonabsorbable
vikrilovy ligature passed through it (RF Patent No. 2253390).
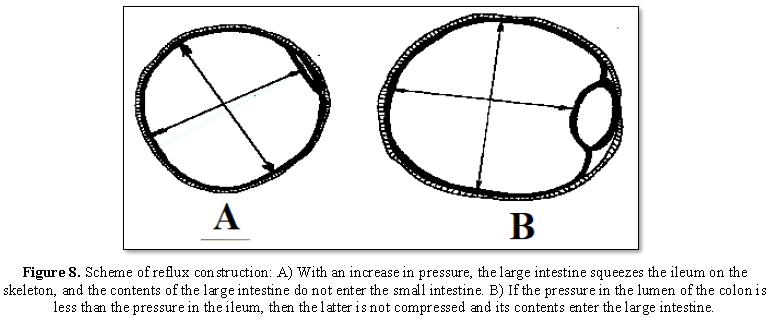
The principles of functioning of the reflux
structure are reflected in Figure 8.
Through contraceptives to the stump of the
large intestine and in the small pelvis 2 trapping drainage were placed. Layer
wound seam. Aseptic dressing.
The drug: 1. The right half of the colon with
a terminal
In the ascending part, there is a tumor up to
Preparation
After hemicolectomy, a course of cefazolin
was conducted from 10.10.2016 to 10.24.2016. 10/20/2016 - skin plastics.
Histological examination of the right half of
the colon No. 10135/45 of 10/13/2016: in the preparation a picture of an
adenomatous polyp with areas of malignancy with the transition to a highly
differentiated adenocarcinoma. Within the limits of resection of tumor growth
no.
Histological examination of the area of the
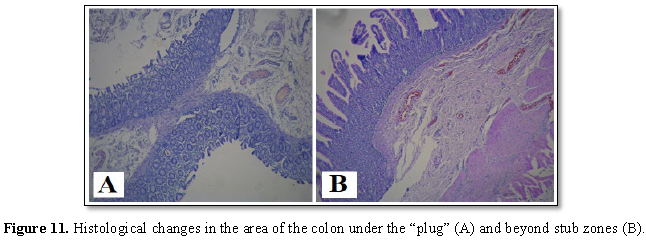
colon outside the zone of “plug” No. 10147/58 dated October 13, 2016 (Figure 11B). Coloring
hematoxylin-eosin. Increase X100. Fragment of the large intestine mucosa with
signs of atrophy of the glands, moderate lymphoid infiltration, edema and
plethora in the submucosal layer, pronounced focal fibrosis of the muscle plate
and moderate lymphocytic infiltration.
Histological examination of the area of the
colon under the “plug” № 10146/50 from 10/13/2016 (Figure 11A). Coloring hematoxylin-eosin. Increase X100. Mucosa
with moderate lymphocytic infiltration and atrophy of the glands. Submucous and
muscular membranes with edema and plethora with weak leukocyte infiltration,
the growth of fibrous tissue is noted in the serous membrane, which proves the
viability of the colon wall under the “plug”.
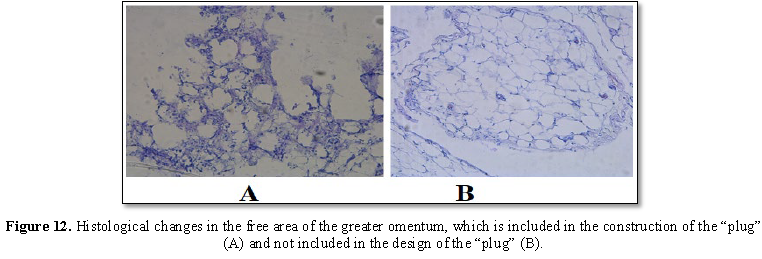
Histological examination of the site of the
great omentum, which is not included in the construction of the “plug”, No.
10159/62 dated October 13, 2016 (Figure
12B). Hematoxylin-eosin staining. Increase X100. Fragment of adipose tissue
of the usual histological structure.
Histological examination of the free area of
the gland included in the construction of the “plug”, No. 10155/58 dated
October 13, 2016 (Figure
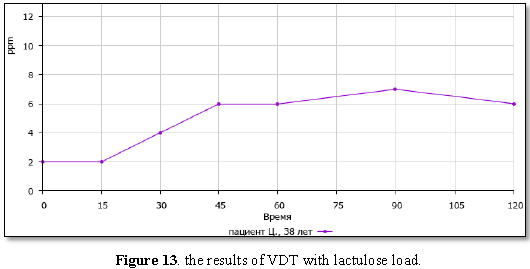
After the second
laparotomy, he has undergone a course of ceftriaxone and metrogil. After 2
months, a hydrogen respiratory test (VDT) with lactulose load was not performed.
The results of the VDT correspond to normal values - the bacterial growth
syndrome (SIBO) is not diagnosed (Figure
13).
A patient with granulating wounds was
performing a skin grating (Figure 14).
FINDINGS
1. When
colon cancer is complicated by perforation into the retroperitoneal tissue and
purulent processes, it is necessary to isolate the soft tissues from the
intestinal contents, for which purpose it is advisable to use the “plug” on the
large intestine that does not cause its ischemia.
2. The
free area of the greater omentum on the gut, the section of the intestine
included in the construction of the “plug” retains its viability.
3. The
developed methods of creating a “plug” on the intestine and a refluxal
small-colonic anastomosis are widely available, safe and adequately provide
their intended functions.
4. The
formation of the developed a reflux small intestinal anastomosis is appropriate
for the prevention of excess bacterial growth syndrome in the small intestine,
as evidenced by the results of VDT with lactulose load.
1.
Pakhomova GV, Podlovchenko TG, Uteshev NS, Selina I E
(2009) Neotlozhnaya khirurgiya raka obodochnoy kishki. (Emergency surgery of
Colon cancer) M: Miklos, p: 96.
2.
Coco C, Verbo A, Manno A, Mattana C, Covino M, et al.
(2005) Impact of emergency surgery in the outcome of rectal and left colon
carcinoma. World J Surg 29: 1458-1464.
3.
Merkel S, Meyer C, Paradopoulos T, Meyer T, Hohenberger W
(2007) Urgent surgery in colon carcinoma. Zetrabl Chir 132: 16-25.
4.
Davydov MI, Aksel EM (2012) Statistics of malignant
neoplasms in Russia and the CIS countries in 2009. Vestnik RONTS im. N.N.
Blokhina RAMN 3: 172.
5.
Shevchenko Yu L, Stoyko Yu M, Levchuk AL (2011)
Combination of complicated forms of colon cancer: A clinic, diagnostics,
surgical tactics. Vesnik Exp Clin Surg 6: 641-646.
6.
Blackham AU, Sweet K, Levine EA, Shen P (2013) Surgical
management of colorectal cancer metastases to the liver: Multi-modality
approach and a single institutional experience. Colorectal Cancer 2: 73-88.
7.
Shaeva SN (2015) Colorectal cancer complicated by
perforation. Features of surgical tactics. Oncol Coloproctol 5: 38-41.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- BioMed Research Journal (ISSN:2578-8892)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Pathology and Toxicology Research
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)