Research Article
Caesarean Section in a Referral Hospital in Sub-Saharan Africa: Frequency and Evaluation according to the Robson Classification
215
Views & Citations10
Likes & Shares
Introduction: The WHO recommends the Robson classification in all maternity wards in order to serve as a global and standard model to better appreciate the practice of caesarean section around the world.
Objective: Study the frequency, indications, the Robson groups most likely to provide caesarean sections and, maternal and perinatal complications.
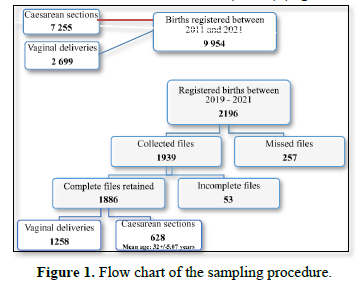
Materials and Methods: This was a retrospective descriptive and analytical study carried out at the Douala General Hospital from January 1, 2011 to December 31, 2021. The SPSS software version 23, the odds ratio at a confidence interval of 95% and a p value
Results: The frequency of caesarean sections is increasing at the Douala General Hospital. It increased from 18.41% in 2011 to 32.49% in 2021, with an average of 27.92%. The main indications for caesarean section were: fetal distress, elective caesarean sections and severe preeclampsia. Group 5 was the first provider of caesarean sections (28.50%), followed by group 10 (17.04%) and group 2 (11.78%). Belonging to groups 5, 10 and 2 significantly increased the risk of caesarean section by 10 times (OR: 10.28; 95% CI [6.90-15.32]; p = 0.001), 4 times (OR = 4.425; 95% CI [2.97-6.58]; p=0.001) and 2 times (OR=2.704; 95% CI [1.68-4.34]; p=0.001) respectively. Maternal and perinatal complications were mainly intra-operative hemorrhage (1.43%), postpartum hemorrhage (0.95%), postpartum anemia (1.43) and fetal asphyxia (7.16%); maternal and perinatal deaths (0.47% and 3.34%) were observed in groups 10, 8 and 5.
Conclusion: The frequency of caesarean sections is increasing at the Douala General Hospital; groups (Robson) 5, 10 and 2 are the most affected. Maternal and fetal deaths are observed in groups 10, 8 and 5.
Keywords: Caesarean section, Frequency, Indications, Robson classification, Complications, Douala General Hospital
INTRODUCTION
Caesarean section (CS) is the artificial delivery of a new-born by abdominal wall surgical incision to remove a new-born from the maternal uterus [1]. While in 2015, the World Health Organization (WHO) estimated that only 10-15% of all births require a caesarean section [2], the global caesarean section rate has risen from 12% in 2000 to almost 21.1% in 2018 [3]. In Cameroon, according to the 2018 Demographic and Health Survey report, between 1991 and 2018, the percentage of births by caesarean section has slightly changed: 2.3% in 1991, 2.0% in 2004, 3.8% in 2011 and 3.5% in 2018, with the highest frequency recorded in the city of Douala (11%) [4]. At the Douala General Hospital (DGH), between January 2000 and December 2007, Nguefack [5] found a caesarean section frequency of 13.25% with the main complications being intra and post-operative hemorrhage [5]. Controlling the caesarean section rate is a major concern in the obstetrical field given the risk of morbidity and mortality associated with this practice [6,7]. In 2017, the WHO proposed to implement the Robson classification in all maternity units and use it as a global standard to assess, monitor and compare caesarean section rates [8]. The Robson system classifies all women into 10 mutually exclusive categories that form a comprehensive set. These categories are based on five basic obstetric parameters: parity, onset of labor, gestational age, presentation and number of fetuses [9]. The Robson system criteria are widely used in developed countries, as well as in many health facilities around the world. In sub-Saharan Africa, this classification is gradually considered.
OBJECTIVE
To assess the frequency and indications of CS, the Robson’s group most likely to experience CS and, the maternal and perinatal complications.
MATERIALS AND METHODS
This was a cross sectional study conducted at the DGH, over a 10-year period from 1 January 2011 to 31 December 2021. Women who delivered in the hospital and whose records allowed them to be classified in one of the ten groups of the Robson classification were included in this study.
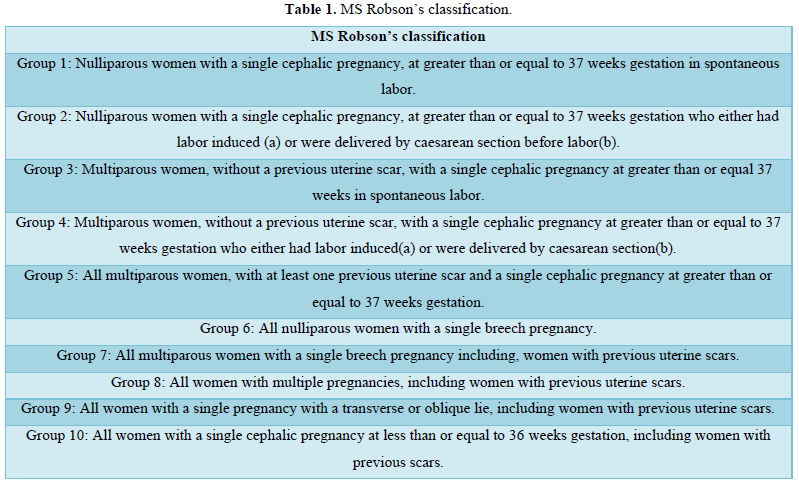
Data were collected from records of the department of Mother and child. using a pre-tested data collection sheet. Sociodemographic data, obstetrical characteristics, indications of CS, mode of admission and maternal and fetal prognosis were collected. Only files collected from 2019 to 2021 were used for Robson’s Classification, meanwhile records from 2011 to 2018 were used for CS rate calculation. Files with at least 95% of the expected information were considered as complete, whereas those with less than 95% were incomplete. Each patient was then classified into one of the ten groups of the Robson classification (Table 1) [9]. Data were analyzed using SPSS software version 26.0. Qualitative data were expressed as numbers and percentages, meanwhile quantitative data as means and standard deviations; Odds ratios with a confidence interval at 95% was used for analytical statistics with a p value was set at 0.05.
RESULTS
- CPD: cephalopelvic disproportion
- Elective caesarean section: it concerns: - Persistence of the indication for the first caesarean section - History of at least 2 caesarean sections - History of uterine rupture - History of surgical myomectomies (group 2b) - Thin lower segment.
- IFV: In vitro fertilization
- TOLAC: Trial of labor after CS
- The main indications for caesarean sections at the DGH were fetal asphyxia (24.20%) followed by, elective CS (22.13%), and severe preeclampsia (9.55%) (Figure 1 & Tables 2 & 3).
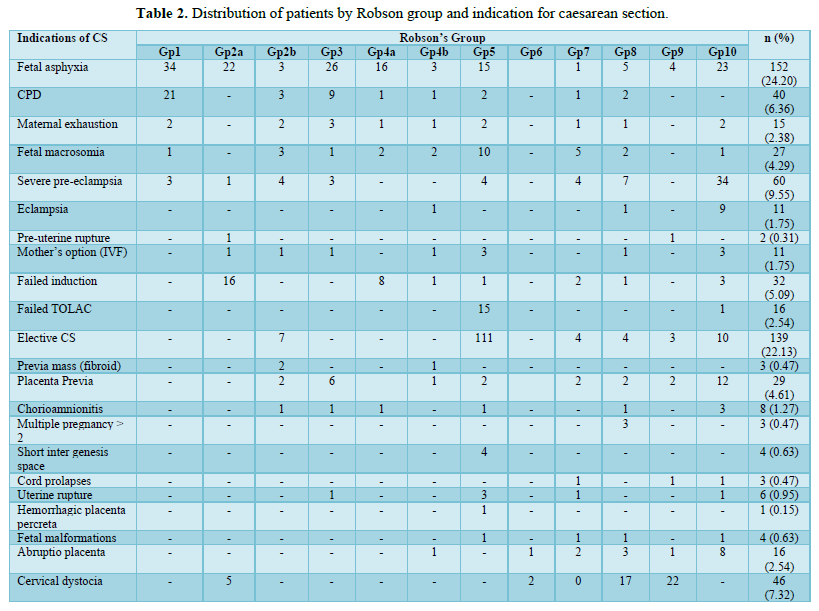
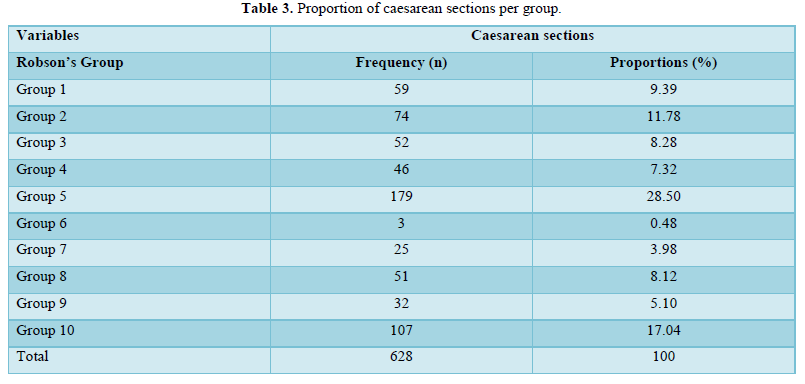
The 03 first groups with the higher CS were group 5 (28.50%), group10 (17.04%) and group 2 (11.78%) (Table 4).
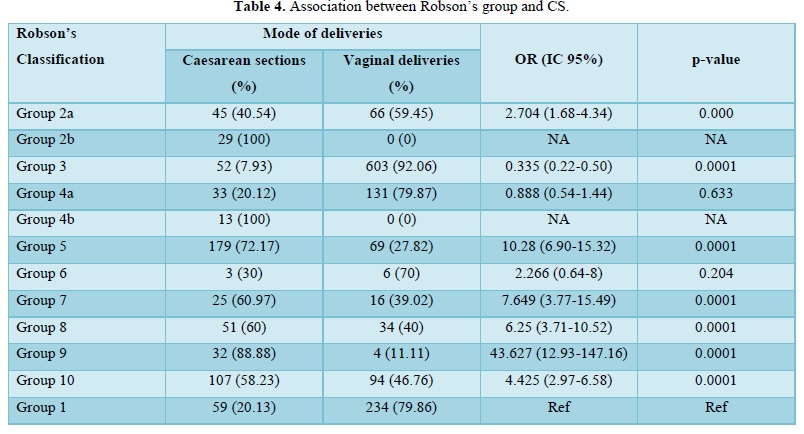
Belonging to Robson's groups 5, 10 and 2 significantly increased the risk of caesarean section by 10 (OR: 10.28; 95% CI [6.90-15.32]; p=0.0001), 4 (OR=4.425; 95% CI [2.97-6.58]; p=0.0001) and 2 times (OR=2.704; 95% CI [1.68-4.34]; p=0.0001) respectively (Table 5).
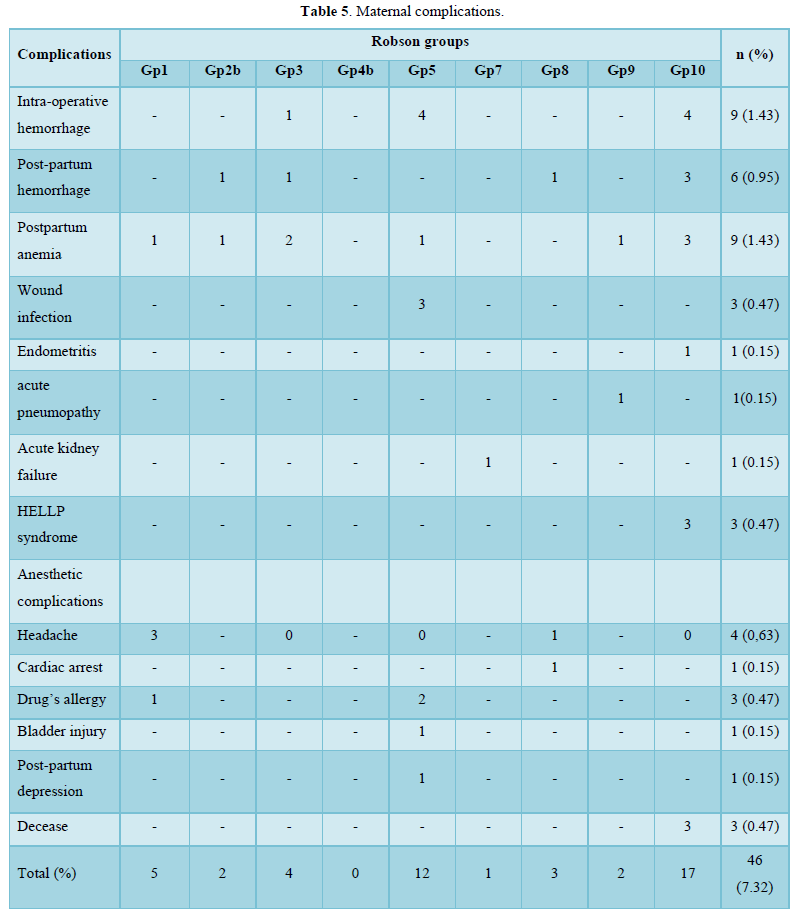
Intra-operative hemorrhage (1.43%), postpartum hemorrhage (0.95%) and postpartum anemia (1.43%) were the main maternal complications. Maternal complications were observed mainly in group 10 (2.70 %) and group 5 (1.91 %) (Table 6).
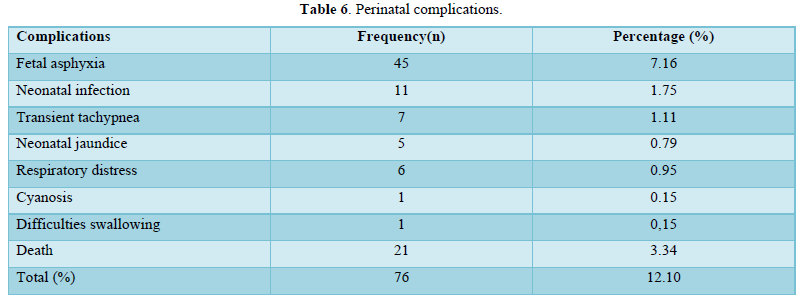
Fetal asphyxia was the main perinatal complication (7,16%).
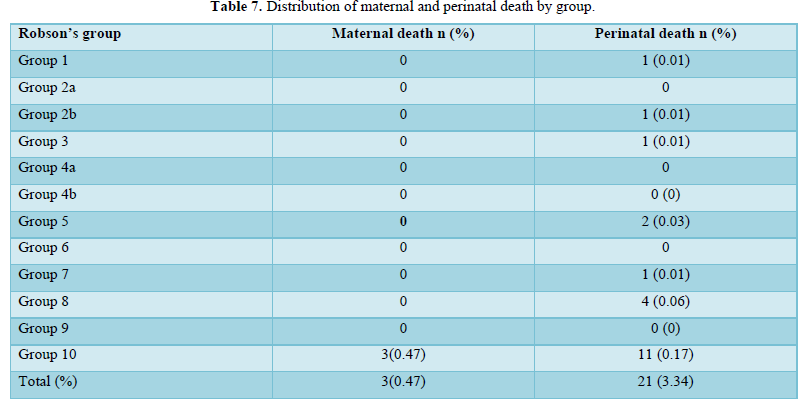
Perinatal death was 3.34%, most frequent in Robson's group 10 (0.17%) and group 8 (0.06 %). Maternal death was 0.47%, only in group 10 (Table 7).
DISCUSSION
The frequency of CS has increased considerably at the DGH, doubling the maximum threshold of 15% prescribed by the WHO. It increased from 18.41% in 2011 to 32.49% in 2021, with an average of 27.92%. (Figure 2). This CS frequency is close to that found in other referral hospitals [10,12] and high compared to the 11% frequency reported in the city of Douala in 2018 [4]. This could be explained by the fact that our study was unicentric; therefore, categories of hospitals that could not perform high-risk deliveries were not taken into consideration. Moreover, the DGH is a referral center that manages most high-risk pregnancies in the city of Douala and its surroundings, thus which usually result in a CS. Between 2019 and 2021, the average age of women who underwent caesarean section was 32.5±5.05 years, range16 to 50 years. This average age is slightly higher than that found by some authors in sub-Saharan Africa [12,14]. The pronatalist culture of sub-Saharan population could explain this situation with pregnancies in advance ages either spontaneously or by medically assisted procreation. The main indications of CS were fetal asphyxia (24.20%), elective CS (22.13%) and severe preeclampsia (9.55%). These findings are in accordance with the results of the demographic survey in Cameroon [4]. The Robson 5 group was the leading provider of caesarean sections (28.50%) (Table 3). The second provider was group 10 (17.04%) and the third was group 2 (11.78%). Those pertaining to Robson's groups 5, 10 and 2 had a significantly increased risk of caesarean section by 10, 4 and 2 times respectively (table III). Maternal and perinatal complications were 7.32% (mainly due to intra-operative hemorrhage, postpartum hemorrhage and postpartum anemia) and 12.10 % (mainly due to fetal asphyxia) respectively (Tables 5 & 6). Group 10 had the highest maternal and fetal complications. These results are similar to those of 15. Sugianto [15] in Indonesia and Tchantchou [16] in Gabon and different from those of developed countries where group 10 is among the least providers of caesarean sections [17-20]. The rate of maternal death (0.47%) was less than that of perinatal death (3.34%) (Table 7). Two cases of maternal death resulted from complications of coagulopathy on placenta abruptio. One case was a cardiac arrest on a uterine rupture with a delaiance in referral. The delaiance in referral was also observed in 60.20% of cases of fetal asphyxia. Emergency medical services with pre-hospital care remain poorly developed in sub-Saharan Africa and the developing world at large. The provision of timely treatment during life-threatening emergencies is still lacking. The main causes of perinatal death were fetal asphyxia and neonatal infection. Most of these deaths were in Robson's groups 8 and 10; making thus the poor prognosis groups. The death rates found in this study were similar to other studies done in sub-Saharan Africa: Essiben [12] reported maternal and early neonatal death of 0.49% and 5.69% respectively, while Kinenkinda [21] found 1.4% and 7.07% respectively. All our findings in this study are still raising out the necessity to urgently tackle, but efficiently, the issue of maternal and perinatal mortality and morbidity which are so far a main concern in our midst.
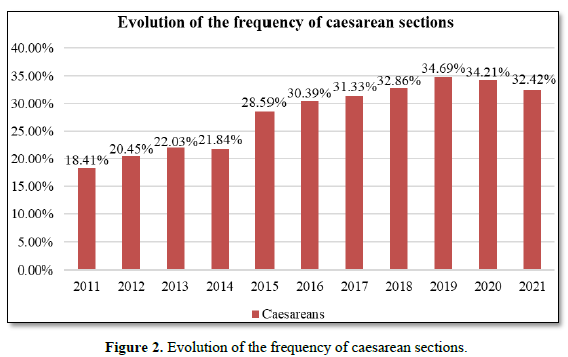
There is an overall increase rate of CS at the DGH from 2011 to 2021, with an overall average of 27.92%.
CONCLUSION
The frequency of CS is increasing at the DGH. Fetal asphyxia, elective caesarean sections and severe preeclampsia are the main indications. Robson's groups 5, 10 and 2 are the most frequent providers of this CS. Maternal and perinatal complications are mainly intra-operative hemorrhage, postpartum hemorrhage, postpartum anemia and fetal asphyxia. Maternal and perinatal death are mainly observed in groups 10, 8 and 5.
LIMITATION OF THE STUDY
We could not exploit entirely files from 2011 to 2018 because they were incomplete.
STRENGTH OF THE STUDY
-
It permits us to have the real CS figure in our setting
-
It is among the first to evaluate CS on Robson’s classification basis, in our settings.
- Larousse É (2022) Césarienne. Larousse [En ligne].
- World Health Organization (2015) Statement on Caesarean Section Rates. Geneva.
- Boerma T, Ronsmans C, Melesse DY, Barros AJD, Barros FC, et al. (2018) Global epidemiology of use of and disparities in caesarean sections. Lancet 392: 1341-1348.
- Institut National de la Statistique (INS) et ICF. (2018) Enquête Démographique et de Santé du Cameroun. Yaoundé, Cameroun et Rockville, Maryland, USA: INS et ICF pp: 167-179.
- Nguefack CT, Priso EB, Njamen TN, Bilkissou M, Ekane GH, et al. (2012) L’accouchement par césarienne à l’Hopital Général de Douala: Incidence, indications et complications. Revue de Médecine et de Pharmacie 2: 2.
- Biccard BM, Madiba TE, Kluyts HL, Munlemvo DM, Madzimbamuto FD, et al. (2018) Perioperative patient outcomes in the African Surgical Outcomes Study: A 7-day prospective observational cohort study. Lancet 391(10130): 1589-1598.
- Keag OE, Norman JE, Stock SJ (2018) Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. PLoS Med 15(1): 22.
- World Health Organization (2017) Robson Classification: Implementation Manual. Geneva.
- Robson MS (2001) Classification of caesarean sections. Fetal Matern Med Rev 12: 23-39.
- Manseur F, Lachmat A, Krouk Y, Oukid MS (2020) Indications of Caesarean section, Interest in Robson’s classification. J Funct Mater Biomol 6: 1-2.
- Foumane P, Koh V, Minkande J, Ngantcha E, Sama DJ, Mboudou E (2014) Risk factors and prognosis of emergency cesarean delivery at the Yaoundé Women’s and Children’s Hospital, Cameroon. Med Sante Trop 24: 1.
- Essiben F, Belinga E, Ndoua CN, Moukouri G, Eman MM, et al. (2020) La Césarienne en Milieu à Ressources Limitées: Évolution de la Fréquence, des Indications et du Pronostic à Dix Ans d’Intervalle. Health Sci Dis 21(2): 7.
- Tura AK, Pijpers O, de Man M, Cleveringa M, Koopmans I, et al. (2018) Analysis of caesarean sections using Robson 10-group classification system in a university hospital in eastern Ethiopia: A cross-sectional study. BMJ 8(4): e020520.
- Kone Nana Aminata. Les accouchements par césarienne selon la classification de Robson au Centre de santé de référence de la Commune V de Bamako (MALI) (2021) Thèse de Médecine: Université des Sciences, des Techniques et des Technologies de Bamako.
- Sugianto, Kusuma AANJ, Suwardewa TGA, Adnyana IBP, Surya IGNHW (2022) Caesarean Section Characteristics Based on Robson Classification at Sanglah Hospital. Eur J Med Health Sci 4(1): 97-102.
- Tchantchou TDD, Ngou MN, Ole S, Ntamack JAB, Mpiga E, et al. (2019) Césarienne à l’Hôpital d'Instruction des Armées Omar Bongo Ondimba. Analyse selon la classification de Robson. Bull Méd Owendo 17(46): 43-47.
- Zeitlin J, Durox M, Macfarlane A, Alexander S, Heller G, et al. (2021) Using Robson’s Ten‐Group Classification System for comparing caesarean section rates in Europe: An analysis of routine data from the Euro‐Peristat study. BJOG Int J Obstet Gynaecol 128(9): 1444‑1453.
- Hehir MP, Ananth CV, Siddiq Z, Flood K, Friedman AM, et al. (2018) Cesarean delivery in the United States 2005 through 2014: a population-based analysis using the Robson 10-group classification system. Am J Obstet Gynecol 219: 105 e1-11.
- Bracic T, Pfniß I, Taumberger N, Kutllovci-Hasani K, Ulrich D, et al. (2020) A 10-year comparative study of caesarean deliveries using the Robson 10 group classification system in a university hospital in Austria. PLoS One 15(10): e0240475.
- Vila-Candel R, Martín A, Escuriet R, Castro-Sánchez E (2020) Analysis of Caesarean Section Rates Using the Robson Classification System at a University Hospital in Spain. Int J Environ Res Public Health 17: 1575.
- Kinenkinda X, Mukuku O, Chenge F, Kakudji P, Banzulu P, et al. (2017) Césarienne à Lubumbashi, République Démocratique du Congo I: fréquence, indications et mortalité maternelle et périnatale. Pan Afr Med J 27: 72.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Journal of Rheumatology Research (ISSN:2641-6999)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Allergy Research (ISSN:2642-326X)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)



