Research Article
The Doctrine of the Nobel Prize Laureate I.I. Mechnikov On Chronic Autointoxication and Premature Aging. is Not the Reason for these Processes in the Failure of the Bauhinia Damper?
1312
Views & Citations312
Likes & Shares
Nobel laureate I.I. Mechnikov: “The causes of natural death are the self-poisoning of the organism coming from the intestines. Physiological sclerosis is a consequence of prolonged poisoning with poisons arising in the colon”.
But I.I. Mechnikov did not indicate the path of development and implementation of chronic autointoxication.
In our opinion, this is the failure of the Bauhinia damper (NBZ). We present our data on chronic autointoxication in NBZ and after its surgical correction.
Keywords: Natural death, Chronic autointoxication, Bauhinia damper
ANNOTATION
The theory of the Nobel laureate I.I. Mechnikov. It was revealed that a person dies earlier than the deadline set by nature, which is due to chronic autointoxication emanating from the large intestine. Based on the analysis of 500 operated patients, the author draws a conclusion that the theory of I.I. Mechnikov is realized through the failure of the Bauhinia valve (NBZ), through the development of the syndrome of excessive bacterial growth in the small intestine. Surgical correction of NBZ stops pathological processes, which is a promising gerontological direction.
When Pasteur made his great discovery of the microbe of lactic acid fermentation in 1857, he at the same time noticed that this organism, although it produces lactic acid itself, suffers from its excess, which leads to the death of the microbe. This death can be attributed to natural death. The latter occurs as a result of self-poisoning, i.e., poisoning by the products of the physiological activity of the microbe itself.
The death of old people is often described as natural, but in the vast majority of cases it depends either on infectious diseases or on apoplectic strokes. Real natural death should be extremely rare in humans. It is likely that natural death, its cause - self-poisoning of the body [1,2].
I subscribe to the opinion of Oscar Bloch, who questions the existence of natural death in humans [1,2]. Some giant cells (macrophages) in senile bones absorb bone matter, bone plates, others destroy hair pigment, and still others absorb muscle contractile matter. The activity of intestinal microbes causes the thickening of the walls of arterial vessels, the development of atherosclerosis. Atherosclerosis, in turn, causes a special disease, sclerosis of the most important organs (liver, kidneys, etc.).
Excreted in the intestine, phenol and carbolic acid produce a chronic change in the arterial walls with all the consequences. This has been proven. In the brain, these cells destroy the noblest elements of our body. The phenomena of neuronophagy are well known in the pathological histology of nerve centers. They are usually observed with nervous diseases and intoxication. These phenomena are also common in the brains of old people and old mammals. All intermediate stages between the presence of a typical nerve cell and its complete disappearance do not allow us to doubt that we are dealing with intense phagocytosis. This phagocytosis consists in the gradual transition of the contents of the nerve cell into the surrounding neuronophages. In the kidneys and liver, there are whole clusters of macrophages that consume the secretory cells of these organs, thereby leading to serious atrophy. Having destroyed the noble elements of the aged organism, macrophages, having formed connective tissue, never again give way to the disappeared noble elements. This is how sclerosis is formed in old people, the reason for our premature wilting. The deeper you get to know the nature of diseases, the more you become convinced of their great similarity with atrophic phenomena that occur in old age. Since the mechanism of senile atrophy is completely similar to the mechanism of atrophy of microbial and toxic origin, the question arises whether there is an interference of microbes and their toxins in old age? Isn't the overexcited state of macrophages due to some kind of poisons developed deep in our body? The main source of our poisons is well known. Our digestive canal contains a huge number of microbes, many of which are capable of secreting substances that are more or less poisonous. Along with acute poisoning, the microbes of the intestinal cavity can cause chronic inflammation by prolonged release of their wastes. It is in these microbial wastes that one should look for the reason for the weakening of the noble elements of our body and the development of the destructive activity of macrophages [1,2].
If, indeed, intestinal microbes are the sources of senile atrophy, then the less the intestinal microbial flora is developed, the less pronounced the phenomena of old age will be.
Birds live much longer than most mammals, the intestinal flora of birds is distinguished by an incomparably lower content of microbes than the flora of mammals. Having almost no large intestine, birds are deprived of that large container of food waste, which in mammals feeds a lot of microbes. Turtles and crocodiles live to a ripe old age without showing any external signs. The large intestine of birds, turtles, crocodiles is very little developed, if not absent at all, and their intestinal flora is extremely poor. The life span of animals is the more significant, the shorter their colon.
This gives us the right to confirm the hypothesis about the role of intestinal microbes as one of the most important causes of the chronic disease, which is our old age. People do not live out their life cycle. Intestinal poisons, being secreted by bacteria in the intestinal canal, are easily absorbed into the bloodstream and spread throughout the body. Their number is too small to cause acute poisoning, but sufficient to produce chronic organ changes. Their action accumulates gradually over months and years, the body wears out, since there are no antidotes. They are rendered harmless to some extent in the liver, but not enough to lose their chronic harmful effects. This manifests itself in the form of changes in organs similar to those characteristics of old age. This conclusion was obtained by experiments on various animals, so that there can be no doubt about its validity [1,2].
An animal organism can develop well without any assistance from the intestinal flora. While the benefits of microbes do not really exist, the harm they cause can no longer be questioned. The microbial waste product indole in small quantities, introduced over several months into the stomachs of various mammals (guinea pigs, monkeys), caused significant chronic organ damage. The brain, liver, kidneys and other organs undergo changes that should be classified as so-called sclerosis. Indole turned out to be a very dangerous poison. Phenol has a similar effect.
Alcohol and tobacco abuse, syphilis and other infectious diseases should be considered only as secondary factors of aging. People who drink a lot of alcohol and smoke a lot of tobacco often reach very old age. Other people suffer from arteriosclerosis without tobacco and alcohol.
It used to be thought that indole and phenol were produced by the body itself completely independently of the intestinal flora. This view turned out to be wrong. Not only animals that do not contain intestinal bacteria, but also those that harbor abundant amounts of them, can use protein foods without producing phenol and indole. So, infants feed on mother's milk, but these poisons are absent in their feces. Large numbers of bacteria in the gut of infants cannot cause rotting. The poisonous ability of one of the best indole generators, E. coli, is inhibited by normal bacilli of the children's intestinal canal (the so-called B. bifidus). Animals that contain very rich intestinal flora may, under certain conditions, produce neither indole nor phenol. Guinea pigs fed carrots or sugar beets do not emit these poisons. However, as soon as they are given potatoes for food, these products can be found in their secretions.
Intestinal putrefaction caused by certain bacteria chronically poisons our bodies and greatly shortens our lives. The intestines contain germs that prevent decay. A common feature in human milk, sugar beets, is a high sugar content. Milk is rich in milk sugar; sugar beet is rich in cane sugar. These types of sugar cannot themselves inhibit the decay of protein substances, but they do this through bacteria that feed on sugar and produce acids from it, namely lactic acid. Plant foods contain more sugar than animal foods. It can be assumed that this is the best remedy for delaying decay and aging changes.
Predatory animals form phenol and indole in the intestines. There are plant nutrients that lead to the production of phenol and indole. The first place is taken by potatoes, then bananas. The best in this regard are vegetables, fruits, dates. If you combine potatoes as a fairly strong poisonous agent with dates acting in the opposite direction, then the production of indole is completely suppressed. Some, despite their predominantly plant-based food, emit many aromatic poisons. There are other people who, with a rich meat diet, still produce a rather small amount of them. This depends on the nature of the intestinal flora, which varies greatly from person to person.
Rotting microbes are considered among the most dangerous. But they encounter powerful enemies - microbes that ferment sugar and produce lactic acid. These microbes must be developed in the intestines. The introduction of Bulgarian yogurt into food can reduce the harmful effects of the intestinal flora. The peoples who eat many different preparations of sour milk (leben, yogurt, kefir, etc.) are distinguished by good health and long life. These dairy products contain a lot of lactic acid bacteria that prevent rotting.
The best formers of lactic acid turned out to be microscopic sticks found in Bulgarian yogurt, and which are therefore called Bulgarian sticks. Rotting bacteria and other harmful bacteria can develop along with the Bulgarian bacillus, but their formation of poisons is inhibited. Thus, it was found that E. coli and other microorganisms from this group in the presence of lactic acid bacteria are not able to form indole and phenol.
In practice, the use of anti-proliferation bacteria has generally proven itself well. Unfortunately, only too often bad drugs are allowed into the trade, which either do not contain lactic acid bacteria at all, or contain only traces of them. Preparations sold in dry form (tablets, powders) are especially susceptible to this drawback, since all known lactic acid bacteria do not form dry-resistant forms (spores). It follows that these microorganisms must be prescribed in liquid cultures or in a wet state. Best suited for this are pure cultures stored in small tubes, which can be taken with dates for dessert.
There are other intestinal diseases that are caused by acidic fermentation (primarily butyric acid bacteria), and in which lactic acid bacteria can probably cause harm rather than benefit. Therefore, treatment with lactic acid preparations should be limited only to diseases caused by decay. When the causative agents of putrefaction have multiplied strongly, it happens that lactic acid bacteria are extremely imperfectly performing their inhibitory action. These microorganisms need for their existence in sugar-containing food, which enables them to produce sufficient amounts of acid to delay putrefaction. However, sugar is so easily absorbed that only a very small part of it reaches, or even does not even reach the lower parts of the intestinal canal. Some plant foods like beets, carrots and especially dates are the best carriers of sugar in the caecum and colon. They can therefore be of great benefit in the fight against intestinal putrefaction.
Many researchers have noted that the human small intestine, as well as a large number of animals, contains significantly fewer microbes than the large intestine. Employees of the Pasteur Institute have shown that pancreatic juice in the form in which it is excreted from the gland, either has little effect on bacteria, or does not work at all. Intestinal juice also does not produce a noticeable bactericidal effect, although it is clearly capable of agglutinating microbes. Only when both juices of the small intestine are combined, i.e., pancreatic and intestinal, can a clear bactericidal effect be obtained. Since the causative agents of putrefaction are usually anaerobes that develop on alkaline media and are incapable of growing on acidic media, it can be concluded that the introduction of acids can interfere with the processes of putrefaction in the intestine. For this reason, Gaiem uses lactic acid for bowel diseases and has very good results. Meanwhile, lactic acid is a microbial product and is produced by some intestinal bacteria like B. coli and mainly Aerogenes lactis.
Undoubtedly, microbes can penetrate the unaffected intestines. Even if microbes remain in the contents of the intestines, they can harm due to the fact that they release special substances into the bloodstream. The fact that microbial products are indeed absorbed into the blood is no longer in doubt. For a long time, a number of substances (derivatives of phenol, cresol, indole, skatole, pyrocatechol, etc.) were found in the brain of humans and animals, the microbial origin of which was suspected. Hydrogen sulfide, mercaptan`RT are also products of the activity of the large intestine.
Bouchard systematically developed the theory of autointoxication of the body, in which the food poisoning of the intestinal flora is the main one.
Absorption of digestive products begins already in the stomach and occurs mainly in the small intestine. The large intestine only finishes the work of absorption, which can occur without it. But you cannot count on extirpation and surgical removal of the colon. But London surgeon Lan sutured the lower part of the small intestine directly to the rectum. There are 120 such patients. In the vast majority of cases, the results were amazing. The sick, for whom life was one continuous torment, turned into healthy people with a ruddy complexion and good digestion. II Mechnikov's assistant sent to London confirmed the truth of these facts [1,2].
It has been established that there are three types of microbes in the human digestive tract that cause rotting. Developing in the intestines, putrefactive bacilli secrete their metabolic products. We were able to confirm that they are capable of producing poisons. By growing microbes in a sterile mi9-xture of minced meat and water, we got toxic substances that are deadly for a rabbit. They produce a toxic effect when introduced not only into the vessels, but also into the large intestine. There is no doubt about the basic fact that our digestive tract, especially the large intestine, contains harmful microbes that produce many types of poisons. Here is a description of the experience. In two balloons, small amounts of feces are inoculated. One cylinder is filled with meat in water, the other with ground vegetables and water. After two days, the liquid in the first cylinder becomes extremely toxic to rabbits, while the liquid in the second cylinder remains completely harmless. The bacterial flora in both cylinders is also sharply different.
Nutrition influences the formation of toxins by bacteria. It has long been known that rotting substances (blood, meat, feces, etc.) contain poisons, the effects of which become especially sharp when they are introduced into the blood of animals. In the contents of the small intestine, mainly digestive juices are toxic, while in the large intestine most of the poisons are of microbial origin. These different poisons behave very differently. Digestive juices are difficult to absorb by the mucous membrane, while some microbial poisons are rapidly absorbed by the walls of the large intestine. In the large intestine, microbes have at their disposal protein substances originating from food and desquamated or immigrated cells. The conditions are favorable for proteolytic action, especially since the large intestine does not contain sugars that could prevent rotting caused by microbes. It should be recognized that the bacilli that cause putrefaction and are contained in our alimentary canal are a source of autointoxication, against which the body must fight with all the means at its disposal. Indole and phenol are produced by numerous bacteria in the intestinal flora. A study of young guinea pigs reared under strictly aseptic conditions showed the complete absence of the above substances, despite the use of a significant amount of proteins such as casein by the body.
It is known that a number of microbes of the human intestinal flora form indole [1,2]. The first place among them is occupied by E. coli, this permanent inhabitant of the alimentary canal. Along with it, B. aerogenes is found, which is almost always contained in the human intestine, as well as the Welsh bacillus (B. erfringes), which is constantly found in the contents of the intestines of an adult and is extremely common in children. Pyogenic staphylococci and proteas, which are often found in the human intestinal flora, also produce this substance. Indole and phenol undergo profound changes in the body, mainly in the liver, which are ultimately excreted by the kidneys. However, only about half of these substances pass from the intestines into urine. Some of the absorbed phenols are burned in the body. According to Munch's research, a healthy person eating a regular diet excretes 17 to 51 mg of phenols in 24 hours. The amount of indican in the urine of a healthy person almost coincides with the amount of phenols, but in patients it never reaches such high figures as were obtained for the latter. The maximum amount of indican was 154 mg per liter of urine. The feces do not contain those substances that are absorbed in the large intestine. But these substances are produced in the large intestine, where it is absorbed to be excreted in the urine. Even in patients whose urine contains relatively very large amounts of phenol, the fecal masses can be completely free of it. However, phenol is the d most readily absorbed by the surface of the large intestine. Phenol, according to numerous evidences, is not produced in the small intestine. There are very few bacteria in the small intestines. There is a big difference between the poisons of the large intestine and the poisons of the small intestine. Tsibulsky and Tarkhanov (1907), having confirmed the great toxicity of the contents of the small intestine relative to the large, do not accept the provisions on the identity of the poisons of the two parts of the digestive tube. According to their experiments, severe toxicity of the contents of the small intestine is created mainly due to pancreatic juice, injection of which into the veins in sufficient quantities can lead to death within 2-3 min. Putrid pancreatic juice is even more toxic, which shows the harmful role of putrefaction. However, since pancreatic juice does not pass into the large intestine, or only a very small amount of it gets there, it is quite natural to observe a decrease in the toxicity of the contents of the colon.
Attempts to expel poorly acting microbes with laxative salts have only been temporary. Enough embryos remained in the intestines to form new cultures, as abundant as before. Food, passing through the stomach and undergoing only insufficient digestion without the disinfecting effect of hydrochloric acid, very often causes disorders that consist in the decay of protein substances. It is this type of decay that lends itself to the most favorable influence of the methodical use of Bulgarian sour milk.
The general picture of chronic poisoning with substances originating from the intestinal flora and as a result of senile degeneration is the same: the invasion of mononuclear cells and the sequential development of connective tissue. Poisons weaken the defense of organ cells and activate macrophages. An abundant number of lactic enzymes was noted in the feces of two very strong old men 94 and 97 years old. Best of all, sugars such as dates, dry grapes, carrots, beets, turnips carry sugars into the large intestine.
I.I. Grekov expressed a position that has retained its relevance: “Despite a number of works devoted to the proximal section of the large intestine, the pathology of this section is still insufficiently explained, because in these works the role of the Bauhinia flap was not taken into account at all” [3,4].
The words of Academician V.T. Ivashkin, pronounced at the All-Russian Conference of Gastroenterologists (Gelendzhik, 1996), are prophetically perceived: ≪Even the ideal implementation of all programs of cardiovascular care for the population on average can extend a person's life only up to 80 years, and full-fledged gastroenterological programs are guaranteed to increase it up to 160 years old≫ [5-7].
Nobel laureate I.I. Mechnikov: “The causes of natural death are the self-poisoning of the organism coming from the intestines. Physiological sclerosis is a consequence of prolonged poisoning with poisons arising in the colon. "
But I.I. Mechnikov did not indicate the path of development and implementation of chronic autointoxication.
In our opinion, this is the failure of the Bauhinia damper (NBZ). We present our data on chronic autointoxication in NBZ and after its surgical correction.
INTRODUCTION
The deficiency of the Bauhinium Damper (NBZ) is widespread among the population. In the study of 900 protocols of irrigoscopy, performed for various indications and not related to the diagnostic search for a Bauhinia flap insufficiency, the NBZ was detected in 64% of patients as an accompanying finding [8].
Widespread NBZ among the population of Russia due to connective tissue dysplasia (DST) and an extensive range of diseases of the colon and terminal part of the small intestine, determining, respectively, the primary and secondary NBZ [9].
Diseases of the gastrointestinal tract (GIT) occupy a prominent place in the structure of the pathology of internal organs, in Russia they are about 2500 per 100 thousand population [10]. In recent years, much attention has been paid to functional diseases of the digestive organs, which is primarily due to their high prevalence and the costs incurred by health care in connection with the examination and treatment of such patients [11]. Leading experts say that irritable bowel syndrome (IBS) affects from 10 to 20% of the adult population of developed countries, which is up to 50% of all visits to a gastroenterologist [12]. According to recent studies, the frequency of DST among adolescents reaches up to 20% (in the cohort about 3000 studied, according to the data of Professor Nechaeva G. I., and 8.5% in a sample of 400 adults [13].
According to our data [8,9], classical appendectomy, and even more so appendectomy with technical difficulties and appendectomy under conditions of a complicated course of acute appendicitis, can lead to an insolvency of the bauhinia valve. The fact of intimate anatomical and functional proximity of the valve structures of the ileocecal junction and appendix is undeniable. Appendectomy destroys these connections, and leads to the development of secondary acquired NBZ.
Many authors [14-16] admit the fact of ascending retrograde infection of the small intestinal mucosa at NBD. A pathological condition in which the titer of microorganisms in the mucous membrane of the small intestine exceeds 105 CFU / ml, or colonization of the colonic flora occurs, has been called Small Bacterial Overgrowth Syndrome (SIBO).
SIBR is a pathological condition that develops as a result of bacterial contamination of the small intestine by various microflora and is accompanied by functional disorders of the digestive conveyor [17,18].
Direct evidence of the occurrence of SIBR in case of the failure of the Bauhinia Damper (NBZ) is the experience of Larry S Miller (2012) [16]. In a clinical experiment, the author modeled the ileocecal valve insufficiency by placing a 4-lumen probe behind the lips of the bauhinia valve in the direction of the ileum of 19 healthy volunteers during a colonoscopy. 1 month after the manipulation with the help of the hydrogen breathing test, all the subjects under study revealed a syndrome of excessive bacterial growth of the small intestine. Thus, by virtually destroying the Bauhinia flap, the author achieved the emergence of SIBR from volunteers.
Currently, SIBO is recognized as a key pathogenetic mechanism in the development and persistence of many diseases of the digestive tract and associated extra-digestive conditions (bronchial asthma, dermatological atopy, diabetes, autoimmune allergic conditions, arthritis, obligate precancerous conditions, etc.).
The actual prevalence of SIBO is unknown today. Clinically, this pathological condition is poorly diagnosable due to the non-specificity of its symptoms, which are often attributed to the main disease that causes SIBO [19]. In fact, SIBO is extremely common in the presence of one or more predisposing pathological conditions. Thus, Ardatskaya MD (2011) [15] indicates that the frequency of detection of excessive bacterial growth in the small intestine in various diseases (chronic gastritis, peptic ulcer, chronic cholecystitis, pathology of the hepatobiliary system, inflammatory and other intestinal diseases (in tons. irritable bowel syndrome), scleroderma, neuropathy (as a complication of diabetes mellitus), the effects of surgery, etc.) is 40–99%. The results of the last meta-analysis [20], which included 11 studies, showed that pathological respiratory tests are much more frequently recorded in patients with IBS than in healthy individuals (OR = 4.46; 95% CI = 1.69 - 11, 80). Similar results were achieved in the second meta-analysis, published a year later, - pathological test results were significantly more frequent in patients with IBS: odds ratio (OR) 4.46, 95% confidence interval (CI) 1.69–11.80. At the same time, taking into account age and gender showed an even more significant result (OSH 9.64, 95% CI 4.26–21.82) [24].
According to the literature, the problem of SIBR is currently a purely therapeutic one. Treatment of bacterial overgrowth syndrome in the small intestine provides for the treatment of the underlying disease, replacement therapy for malabsorption syndrome and antibacterial therapy [21,17]. The main group of drugs used for SIBR is intraintestinal antibiotics [22-EHP [24]. It should be recognized that in the absence of an impact on the cause, successful pathogenetic treatment is temporary, which is confirmed by the example of rifaximin therapy. The frequency of recurrence of SIBR after effective therapy with rifaximin reached 44% after 9 months [25].
Many authors [17,26] separately stop at an obvious conclusion - the prediction of the SIBR and the risk of its recurrence after successful antibiotic therapy depends primarily on the therapeutic effect on the primary background disease that has contributed to the contamination of the small intestine. Gabrielli [25] rightly points out that the recurrence of SIBO in the event of persisting predisposing causes often leads to a chronic process and a complex, and sometimes impossible, conservative correction.
Thus, we have not encountered literary data that would describe etiotropic therapy. In our opinion, the problem of SIBO in patients with functional pathology of the gastrointestinal tract in many cases is due to damage to a specific anatomical structure, namely, the Bauhinia valve, which is a surgical problem.
We have not met domestic studies on the etiotropic effect on the syndrome of excessive bacterial growth in patients with proven deficiency of the bauhinia valve. The few foreign works [14,16] are devoted only to the statement of the fact that there is a SIBR at the NBZ.
The purpose of the study is to determine the syndrome of excessive bacterial growth of the small intestine in patients with proven insufficiency of the bauhinia valve and after its surgical correction.
MATERIALS AND METHODS
The study was conducted on the basis of the surgical department of the city hospital “Nizhny Novgorod City Clinical Hospital No. 12” in the period from September 2014 to December 2014. The main group included 20 patients (16 women, 8 men, age from 23 to 57 years) with proven by the results of irrigoscopy the insufficiency of the bauhinia valve. All patients of the main group performed Bauginoplasty according to the methods of prof. Martynova V.L. A control group of 20 patients was also formed (11 women, 9 men, age from 28 to 49 years), who underwent an irrigoscopy in order to diagnose diseases of the large intestine, according to the results of which the ileo-cecal valve turned out to be wealthy. Simultaneously, patients of the main group underwent appendectomy. The removed vermiform process was sent for histological examination. In the case of intraoperative diagnosis of mesenteric mesentery of the ileum, the altered lymph node was resected, a backseed from a section of the lymph node was performed, and his histological examination was performed.
Preparation for irrigoscopy was carried out for two days and consisted in the prohibition of food intake containing slags, in the formulation of high enemas with a total volume of 1.5 to 3 liters 3-4 times a day. It is imperative to thoroughly empty the cecum from the intestinal contents, since its presence in the form of an embossed mass may prevent the radiopaque substance from passing into the ileum with the failure of the bauhinia valve. This can lead to a false negative conclusion. The taut intestine must be filled with radiopaque substance. Repeated X-ray examination after a bowel movement is fundamentally important, since during bowel movement a maximum pressure is created in the intestine, which, if the ileocecal locking apparatus fails, will be accompanied by a pronounced reflux of the radiopaque substance into the ileum (Figure 1).

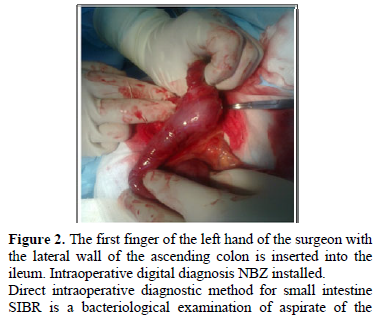
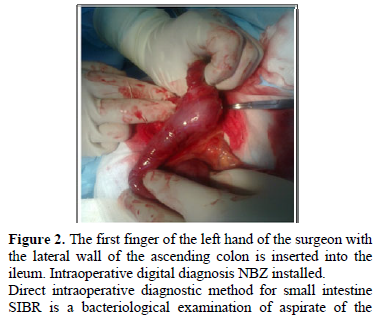
We performed intraoperative digital diagnostics of the failure of the bauhinia valve. Normally, the gap of the thin-colic transition is no more than 2 cm and does not miss the first finger of the surgeon's left hand. In the NBZ environment, on average, this transition has a diameter of 3–3.5–4 cm, which determines the almost unhindered passage of 1 finger of the left hand (so conveniently) by the surgeon into the ileum. The technique consists in the following: after extracting the ileocecal angle from the right ileal fossa, the surgeon 1 finger of the left hand brings the lateral wall of the ascending colon, opposite the ileocecal anastomosis, closer to this anastomosis and tries to insert it and the finger into the ileum. With its introduction into the ileum, in our opinion, the diagnosis of NBZ is established (Figure 2). If it is impossible to perform this manipulation, the diagnosis of the NBZ can be rejected.
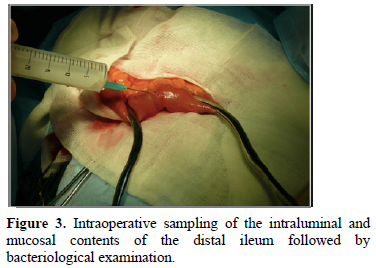
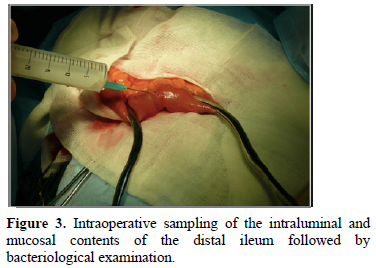
intraluminal and mucosal contents of the distal ileum (Figure 3). The technique of material sampling is as follows: 20 cm proximal to the ileocecal junction after isolation of the 10-cm long loop of the ileum with a length of 10 cm by ileum intestinal tissue, the lumen puncture is performed. The needle is held obliquely relative to the intestinal wall, 10 ml of sterile physiological NaCl solution is injected into the intestinal cavity. The exposure is maintained for 5 minutes, the contents of the isolated ileum are aspirated, until the needle passes through the mucous layer of the intestine, the needle is removed. The puncture site is peritonized. Aspirate is sent for bacteriological examination

We performed intraoperative digital diagnostics of the failure of the bauhinia valve. Normally, the gap of the thin-colic transition is no more than 2 cm and does not miss the first finger of the surgeon's left hand. In the NBZ environment, on average, this transition has a diameter of 3–3.5–4 cm, which determines the almost unhindered passage of 1 finger of the left hand (so conveniently) by the surgeon into the ileum. The technique consists in the following: after extracting the ileocecal angle from the right ileal fossa, the surgeon 1 finger of the left hand brings the lateral wall of the ascending colon, opposite the ileocecal anastomosis, closer to this anastomosis and tries to insert it and the finger into the ileum. With its introduction into the ileum, in our opinion, the diagnosis of NBZ is established (Figure 2). If it is impossible to perform this manipulation, the diagnosis of the NBZ can be rejected.
intraluminal and mucosal contents of the distal ileum (Figure 3). The technique of material sampling is as follows: 20 cm proximal to the ileocecal junction after isolation of the 10-cm long loop of the ileum with a length of 10 cm by ileum intestinal tissue, the lumen puncture is performed. The needle is held obliquely relative to the intestinal wall, 10 ml of sterile physiological NaCl solution is injected into the intestinal cavity. The exposure is maintained for 5 minutes, the contents of the isolated ileum are aspirated, until the needle passes through the mucous layer of the intestine, the needle is removed. The puncture site is peritonized. Aspirate is sent for bacteriological examination
Indirect techniques included the determination of urinary indican (by the method of Obermeyer) before the operation and on the 7th and 45th day after bauginoplasty; hydrogen respiratory test (VDT) with a lactulose load, which was carried out using a Gastrolyser apparatus before the operation and on the 7th and 45th day after the operation. A preoperative study of patients with NBZ using these techniques was performed prior to the radiopaque examination of the intestine, or 4 weeks after irrigoscopy. Patients of the main group did not receive antibiotic therapy in the postoperative period. Preoperative preparation consisted of 3-fold cleansing enemas, which could not affect the biocenosis of the small intestine.
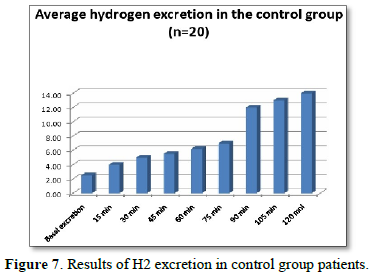
In order to determine the syndrome of excessive bacterial growth in the patients of the control group, indirect diagnostic methods were carried out, which included the determination of urine indican (by the method of Obermeier) and VDT with a load of lactulose, performed using a Gastrolyser apparatus. The study preceded the irrigoscopy.
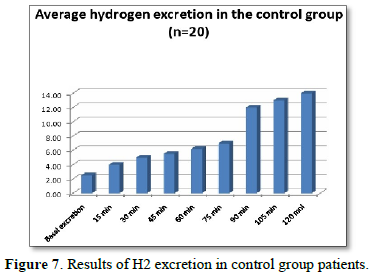
Preparation of patients for VDT with lactulose was carried out according to the method proposed by [34]. The diagnostic criterion for the presence of SIBS in patients was an increase in H2 excretion after exercise in the period from 0 to 60 min by 10 ppm (in the absence of abdominal symptoms after lactulose, such as abdominal pain, rumbling, flatulence, diarrhea) and 5 ppm (in the presence of abdominal symptoms). The group included patients with basal secretion of hydrogen up to 5 ppm.
It was carried out using statistics.
RESULTS AND DISCUSSION
Postoperative complications in the patients of the main group were not observed. The proposed preoperative irrigoscopy. It was confirmed that a chronic inflammatory catarrhal was observed in all 20 cases.
Intraoperative mesadenitis was detected in 16 patients of the main group. It has been shown that there has been no clear link between the cortical and cerebral layers. The following is the result: E. coli hemolytic was determined in 9 cases (104 CFU / ml), St. aureus - in 7 cases (103-4 CFU / ml).
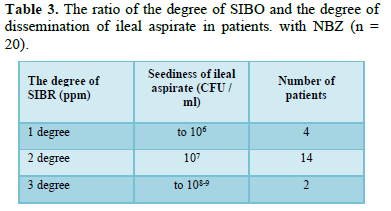
It has been taken for 20 patients who have been diagnosed in the biocenosis. The spectrum of microorganisms is determined by the following microorganisms: E. coli hemolytic was determined in 10 patients (105-107 CFU / ml), St. aureus-in 6 patients (106-108 CFU / ml), C. albicans-in 4 patients (105-109 CFU / ml). The sown flora is identical.
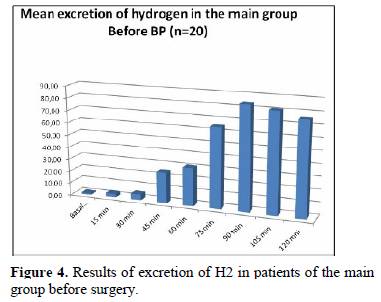
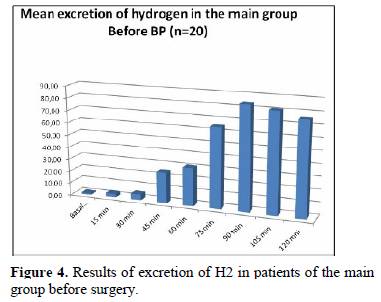
Bauginoplasty (BP) according to the results of the patient’s life cycle (Figure 4), the colony peak at 90th minute). The patients of the main group were distributed as follows (Table 1).
The determination of urinary indican in patients of the main group before surgical correction gave positive results in 16 cases (Table 2). The presence of an insignificant (1 degree - increase up to 50 ppm) distal syndrome of excessive bacterial growth in 4 patients in whom urine indican was negative may indicate a lack of sensitivity of this screening test compared to VDT.
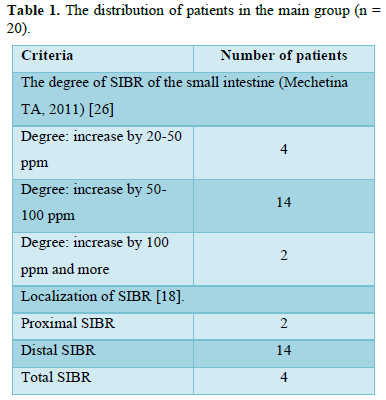
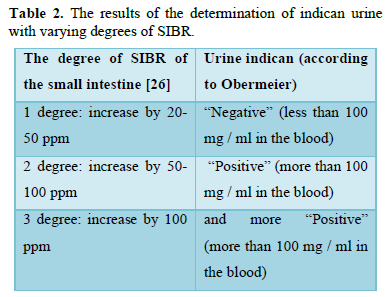
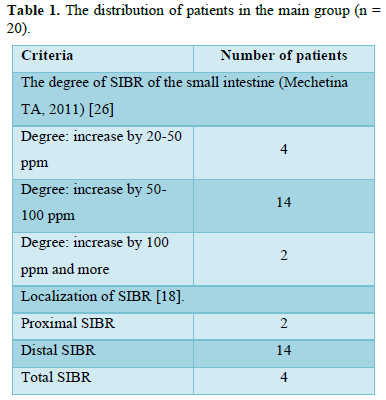
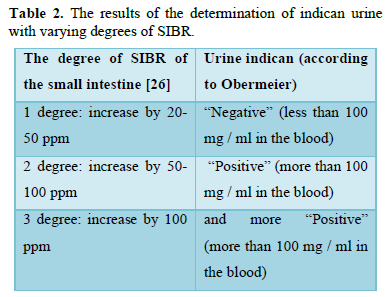
On the 7th and 45th days of the postoperative period, in the absence of antibiotic therapy, indican urine in all operated patients (n = 20) was negative.
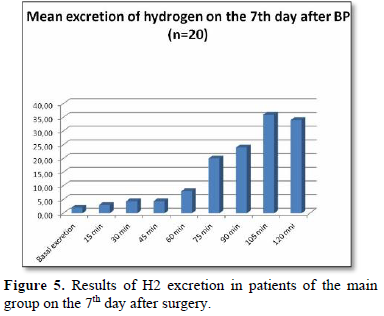
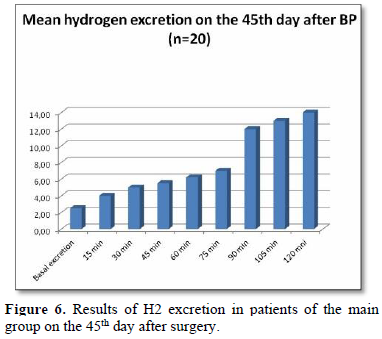
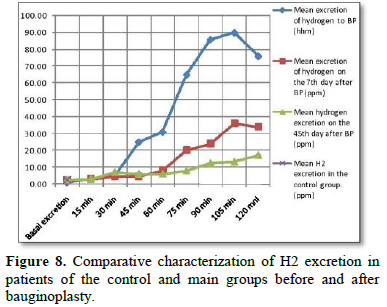
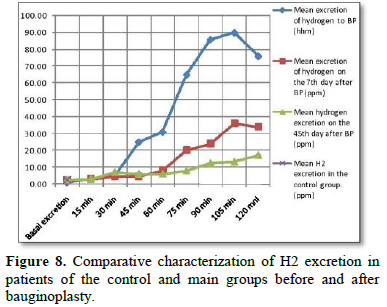
According to the results of VDT with lactulose load in patients of the main group on the 7th day after the Bauginoplasty (BP) (Figure 5), all of the patients underwent a significant reduction in the amount of hydrogen released, while the lactulose passage through the intestines normalized (the large intestinal peak is determined at 75 minute). On the 45th day after Bauginoplasty, VDT corresponded to the norm in all patients (Figure 6).
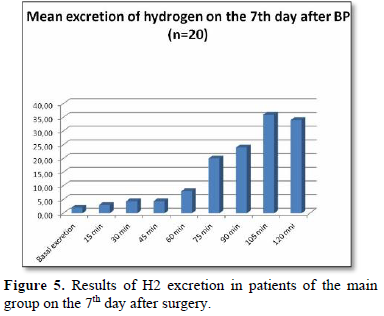
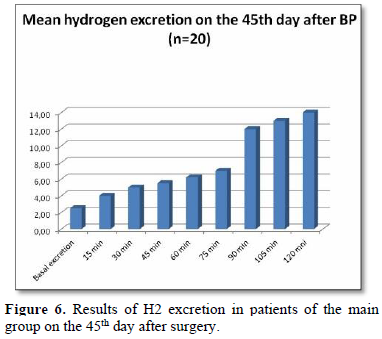
Our studies confirm the presence of small intestine SIBR in patients with NBZ, which is consistent with the data of foreign authors [14, 16] and fits into the logic of colonic reflux pathogenesis in the small intestine. On the reliability of the data in this study cannot speak. However, an obvious difference is found in the results of VDT in patients of the compared groups: a significant decrease in the concentration of hydrogen released after the operational benefit (Figure 8). The first facts obtained objectively indicate the effectiveness of Bauginoplasty, the positive clinical results of which we observed in 500 operated patients with NBZ [9].
The results of the bacteriological examination of the ileum aspirate of patients with NBZ confirm the presence of SIBR detected by HTD with a load of lactulose. At the same time, a correspondence was established between the degree of SIBR (according to the results of VDT) and the degree of contamination of ileal aspirate (Table 3). This is consistent with the data of Mendoza [28], which established the sensitivity (85.7%) and specificity (90.9%) of the hydrogen breath test with lactulose compared with the “gold standard”.
The determination of indican urine makes it possible to suspect SIBS in patients with a pronounced degree of dissemination of the small intestine (increased H2 excretion above 50 ppm), but not informatively in patients with SIBS grade 1 (elevation of H2 to 50 ppm) compared to VDT. The revealed diagnostic value of this method retains its value as a screening test for small intestine SIBR of 2 and 3 degrees.
The phenomena of mesadenitis and the presence of microorganisms in the lymph nodes confirm the translocation of microorganisms through the intestinal wall. The fact of bacterial translocation diagnosed in patients with SIBO of the small intestine under NBZ conditions is consistent with the literature data [29-33].
FINDINGS
-
Patients with a normally functioning ileocecal valve are not predisposed to the formation of a distal SIBO.
-
SIBR is obligately associated with the NBZ and determines the process of bacterial translocation.
-
A positive qualitative reaction of urine to indican indicates that the patient has a SIBO of the 2nd degree and higher.
-
SIBO was determined in 20 (100%) patients with NBZ: 1 degree - in 4 (20%) patients; Grade 2 in 14 (70%) patients; Grade 3 in 2 (10%) patients;
-
On the 7th day after Bauginoplasty, SIBR Grade 1 was determined in 8 (40%) patients, and in 12 (60%) operated patients, data for SIBO were not revealed according to the results of VDT;
-
On the 45th day after Bauginoplasty, the concentration of hydrogen released corresponded to the norm;
-
Bauginoplasty - a method of etiopathogenetic impact on the syndrome of excessive bacterial growth in the small intestine in patients with NBZ.
- Mechnikov II (1908) Etudes about human nature. M: Hauka, pp: 245.
- Mechnikov II (1913) Etudes of optimism. Moscow: Nauka, pp: 213.
- Grekov II (1952) Selected works / I.I. Grekov. M: Medicine, pp: 28-51.
- Grekov II (1972) Bauginiospasm and bauginoplasty (to the question of the so-called chronic appendicitis, relapses of pain after appendectomy and their treatment). Bull Surg 9: 122-151.
- Ivashkin VT, Trukhmanov AS (2000) Diseases of the esophagus: Pathological physiology, clinical picture, diagnosis, treatment. M: Triada-X. pp: 179.
- Ivashkin VT (1993) Syndrome // Ros. zhurn. Gastroenterol Hepatol Coloproctol 2(3): 27-34.
- Ivashkin VT, Trukhmano AS (2003) Modern approach to the treatment of gastroduodenal reflux disease. Mil Med J 10: 26-34.
- Martynov VL (2013) Surgical treatment of reflux disease: Monograph / V.L. Martynov. - Nizhny Novgorod, Publishing house LLC. Center for operational printing. pp: 535.
- Martynov VL (2006) Refluxes of the digestive tract and their surgical correction: dis. Dr. honey. Sciences: 14.00.27 / Martinov Vladimir Leonidovich. Saransk. pp: 261.
- Filippova TV (2014) The value of medical genetic counseling for diseases of the digestive system. RZhGK 1: 56-61.
- Sheptulin AA (2010) Gastroesophageal reflux disease and functional diseases of the gastrointestinal tract: Is there any connection? / A. A. Sheptulin, M. A. Wiese-Hripunova. RZhGGK. 4: 44-48.
- Sperber AD, Drossman DA, Quigley EM (2012) The Global Foundation for World Gastroenterology Organization symposium. Am J Gastroenterol 107(11): 1602-1609.
- Nechaeva GI, Yakovlev VM, Gromova OA, Torshin IYU (2009) Connective tissue dysplasia in children and adolescents. Innovative hospital-saving technologies for diagnosis and treatment in pediatrics. M.: Union of Pediatricians of Russia. pp: 96.
- Zaidel O (2003) Uninvited Guests: The Henry C. Lin. Practical Gastroenterology XXVII (7): 24-37.
- Ardatskaya MD (2011) Syndrome of excess bacterial growth: A tutorial / M. D. Ardatskaya. - Moscow: Forte print. pp: 56.
- Miller LS, Vegesna AK, Sampath AM, Prabhu S, Sesha Kotapati K, et al. (2012) Ileocecal valve dysfunction in small intestinal bacterial overgrowth: A pilot study. World J Gastroenterol 18: 6801-6808.
- Kucheryavy YA, Cheryomushkin SV, Mayevskaya EA, Sutugina EA (2014) Interrelation of irritable bowel syndromes and excessive bacterial growth: Is it there? RZGGK 2: 5-14.
- Maev IV, Ivashkina NY, Kucheryavy YA, Oganesyan TS (2011) Diagnosis and treatment of the syndrome of excessive bacterial growth in the small intestine. Eksper Wedge Gastroenterol 3: 125-129.
- Bures J, Cyrany J, Kohoutova D, Forst LM, Rejchr TS, et al. (2010) Small intestinal bacterial overgrowth syndrome. World J Gastroenterol 28: 2978-2990.
- Ford AC, Spiegel BM, Talley NJ, Moayyedi P (2009) Small intestinal bacterial overgrowth in irritable bowel syndrome: Review and meta-analysis. Clin Gastroenterol Hepatol 7: 1279-1286.
- Avdeev V (2010) Diagnosis and treatment of bacterial overgrowth syndrome in the small intestine. Doctor 12: 1-3.
- Plotnikova EY, Borsch MV, Krasnova MV, Baranova EN (2013) Some aspects of diagnosis and treatment of excessive bacterial contamination of the small intestine in clinical practice [electronic resource]. Attending doctor 4.
- Poluektova EA, Kuchumova SY, Sheptulin AA, Ivashkin VT (2013) Treatment of irritable bowel syndrome from the standpoint of modern ideas about the pathogenesis of the disease. RZGGK 1: 57-65.
- Kucheryavyi YA, Oganesyan TS (2010) Syndrome of excess bacterial growth. RGGGK 5: 63-68.
- Gabriell M, Bonazzi P, Scarpellini E, Bendi AE, Lauritano EC, et al. (2011) Prevalence of small intestinal bacterial overgrowth in Parkinson's disease. Mov Disord 26: 889-892.
- Lauritano E, Gabrielli M, Scarpellini E, Lupascu A, Novi M, et al. (2008) Small intestinal bacterial over growth recurrence after antibiotic therapy. Am J Gastroenterol 103: 2031-2035.
- Gabrielli M, Angelo GD, Rienzo TDI, Scarpellini E, Ojetti V (2013) Diagnosis of small intestinal bacterial overgrowth in the clinical practice. Euro Rev Med Pharmacol Sci 17: 30-35.
- Mendoza E (2007) Diagnosis of small intestinal bacterial overgrowth in children: C., Crismatt C., Matos R. Biomedica 27(3): 325-332.
- Wiest R, Garcia-Tsao G (2005) Bacterial translocation in cirrhosis. Hepatology 41: 422-433.
- Hashimoto N, Ohyanagi H (2002) Effect of portal portal hypertension on gut mucosa. Hepatogastroenterol 49: 1567-1570.
- Heuman DM (2004) Persistent ascites and low sodium, identify patients with MELD scores and D. Abu-assi, S. G., Habib A. Hepatology 40: 802-810.
- Zharkova MS, Mayevskaya MV, Ivashkin VT (2012) Influence of excess bacterial growth syndrome and bacterial translocation on the course of the disease in patients with cirrhosis of the liver. RGGG 5: 56-63.
- Mechetina TA (2011) Syndrome of excessive bacterial growth in the small intestine after cholecystectomy. Dis Cand Honey Sci. Moscow pp: 134.
- Ledochowski M (2008) Hydrogen Breath tests. 1st Innsbruck: «Akademie» 59.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Diabetes (ISSN: 2644-3031)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)









