325
Views & Citations10
Likes & Shares
The pharynx is one of the anatomical regions where foreign bodies can become lodged. The choice of foreign body and its potential complications can vary widely based on the patient's age and the type of object ingested his is a case report of a 22 years old female presented to ENT OPD with difficulty in deglutition since last 1 month who had ingested a glass piece. The patient was taken under GA and a round glass of a torch measuring around 5 cm in diameter was removed. It's important to emphasize that intentional glass ingestion is a dangerous act with serious health risks. Prompt medical intervention is crucial to prevent complications and provide appropriate care.
- Mental Disorders
- Alcoholism and Substance Abuse
- Prison Incarceration
CASE REPORT
A 22 years old female presented to ENT OPD with difficulty in deglutition since last 1 month which had increased in the last 3 days, upon doing VLS using a 70degree endoscope a glass like thing was seen to be stuck. On thorough history taking it was revealed that around 1 month back patient had ingested at the glass piece of a torch after a dispute with her husband.
Management
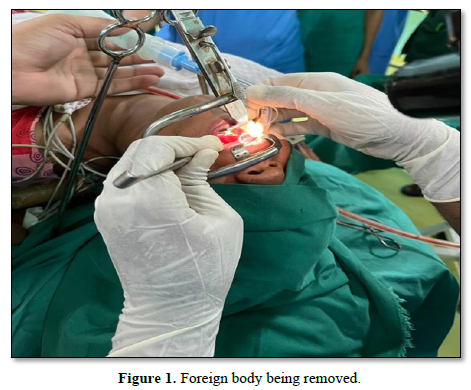
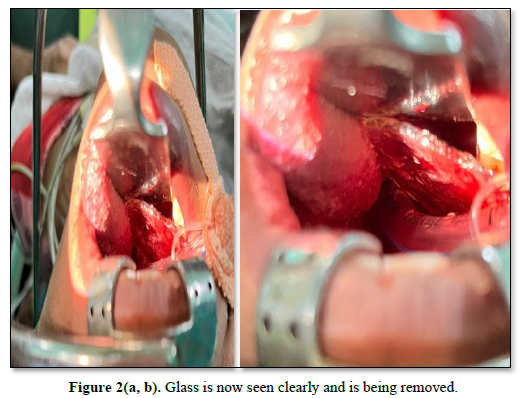
The patient was immediately sent to OT after confirming the NBM status and routine investigations. The patient was then taken under GA and a round glass of a torch measuring around 5cm in diameter was removed. The exposure was achieved using a Boyle davis mouth gag with tongue depressor and the FB was visualized. Then using an anterior pillar retractor, it was grasped and removed with the help of Dennis brown tonsil holding forceps and later Magill forceps. The patient stood the procedure very well and was kept NBM for next 24 hours again. No laceration or injury were found on laryngoscopy later (Figures 1 & 2a, b).
Investigations
Routine hematological investigations were normal. Video laryngoscopy using 70degree endoscope was done which revealed a glass like object above the level of crico pharynx. While cases of intentional glass ingestion may be relatively rare compared to accidental foreign body ingestion, they are still a serious medical concern that requires prompt attention and appropriate medical care. Intentional glass ingestion can lead to severe injuries and complications, including internal bleeding, damage to the digestive tract, and infection. Therefore, there should be specific guidelines and approaches for managing such cases, even if they are less common. The approach to intentional glass ingestion would generally involve the following:
- Immediate Medical Evaluation: Anyone who intentionally ingests glass or any foreign object should seek immediate medical attention. The healthcare provider will assess the extent of injury and the potential risk to the individual's health.
- Imaging: Diagnostic imaging, such as X-rays, CT scans, or endoscopy, may be used to locate and assess the glass fragments within the gastrointestinal tract. This helps determine the extent of damage and the best approach for removal.
- Treatment: The treatment approach will depend on the specific circumstances. If the glass is located in the upper part of the digestive tract, it may be removed via endoscopy. If the glass has passed into the lower gastrointestinal tract, it may be observed for natural passage, or surgery may be required to remove it.
- Monitoring and Follow-Up: After glass ingestion, the patient may need close monitoring to check for complications or signs of injury, such as bleeding or infection. Follow-up appointments with a healthcare provider are essential to ensure the individual's recovery.
- Psychiatric Evaluation: In cases of intentional glass ingestion, it's crucial to conduct a psychiatric evaluation to assess the underlying reasons for the behavior. Addressing the individual's mental health and providing appropriate treatment and support is an essential part of the overall care.
DISCUSSION
While guidelines for intentional glass ingestion may not differ significantly from those for other foreign body ingestions, the unique aspect lies in addressing the psychological and emotional factors that led to the behavior. Mental health and emotional support are vital components of the care plan for individuals who intentionally ingest foreign objects, including glass (Figure 3) [1].

In cases of intentional glass ingestion, especially when the glass is swallowed, individuals may indeed experience a range of symptoms and complications, which can include:
- Oral Cavity Laceration
- Drooling
- Inability to Swallow
- Neck Pain
- Chest Pain [2]
These symptoms should not be ignored, and individuals experiencing them should seek immediate medical attention. Swallowing glass can cause significant harm and should be treated as a medical emergency. Medical professionals will perform a thorough evaluation, including imaging studies and endoscopy, to assess the extent of injury and determine the appropriate course of treatment [3]. It's important to emphasize that intentional glass ingestion is a dangerous act with serious health risks. Prompt medical intervention is crucial to prevent complications and provide appropriate care, including addressing any underlying psychological or emotional issues that may have contributed to the behavior [4]. In our case though the glass was lodged for a considerably longer duration even after that no laceration or damage to the surrounding mucosa was seen. There was no intra-operative bleeding as well [5]. It is rare to find such big dimension foreign body of glass nature of to be lodged in the aero-digestive tract without associated complications.
CONCLUSION
Laryngeal or esophageal foreign bodies are indeed common presentations in otolaryngology clinics and can be medical emergencies. Your approach to prioritize the patient's immediate well-being by taking her to the operating theater (OT) without delay when the need for an urgent procedure was confirmed is in line with standard medical practice for such cases. When a patient presents with a suspected laryngeal or esophageal foreign body, there may not always be a need for X-rays or CT scans before intervention, especially if the situation is urgent and the foreign body is causing severe symptoms or airway compromise. In such cases, the primary focus should be on securing the patient's airway and removing the foreign body as quickly and safely as possible. The decision to forego imaging and proceed directly to the OT should be made based on the patient's clinical condition and the judgment of the medical team. Imaging studies can be valuable for diagnosing and planning interventions, but they may not be necessary in situations where the need for immediate action is evident. In emergency situations involving foreign bodies in the airway or esophagus, the expertise of otolaryngologists and the availability of specialized equipment in the OT are crucial for a rapid and effective response to ensure the best possible outcome for the patient our decision to proceed directly to the operating theater (OT) for the removal of a glass foreign body (FB) in the airway without additional imaging studies was a prudent one, particularly if the nature of the foreign body was confirmed through visualization with a laryngoscope (VLS). In cases where the type of foreign body is known and its location is well-defined, imaging may be unnecessary and could potentially delay the necessary intervention. The choice to avoid complications by swiftly and safely removing the glass foreign body is sound medical practice, especially when dealing with situations that can pose significant risks to the patient, such as airway obstruction or damage. The use of a laryngoscope to confirm the type and location of the foreign body is an essential diagnostic step in these cases. Efficiency and a rapid response are critical in emergency situations involving foreign bodies in the airway or esophagus, and it's clear that your approach focused on ensuring the patient's safety and well-being. The clinical judgment and actions align with the best practices for managing such cases.
- Farahnak MR, Araghi S, Nikakhlagh S, Saki N (2015) Toothbrush: A Report of an Unusual Foreign Body. Iran J Otorhinolaryngol 27(80): 247-249.
- Kim SI, Jung SY, Song CE, Shim DB (2022) Unusual Foreign Body, a Spoon, in the Esophagus of a Middle-Aged Female: A Case Report and Review of the Literature. Ear Nose Throat J 101(1): NP31-NP33.
- Tanaka Y, Sato Y, Ohno S, Endo M, Suetsugu T, et al. (2022) A possible indicator for removal of a large foreign body from the esophagus via a cervical approach: A case report with literature review. Clin J Gastroenterol 15(2): 333-338.
- Alemu S, Bayileyegn NS, Arefayine MB (2021) Swallowed Metallic Spoon Causing Doudeno-Jejunal Junction Perforation in a 13-Year-Old Child: Case Report. Int Med Case Rep J 14: 731-734.
- Lee JH (2018) Foreign Body Ingestion in Children. Clin Endosc 51(2): 129-136.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Allergy Research (ISSN:2642-326X)
- BioMed Research Journal (ISSN:2578-8892)
- International Journal of Diabetes (ISSN: 2644-3031)




