689
Views & Citations10
Likes & Shares
Introduction: Diffuse large B-cell lymphoma (DLBCL) is the most common lymphoid malignancy in adults. This subtype of lymphoma is poorly investigated among black Africans. The purpose of our work was to evaluate the survival of adult DLBCL patients followed at the Douala General Hospital (DGH), Cameroon in order to provide knowledge and better plan for care.
Patients and methods: In a retrospective descriptive and analytical study, we studied the medical records of 49 patients with diffuse large B-cell lymphoma between 2007 and 2016 in the Department of internal medicine of the DGH (hematology unit). We studied treatment response, overall survival, event-free survival, and event-related survival (relapse). Data was analyzed using univariate and multivariate analyses.
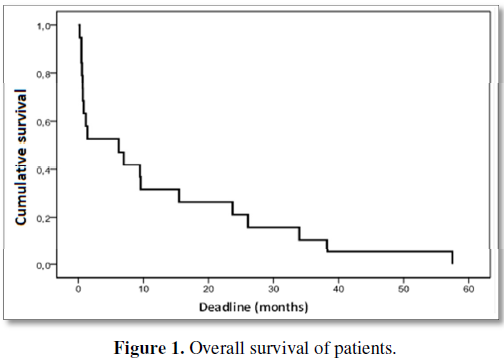
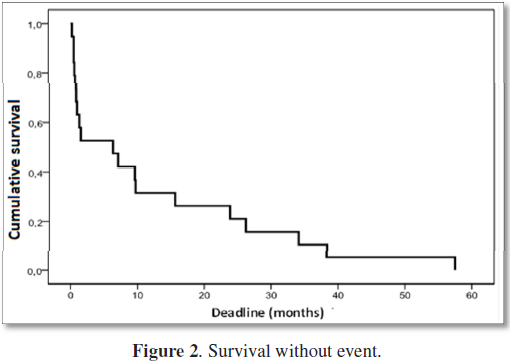
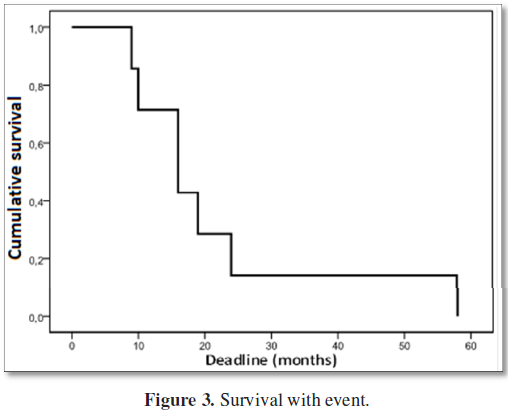
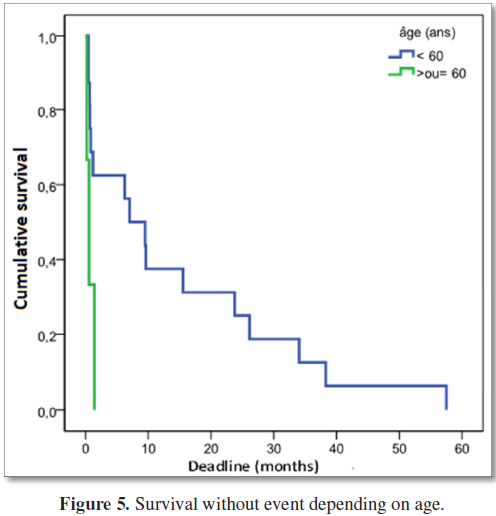
Results: The median age of patients was 47 years old. The most represented age group was 50 to 59 years old. We noted a male predominance with a male/female sex ratio of 2.5. The extra-ganglionic location was predominant at 42.9%; lactate dehydrogenase (LDH) was high in 61.2% of patients. The CHOP (cyclophosphamide, oncovin, doxorubicin, and prednisolone) protocol was the most used (71.4%), making it possible to obtain a complete remission rate in 65.3% of cases. However, for patients who received rituximab in combination with CHOP, the complete response rate was 72.7% (8 out of 11 patients). The median Overall Survival (OS) was 10.5 months. The median survival for the CHOP protocol was 9.6 months whereas for the R-CHOP protocol it was 15.7 months. The median of event-free survival was 6.2 months, better for the under 60 age group, and the median for event-specific survival was 16.0 months.
Conclusion: The survival of patients with large B-cell lymphoma remains low in our limited-income trial. Access to immunotherapy for a large number of patients could improve this survival.
Keywords: Diffuse large B-cell lymphoma, Survival, Douala
INTRODUCTION
PATIENTS AND METHODS
Our study was carried out in the Hematology unit of the General Hospital of Douala-Cameroon from January 2007 to December 2016. We included all patients with diffuse large B cell lymphoma who’s histological and immunohistochemical diagnoses were performed after a biopsy of the lymph nodes or organs, with a complete medical file and who had received a chemotherapy protocol.
The study was retrospective, descriptive and analytical. Each medical record was exploited using a survey form. The following items were searched:
· Demographics: age, sex
· Exposure to pesticides
· The presence of certain comorbidities: HIV, viral hepatitis B and/or C, HTN
· Clinical data: general condition (weight loss, night sweats, fever and activity index according to WHO standard) as well as localization of lymphoma (lymph node or extra nodal)
· Biological examinations: blood count, blood LDH activity, beta-2 micro globulin, transaminase, urea, creatinemia, blood electrolytes
· Histological examinations: anatomopathological and immunohistochemical
· X-ray examinations: standard radiography, CT scan, abdominal ultrasound
· Immunohistochemistry was performed at Centre Pasteur in Cameroon. The biological assessment and the radiological explorations were made at the DGH.
· The protocol used: CHOP, R-CHOP (rituximab, cyclophosphamide, oncovin, doxorubicine, prednisolone), COP (cyclophosphamide, oncovin, prednisolone)
· The response to treatment: complete remission or partial remission
· Global survival, with and without event (relapse...)
Prognostic factors were identified by a univaried and multivariate analysis. Complete remission was characterized by the disappearance of all clinical, biological and radiological signs of the disease. Partial remission was a partial regression of the tumor.
Therapeutic compliance was assessed based on the regularity of the administration of chemotherapy. Patients who received treatment every 21 days had good compliance, whereas those who had treatments with intervals greater than 21 days had poor compliance.
Overall survival (OS) was defined as the time elapsed since the beginning of first-line chemotherapy to the date of death regardless of the cause or until the date of the last follow-up. Event-free survival (EFS) was defined as the time elapsed between the onset of first-line chemotherapy and the onset of any symptom of treatment failure, including progression of the disease or discontinuation of treatment for any reason (toxicity, patient preference, documented progression or death). Survival with event was defined by the time elapsing between the start of chemotherapy and the various relapses until the date of the latest news or death of the patient. Our study was approved by an ethics committee of the University of Douala and we obtained the authorization of research of the General Hospital of Douala. The anonymity of the patients was respected during the exploitation of the data.
The collected data were analyzed with the Epi-Info 7.0 and Excel 2007 software. The statistical analysis used the calculation of the averages and the Chi2 test. The level of significance was set at 5% for the value of p. The calculation of survival was done according to the Kaplan-Meir method thanks to the existence in the record of an inclusion date (date of admission) and a date of assessment (date of death or latest news) mentioned by day, month and year.
RESULTS
The general characteristics (demographic and clinical) of the study participants are presented in Table 1 and the para-clinical assessment of patients in Table 2.
The consultation period was less than or equal to 3 months in 28.6%, 3 to 6 months in 20.4% and more than 6 months in 51%.
Regarding HIV infection, 7 patients (14.3%) were positive and 4 patients (8.2%) were exposed to pesticides.
With respect to treatment (Table 3) the complete remission rate was 65.3%, and the partial remission rate was 26.5%. The failure rate was 32.7%.
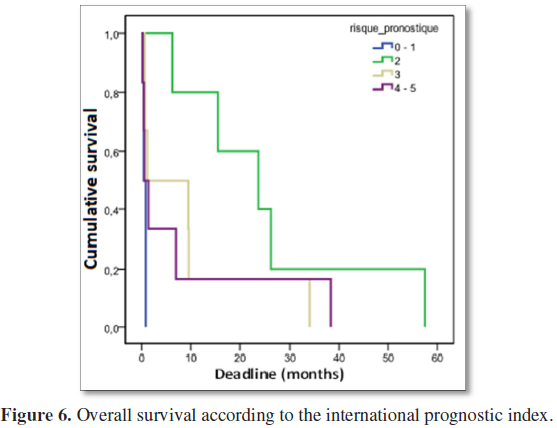
In our study, there was no statistically significant difference between overall survival and international IPI prognosis index (P=0.1). For an IPI between 0-1 the median survival was 0.5 months, for an IPI at 2, the median survival was 23.8 months; for an IPI at 3, the median survival was 1.2 months and for an IPI between 4-5, the median survival was 0.6 months (Figure 6). Death was observed in 12 cases, 24.5%. It was renal disease in 1 case (8.3%), anemia in 3 cases (25%), infections in 2 cases (16.6%) and 6 cases (50%) for which cause of death was indeterminate.
The relationship between the therapeutic response and the general characteristics of the patients are given in Table 4, with a unified analysis.
The median age of our study population was 47 years old. Diffuse large B-cell lymphoma can occur at any age, but most patients were under 60 years of age; the most affected age group was between 50 and 59 years of age. The young age of our patients could be a particular epidemiological element justifying the propagation of diffuse large B cell lymphoma in Cameroon and even African black people. But also, because life expectancy is lower in sub-Saharan Africa. It is on average 60.2 years for men and 63.1 years for women [6]. The sex ratio was 2.5 in favor of males. This male predominance is confirmed by several authors in West Africa as in North Africa [7,8].
The consultation period found here was between 4-6 months for 20.4% of patients and more than 6 months for 51% of patients. The long delay before the first consultation would be partly due to ignorance of the severity of the disease among affected people. Patients often present late in the hematology consultation after several transfusions or after treatment with products from the African pharmacopoeia [9]. But, this can also be explained by financial difficulties preventing early diagnosis and treatment [10-12].
The majority of the patients (95.9%) were at stages III and IV of Ann Arbor scale. This could be explained by the delay in diagnosis related to ignorance and limited financial resources.
In our study, we found an extra ganglionic localization in 42.9% of cases, similar to that of Abdelhamid et al. [7] in Egypt. Tolo et al. [8] reported lymph node involvement in 59% of cases. According to Mounier et al. [13], the presence of more than one extra-ganglionic localization represents a factor of poor prognosis.
Immunohistochemistry was performed in 19 patients out of 49. The CD 20 receptor was found in 84.2% of cases. Ngouadjeu et al. [14] in 2016, in a series of 44 patients with extra nodal lymphoma counted 6 patients who achieved immunohistochemistry. All patients (63) in the Ivorian study in 2012 had performed immunohistochemistry [8]. The lack of financial means and the lack of adequate technical platform could explain the low frequency of realization of this examination in our context. HIV serology was positive in 7/49 patients or 14.3%. Some authors have noted that HIV infection and immunosuppression increases the risk of developing cancer in general and lymphoma in particular [8].
Pesticide exposure was noted in 4 patients, i.e., 8.2%. Preliminary studies carried out by Alavanja in the United States in 2006, noted that in a population of 37,343 farmers exposed to the use of agricultural pesticides, there were 4000 new cases of cancer, 10% of which were hematological malignancies [15].
At least one clinical B signs were present in 73.5% of patients. This value is close to that found by Tolo et al. [8] in Ivory Coast which was 75%. The presence of clinical B signs is due to the disseminated nature of the disease but also to the delay of the consultation.
Four protocols were used namely R-CHOP, CHOP, COP and ACVBP. Among these protocols, CHOP, which for a long time was the standard treatment for diffuse large B-cell lymphoma, was the most used with 71.4% of cases, followed by 22.5% R-CHOP. We observed a better response to treatment with the R-CHOP protocol. Indeed, of the 11 patients who received the R-CHOP protocol, 8 were on CR. We can say that the addition of rituximab to chemotherapy regimens significantly improved the outcome of treatment of diffuse large B-cell lymphoma [16]. We obtained 32 (65.3%) cases of complete remission; this rate of complete remission is similar to that observed by Tolo et al. [8] (68%). This proportion of complete remission observed in our series could be explained by the fact that these patients were being followed up in a referral hospital usually attended by people with middle-income level.
It was also noticed that 30 patients received 4-7 courses of chemotherapy while 18 received at least 8 courses of chemotherapy. The unfinished treatment could be explained by the feeling of being cured when the general condition improves and/or the mass disappears. We recommend that routine use of rituximab immunotherapy be combined to CHOP (R-CHOP) as an appropriate alternative. However, the price of the anti-CD 20 monoclonal antibody (CFAF 836,000 per 500 mg bottle) remains high for Cameroonians who do not have health insurance. We agree with some authors that it is necessary to develop a Europe - Africa or America-Africa partnership to better specify the diagnosis of lymphoma and to propose an adapted treatment, this in view of the insufficiencies in human resources, infrastructures and financial [17].
The duration of follow-up was 12 months whereas the median of overall survival was 10.5 months. Overall survival was 50%, 41.7% and 8.3% respectively at 1 year, 3 years and 5 years. The Median survival without event was 6.2 months. The survival without event was better for the age group <60 years (7.0 months) compared to the age group ≥ 60 years (0.6 months). The median survival with event was 16 months. In South Korea, Jang et al. [4] in 2011, in a series of 177 patients had a median follow-up duration of 52 months, a mean survival without event and overall survival at 3 years of 62 and 74%, respectively. The difference between the 2 series would be related to the fact that all patients in the Korean series had more lymph nodes involvement in most cases, a WHO score between 0 and 1 and that the R-CHOP protocol was the mostly used. In France, the 5 year survival for the entire cohort was 59% [18]. In Tunisia, overall survival at four years was 56%. Event-free survival was 49% [7]. Tolo et al. [8] observed event-free survival at 3 years was 32% and overall survival at 3 years was 50% [8]. The 3-year survival in the Ivorian series was superior to ours (41.7%); our poor survival rate is explained by the advanced stage of the pathology during the first contact with the specialist, the underutilization of the immunotherapy and the lack of recourse to therapeutic intensification.
The median survival for the CHOP protocol is 9.6 months whereas for the R-CHOP protocol it is 15.7 months. Li et al. [19] in China in 2012 showed a median survival for the CHOP protocol of 70.2% and 84.1% for the R-CHOP protocol. The Chinese study found that R-CHOP provided a greater benefit of survival in the initial treatment of DLBCL [19]. This result comforts us that the addition of rituximab to chemotherapy would significantly improve the clinical outcome of patients with DLBCL [5].
Treatment regularity was associated with complete remission (P=0.002). Tolo et al. [8] found factors associated with complete remission to be associated to the Ann Arbor stage, to the biological symptoms, to international prognostic index, and the socio-economic level. Treatment-compliant patients had a high complete remission rate (75.6%), which could be explained by the fact that CHOP was also effective, but the long delay between chemotherapy treatments may be conducive to re-evolution of the disease.
There is a statistically significant difference (P=0.018) between survival without event and age; the response in patients younger than 60 was better. The median for the age group <60 years is 7.0 months while for the age group ≥ 60 years it was 0.6 months. However, the Chinese study found that elderly patients (>60 years) have a higher overall survival than younger patients (≤ 60 years) [19]. Patients over 60 years of age less supported the disease and treatment probably due to comorbidities and advanced stage of the disease.
CONCLUSION
The majority of patients had the clinical and biological features of advanced disease. The cyclophosphamide doxorubicin, vincristine and prednisone (CHOP) protocol was still the most used. The combination of Rituximab with CHOP (R-CHOP) chemotherapy provided a better rate of complete remission. Compliant patients also had a better response. The median of global longevity was 10.5 months. The median of event-free survival was 6.2 months and the median of event-specific survival was 16.0 months. Rapid diagnosis and meaningful use of immunotherapy would improve patient survival and allow studies to be conducted on a prospective basis.
CONFLICTS OF INTEREST
The authors do not declare any conflict of interest.
AUTHOR’S CONTRIBUTION
Ngouadjeu, Souga, Tomowiak have designed and redacted the article.
Banos, Chetcha, Mouelle have contributed to the writing of the article.
Luma supervised the article.
1. Société française d’hématologie (2007) Lymphomes malins non hodgkinien agressifs localisés. Hématologie 13: 320-313.
2. Martelli M, Ferreri AJ, Agostinelli C, Di Rocco A, Pfreundschuh M, et al. (2013) Diffuse large B-cell lymphoma. Crit Rev Oncol Hematol 87: 146-171.
3. Griffiths R, Gleeson M, Knopf K, Danese M (2010) Racial differences in treatment and survival in older patients with diffuse large B-cell lymphoma (DLBCL). BMC Cancer 10: 625.
4. Jang G, Yoon H, Kim S, Lee DH, Lee SW, Huh J, et al. (2011) Addition of rituximab to the CHOP regimen has no benefit in patients with primary extra nodal diffuse large B-cell lymphoma. Korean J Hematol 46: 103-110.
5. Synthèse d’avis de la commission de la transparence (2016) HAS. Hématologie mise au point. Available at: https://www.has-sante.fr/portail/upload/docs/application/pdf/2017-01/dir 1/pixuvri_synthese_ct15478.pdf
6. Organisation mondiale de la santé (OMS) (2014) Statistiques sanitaires mondiales. Genève-Suisse, OMS.
7. Laatiri MA, Elloumi MZ, Ali B, Ben Othmen T, Msadek F, et al. (2010) Tunisian experience in the treatment of aggressive non-Hodgkin’s lymphoma in adults: about 337 patients. Bull Cancer 97: 409-416.
8. Tolo DA, Kouakou B, N'dhatz E, Nanho C, N'Dogomo M, et al. (2012) Characteristics and results of the management of diffuse large B-cell lymphomas: The experience of Cote d’Ivoire. Adv Hematol 945138.
9. Ngouadjeu Dongho E, Tomowiak C, Okalla C, Sume GE, Cazanave M, et al. (2013) Epidemiological profile of blood diseases at the general hospital of Douala-Cameroon from September 2007 to September 2011. Horizon Hématol 3: 48-53.
10. Chauvin S (2012) Macroéconomie et développement. Cameroun: Enjeux de la croissance. Agence française de dévelopement. Available at: http://www.afd.fr/fr/cameroun-les-enjeux-de-la-croissance
11. Banque Mondiale (2017) Cameroun accueil. Available from: http://www.banquemondiale.Org/fr/Country/Cameroon
12. France diplomatie (2017) Présentation du Nigéria: Données générale. http://www.diplomatie.gouv.fr/fr/dossiers-pays/nigeria/presentation-du-nigeria
13. Mounier N, Moral P, Haioun C, Coiffier B, Tilly H, Chatelain C, et al. (1998) Multivariate analysis of the survival of patients with aggressive lymphoma. Variation in the predictive value of prognostic factors during the course of the disease. Cancer 82: 1952-1962.
14. Ngouadjeu Dongho E, Ngo Bayemi RP, Fewou Amadou A, Chetcha Chemeni B, Moueleu Ngalagou T, et al. (2016) Extra nodal lymphoma at the General Hospital of Douala over 6 years: Epidemiological, clinical and therapeutic aspects. AJIH 6: 49-53.
15. Goff J, Nicholas JC (2001) Virus Epstein Barr et système immunitaire. RFL 377: 33-40.
16. Abdelhamid T, Samra M, Ramadan H, Mehessin M, Mokhtar N (2011) Clinical prognostic factors of diffuse large B cell non-Hodgkin lymphoma: a retrospective study. J Egypt Natl Cancer Inst 23: 17-24.
17. Kikkeri N, Raphael M, Ayers L, Hurtwitz N, Calbi V, et al. (2011) Lymphomas in sub-Saharan Africa – What can we learn in improving diagnosis, managing patients and fostering translational research? Br J Hematol 154: 696-703.
18. Le Guyader-Peyrou S, Orazio S, Dejardin O, Maynadie M, Troussard X, et al. (2016) Factors related to diffuse large B-cell lymphoma relative survival in a population-based study in France: Is there a role of socio-economic status? Hematol 152918.
19. Li X, Liu Z, Cao J, Hong X, Wang J, et al. (2012) Rituximab in combination with CHOP chemotherapy for the treatment of diffuse large B cell lymphoma in China: A 10 year retrospective follow-up analysis of 437 cases from Shanghai Lymphoma Research Group. Ann Hematol 91: 837-845.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Journal of Alcoholism Clinical Research
- Journal of Clinical Trials and Research (ISSN:2637-7373)