660
Views & Citations10
Likes & Shares
Systemic Lupus Erythematosus is a multisystem connective tissue disease, characterized by a wide variety of clinical features and the presence of numerous auto-antibodies, circulating immune complexes and wide spread immunologically mediated tissue damage. The expression of the disease is greatly influenced by genetic, environmental, dietary, demographic and geographical factors.
Most of the literatures on SLE are from the Western countries. Given the importance of diet, life style, genetic, environmental and racial factors, a change in the clinical profile of the disease should be anticipated in different parts of the world. This article combines the observations made in two well-conducted studies in a tertiary care center in North Kerala and describes SLE as a hematological disease in our sub set of population and on the criteria which we had developed for diagnosing SLE, the Kozhikode Criteria.
INTRODUCTION
Systemic Lupus Erythematosus is a multisystem connective tissue disease, characterized by a wide variety of clinical features, presence of numerous auto-antibodies, circulating immune complexes and wide spread immunologically mediated tissue damage [1]. The expression of the disease is greatly influenced by genetic, environmental, dietary, demographic and geographical factors. Considerable variation has been observed regarding the clinical manifestations of SLE among various geographical regions and ethnic groups. The first case of SLE in India was reported in 1955 [2]. Subsequent studies conducted in different parts of India described the various manifestations in Indian population with SLE.
Race has shown to be a major predictor in the clinical manifestations, serological pattern and morbidity in SLE [3,4]. Being the largest continent, both by area and population, Asia encompasses people of different diet, lifestyles, and socio cultural background with diverse ethnic groups. Diet and life style habits of the Indian population are never comparable to the western practices and standards. Importance of dietary factors is exemplified by an Indian study on Vitamin D levels and SLE [5]. Although a causal relationship could not be established, it was found that people with Vitamin D deficiency have severe disease. Interestingly Vitamin D deficiency is very high among Indians. High melanin concentration in the skin [6], avoidance of sunlight and poor food habits contribute to low levels of Vitamin D 3 in Indians [7], the same are the causes for other diseases as well [8].
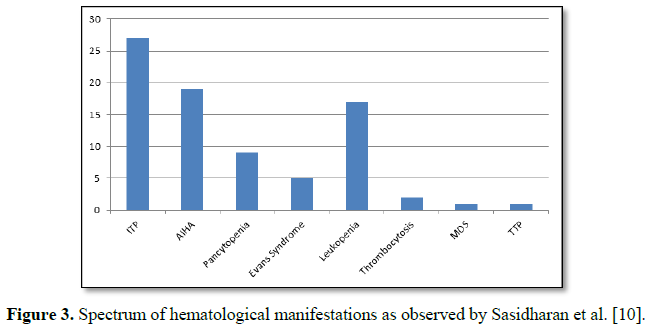
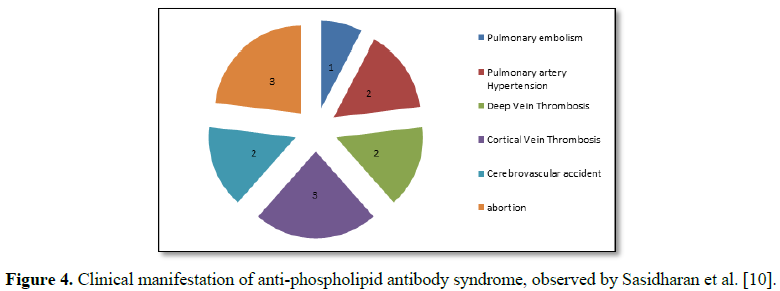
Hematological manifestations of SLE are diverse and are often the presenting manifestation of the disease [9,11,12]. The major hematological manifestations are anemia due to hemolysis, MDS, B12 deficiency, Pure Red cell aplasia; leucopenia due to MDS or aplasia, B12 deficiency, hypersplenism; ITP like presentation and thrombocytopenia due to multiple other causes; Pancytopenia and anti-phospholipid antibody syndrome with its varied presentation like cerebral vein thrombosis, deep vein thrombosis, Budd Chiari syndrome, Pulmonary thromboembolism with its varied presentations (including primary pulmonary hypertension-like presentation).Other manifestations seen are lymphadenopathy and hepatosplenomegaly mimicking lymphoma or leukemia, myelofibrosis, macrophage activation syndrome (HLH), TTP, pure red cell aplasia, MDS, etc., are not uncommon. It has been observed in our studies that SLE presents with hematological manifestations alone, without features of musculoskeletal, dermatological or other system involvement [9]. In almost all these cases presenting with hematological manifestations, it was only because a high index of suspicion that, they were diagnosed and treated early, to the advantage of the patient. The diagnosis in these cases was primarily by good clinical evaluation, looking for evidence of an autoimmune phenomenon and after ruling out other causes. Many such cases, which presented initially with manifestations of autoimmunity in one tissue or organ alone, were ANA negative and did not satisfy the ACR criteria, but did so on follow up [9]. A study from central rural India also showed that the manifestations in SLE were more Hematological and immunological [11]. Two separate studies from South India have shown that mucocutaneous manifestations are less prevalent [12,13]. Taking into account the aforementioned factors, we proposed the need for a practical guideline to diagnose SLE and framed a new criterion named as the Kozhikode criteria [9,10].
Major/essential criteria
1. Presence of an unresolved autoimmune disorder, which is known to occur with SLE (Chronic ITP, Immune hemolytic anemia, autoimmune hypothyroidism and autoimmune hepatitis).
2. No other causes identified, other than autoimmunity, for the said problem, by clinical reasoning and investigations.
Minor criteria
1. Another co existing autoimmune disorder/any other clinical or laboratory evidence of autoimmunity.
2. Positive ANA.
3. Positive anti ds DNA.
4. Sustained and definitive response to steroids and immunosuppressant even after 6 months of follow up.
If the patient has 2 essential and 2 or more minor criteria, they can be diagnosed as SLE.
Our first study was to establish the fact that SLE presents more often with hematological manifestations, and the second study was to establish the validation of the Kozhikode Criteria, both were done in a tertiary care center in North Kerala sequentially [10,14].
MATERIALS AND METHODS
Both the studies were conducted in Government Medical College, Kozhikode, after getting approval from the institutional research committee. The first study was conducted in the year 2009-2010, by Sasidharan et al. [10] and the second one in the year 2013, by Arathi et al. [14]. Both the studies included diagnosed cases of Systemic Lupus Erythematosus, in the Departments of Internal Medicine, Rheumatology, Hematology and Nephrology Departments of Government Medical College, Kozhikode. The studies included already diagnosed cases of SLE and the newly diagnosed cases during their respective study periods. The cases were followed up for a period of one year. There was a considerable overlap in patients in both the studies, since patients already under follow up were included.
Clinical diagnosis of SLE was considered in those presenting with unsettled clinical problems and conditions that were autoimmune in nature, like chronic ITP, hypothyroidism, autoimmune hemolytic anemia, vitiligo, alopecia and all other autoimmune disorders with some laboratory evidences to suggest autoimmunity.
Basic investigations constituting complete blood count, including red cell indices, ESR, renal and liver function tests, urine routine, peripheral smear, ANA, anti-ds DNA were done for all cases. Further investigations like reticulocyte count, Coombs test, ANA profile, radiological tests, tissue biopsy or cytology, including bone marrow, were done in relevant cases. Data was collected using structured personal interview and clinical examination. The first study included patients who satisfied either the ACR criteria or the Kozhikode Criteria. The new criteria was essential, to include those patients who did not satisfy the ACR criteria, but were strongly suggestive of having an autoimmune etiology.
The second study was aimed at validating the Kozhikode Criteria [14]. For this purpose both the ACR and the Kozhikode Criteria were applied to all diagnosed cases of SLE. All newly diagnosed cases that were diagnosed as SLE using the Kozhikode Criteria were also subjected to the ACR criteria. We found that large number of them did not satisfy the ACR criteria, but all of them who satisfied the ACR criteria also satisfied the Kozhikode Criteria. Those who did not satisfy the ACR criteria initially were reviewed after a period of 6 months and the ACR criteria was applied again to see if they satisfied it and thereby to prove whether the Kozhikode Criteria helps in early diagnosis of SLE. In addition, those who were already under follow up were studied by reviewing their clinical features and treatment details and noted whether or not they satisfied the ACR criteria at the beginning and by calculating the average time required to satisfy the ACR criteria.
For assessing the influence of diet and life style, we recruited the caretakers of patients who matched with the cases in age and sex, utilizing a case control design. Dietary information was estimated using the semi quantitative food frequency questionnaire derived from the Integrated Disease Surveillance Project, Non Communicable disease Survey Questionnaire. There were six possible responses, regarding how frequent a particular food item was consumed. The six responses were, nil/less than once in a month, 1-3 times in a month, 1-2 times in a week, 3-4 times in a week, 1-2 times in a day, 3-4 times in a day.
RESULTS
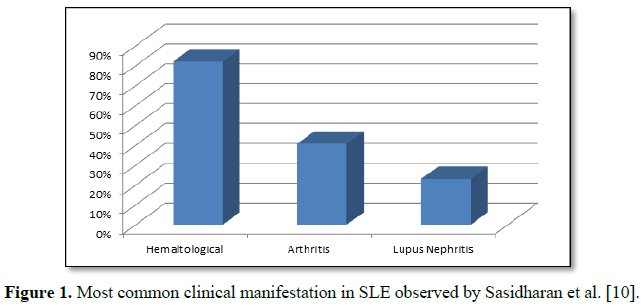
It was seen in both the studies that, a large proportion of cases presented with hematological manifestation as the first symptom (42.69%). There was an inverse relationship between musculoskeletal and hematological manifestations (p value<0.001). There were 10 cases of hypothyroidism and 6 cases of autoimmune hepatitis in the study by Sasidharan et al. [10]. These diseases are not given any representation in the ACR criteria. The most common hematological manifestation was Immune Thrombocytopenic purpura (Figure 3).
Anemia was seen in 62.9% cases. It was multifactorial. It was due to nutritional, autoimmune and anemia of chronic disease.
The commonest manifestation of APLA was Cerebral Venous Thrombosis (CVT) and abortions. Thrombocytopenia was seen in 7 cases of APLA. All the patients had only mild thrombocytopenia that did not warrant any intervention (Figure 4).
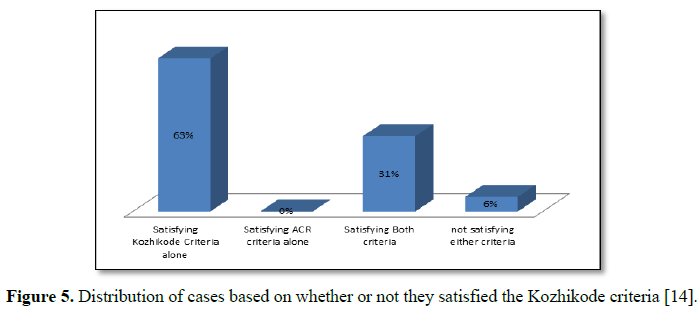
In the study conducted by Arathi et al. [14], for validation of the Kozhikode criteria, there were a total of 71 cases. Out of this 30 were new cases and 41 were previously diagnosed cases of SLE, already under follow up. Of the 71 cases, 45 satisfied Kozhikode Criteria alone, but only 22 satisfied both ACR and Kozhikode Criteria and 4 did not satisfy either criterion. Altogether, 67 patients satisfied the Kozhikode Criteria at the beginning of the study. There was no such group of patients who satisfied the ACR criteria alone but not the Kozhikode criteria, validating the new criterion. Both these observations are highlighting the utility of the new criterion. Out of the 30 new cases, 26 individuals satisfied the Kozhikode criteria, whereas only 6 were satisfying the ACR criteria. The 26 newly diagnosed cases, which satisfied the Kozhikode criteria alone, were followed up for a period of 6 months and it was observed that only 2 of them satisfied the AR criteria at the end of 6 months (Figure 5).
Of the 4 cases which did not satisfy either of the criteria, 2 of them satisfied the Kozhikode criteria at the end of 6 months. One of them had refractory oral ulcers, which subsequently became ANA positive and responded well to steroids. The second patient was a case of alopecia and ITP who responded well to steroids and later became ANA positive. None of the 4 satisfied the ACR criteria even at the end of 6 months. Of the 2 patients who did not satisfy either of the criteria, one patient had refractory oral ulcers and the other patient had lost for follow up.
Among the patients who were already under follow up, it was found that 16 of them who all had satisfied the Kozhikode criteria in the initial diagnosis itself, had satisfied the ACR criteria only during variable periods of follow up as given in Table 1.
The most common clinical manifestation was hematological and it was unusual to see any joint symptom in this sub set. Arthritis was seen in combination with other symptoms but not alone as the initial manifestation. Among the new cases, only two were ANA positive at the time of initial clinical presentation. They were diagnosed and treated as SLE due to strong index of suspicion. Those who were ANA positive were also positive for double stranded DNA. Of the ANA negative patients among new cases, only 2 became ANA positive at 6 months of follow up.
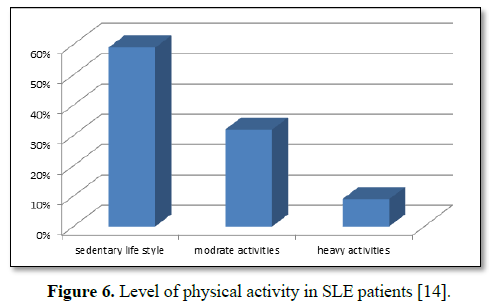
Majority of the patients belonged to moderate socio economic status. Among those diagnosed as SLE, most of them, had a sedentary life style (p<0.05) (Figure 6).
Comparison of diet among cases and controls showed statistically significant decrease in intake of pulses, green leafy vegetables, legumes and fruits (p=0.000). The intake of junk food and canned food was statistically significant among cases than in controls (p=0.000).
DISCUSSION
In both the studies, it was found that hematological manifestations were the commonest and the presenting symptom. This was contrary to the description of the disease in most western books [15,16]. Our findings emphasize the fact that hematological manifestations are a common presenting symptom and may be missed if the index of suspicion is low. Some studies in different parts of the world have evaluated the hematological findings in SLE and the prevalence rates obtained in them are comparable to our observations [17-20]. But hematological manifestations as the initial presentation and its proper inclusion in the criteria for diagnosing SLE were not addressed in any of these studies.
There was a significant inverse relation between the presence of musculoskeletal symptoms and hematological manifestations. The commonly co existing abnormality of autoimmune hypothyroidism in patients presenting with hematological manifestations is under represented in the ACR criteria. No such studies are found in the literature.
Twelve patients in the first study were ANA negative and did not satisfy the ACR criteria and 28 cases in the second study were ANA negative and 24 cases in the second study did not satisfy the ACR criteria. Thus ANA negativity does not rule out SLE in early stages. They all had the clinical diagnosis of possible SLE or evolving SLE at the time of initial presentation itself. In 1982, Mc Hardy and Rennie [21] investigating a cohort of SLE patients in Aberdeen shire, had suggested a prevalence of 8.9% for ANA negative SLE.
Gladman et al. [22] and Ferrerio et al. [23], in two separate studies found that the prevalence of ANA negative SLE was approximately 5%. This emphasizes the importance of relying on individualized clinical judgment rather than on the existing criteria alone for treating the disease and the need for rigorous follow up of all suspected cases, even if they are ANA negative. Based on these observations, Sasidharan et al. [10] proposed the new criteria- The Kozhikode Criteria.
The second study was undertaken to validate the Kozhikode criteria as an alternative to the ACR criteria. The observations of the study has shown the utility of the Kozhikode criteria for early diagnosis of SLE and the observations mentioned are supporting the superiority of the Kozhikode criteria over the ACR criteria for the early diagnosis of SLE. The study has thus validated the Kozhikode Criteria as a useful tool for early diagnosis of SLE.
It was also observed that several of the patients were ANA negative at the time of presentation and they become ANA positive during follow up only. All these patients were clinically diagnosed as SLE or evolving SLE and all of them had satisfied the Kozhikode criteria and not the ACR criteria.
None of the patients were doing exercise on a regular basis. The level of physical activity in the newly diagnosed cases when compared to the controls showed statistically significant decrease in physical activity among the cases. Although there were studies establishing the role of lack of regular exercise and sedentary life style increasing the mortality in SLE, there were no studies relating them to the etiology of SLE [24,25].
The comparison between diets of cases and controls showed statistically significant difference, showing poor intake of pulses, green leafy vegetables and fruits. The intake of junk food, fried meat and canned food was higher among cases than controls, with a significant p value.
The study also observed the following pit falls of the ACR criteria. Hematological manifestations are underrepresented in the ACR criteria. The dietary, life style and ethnicity may be responsible for the higher prevalence of hematological manifestations in our population and the ACR criteria, which were validated on the western population, cannot be applied on our population. SLE can be diagnosed with the ACR criteria only after more than one organ has been involved. Usually it will take years for patients to satisfy 4 out of the 11 criteria and these results in delay in diagnosis and initiation of treatment (Table 2).
1. Laurance J, Wong JE, Nachman R (1992) The cellular hematology of systemic lupus erythematosus. Systemic Lupus Erythematosus. 2nd Edn. Churchill Livingston: New York.
2. Desai SC, Bhadnakar SD (1955) A case report of acute disseminated lupus erythematosus. Indian J Dermatol Venerol 21: 131-134.
3. Tsao BP, Grossman JM (2001) Genetics and systemic lupus erythematosus. Curr Rheumatol Rep 3: 183-190.
4. Siegal M, Lee SL (1973) The epidemiology of systemic lupus erythematosus. Semin Arthritis Rheum 3: 1-54.
5. Mandal M, Tripathy R, Panda AK, Pattanaik SS, Dakua S, et al. (2014) Vitamin D levels in Indian systemic lupus erythematosus patients: An association with disease activity index and interferon alpha. Arthritis Res Ther 16: R 49.
6. Clemens TL, Adams JS, Holick MF (1982) Increased skin pigment reduces the capacity to synthesize vitamin D3. Lancet 1: 74-76.
7. Sasidharan PK (2018) Vitamin D deficiency causes and solutions. J Fam Med Sci 1.
8. Sasidharan PK (2017) Healthy India, untold secrets of health care. Jaypee Brothers: New Delhi.
9. Sasidharan PK (2010) SLE as a hematological problem. Hematology Today, Mumbai: Vikas publications, pp: 953-966.
10. Sasidharan PK, Bindhya M, Sajeeth Kumar KG (2012) Hematological manifestations of SLE at initial presentation: Is it under estimated? ISRN Hematol.
11. Agrawal SR, Tiewsoh I, Rajput AS, Jain AP (2013) A cross sectional hospital based study of clinical and immunological profile of systemic lupus erythematosus patients from central rural India. Indian J Allerg Asthma Immunol 27: 33-37.
12. Binoy JP, Muhammed F, Kumar N, Razia MV (2013) Clinical profile of systemic lupus erythematosus in North Kerala. J Indian Rheumatol Assoc 11: 94-97.
13. Kosaraju K, Shenoy S, Suchithra U (2010) A cross sectional hospital based study of the auto antibody profile and clinical manifestations of systemic lupus erythematosus in South Indian patients. Indian J Med Microbiol 28: 245-247.
14. Arathi N, Sasidharan PK, Geetha P (2016) Kozhikode criteria for diagnosing systemic lupus erythematosus as a hematological disorder. J Blood Med 7: 13-18.
15. Hahn BH (2018) Systemic lupus erythematosus in Harrisons Principles of Internal Medicine. 17th Edn. McGraw Hill: New York, NY, USA.
16. Wallace J, Hannahs B, Francisco P, Quismorio Jr. JR (2006) Dubois lupus erythematosus. 7th Edn. Lippincott Williams and Wilkins: Philadelphia, Pa, USA.
17. Gokce M, Besbas N, Belginer Y, Cetin M, Gumruk F, et al. (2011) Hematological features in children with systemic lupus erythematosus: Are they lupus more common than appreciated? Pediatr Rheumatol 9: 242.
18. Nossent JC, Swaak JG (1991) Prevalence and significance of hematological abnormalities in patients with systemic lupus erythematosus. Q J Med 80: 605-612.
19. Keeling DM, Isenberg DA (1993) Hematological manifestations of systemic lupus erythematosus. Blood Rev 7: 199-207.
20. Beyan E, Beyan C, Turan M (2007) Hematological presentation in systemic lupus erythematosus and its relationship with disease activity. Hematology 12: 257-261.
21. Mc Hardy KC, Horne CH, Rennie J (1982) Anti-nuclear antibody negative systemic lupus erythematosus, how common? J Clin Pathol 35: 1118-1121.
22. Gladman D, Chalmers A, Urowitz MB (1978) Systemic lupus erythematosus with negative LE cells and anti-nuclear factor. J Rheumatol 5: 142-147.
23. Ferrerio JE, Reiter WM, Saldana MJ (1984) Systemic lupus erythematosus presenting as chronic serositis with no demonstrable anti-nuclear antibody. Am J Med 76: 1100-1105.
24. Kathleen J, Berkebile C, Hastings C, Yocum AD (1989) Health status and disease activity in SLE. Arthritis Rheum 2: 65-69.
25. Minami Y, Sazaki T, Arai Y, Kurisu Y, Hisamichi S (2003) Diet and systemic lupus erythematosus: A 4 year prospective study of Japanese patients. J Rheumatol 30: 747-754.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- Journal of Pathology and Toxicology Research
- Journal of Rheumatology Research (ISSN:2641-6999)
- BioMed Research Journal (ISSN:2578-8892)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)