1183
Views & Citations183
Likes & Shares
The primary care physician often is called upon to evaluate the clinical relevance of dermatological cases. Paederus dermatitis is an acute irritant dermatitis resulting from a contact with the hemolymph of Paederus beetles. This dermatitis mimics other infectious skin disorders, often resulting in diagnostic dilemmas, so it is necessary to increase awareness about this condition. We describe a clinical case report that came to our observation.
Keywords: Paedereus, Irritant dermatitis, Skin lesions, Fewer
INTRODUCTION
The general practitioner (GP) has often in his profession way of assessing clinical cases of dermatological interest. The Social changes, the opportunity to travel and to visit large areas of the globe, the migrations now put the GP in the medical conditions to observe certain events that were previously seen only in exotic countries. Paederus beetle exposure can cause health problems. A case of Paederus dermatitis in Sierra Leone is presented to highlight the importance of this clinical entity in the setting of General Medicine of another country. We describe a clinical case report that came to our observation in a primary care setting and subsequently evaluated even in a specialized environment.
CASE PRESENTATION
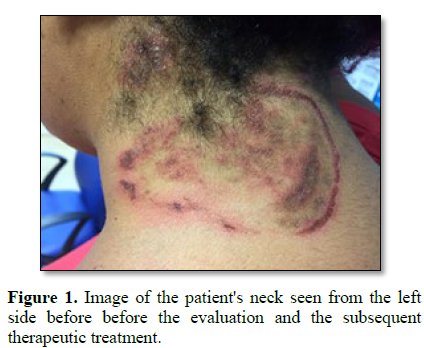
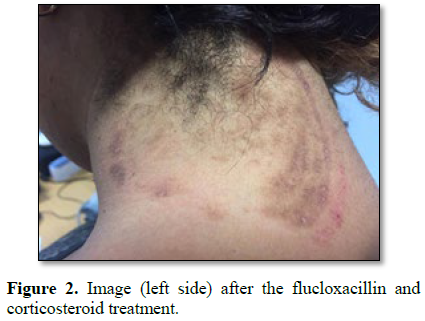
A 32 year old patient came home from a week-long vacation in Sierra Leone. There was nothing relevant in her previous pathological medical history and in her anamnesis. The patient took the contraceptive pill and no other medication. She came to visit referring to presenting about from 8 days a lesion on the neck associated to a high intermittent fever. The fewer was present from the day before, and she was referring to control it with paracetamol. There was also the presence of diffuse arthropathy and nausea (Figure 1). No vomiting and diarrhea. The patient was visited and the objective examination was to find out the presence of a cervical lymphadenopathy bilaterally, normal vital signs, no other associated symptoms. We also noted, in a fairly clear and striking way, the presence of linear reddish lesions giving a whiplash appearance on the neck (almost at the center of the neck as shown in Figure 1), with kissing lesions on the adjacent surfaces of the neck of our subject. She did not remember stings or bites. We initially suspected a symptomatic case of Lyme disease, a rickettsiosis with tache noire and injury by scratching associated given the systemic symptoms and arthromyalgia, a scrofuloderma typical tuberculous or an enlarge impetigo. We rejected the suspected diagnosis of spider bite to the absence of neurological signs and seizures. Blood tests were normal. The patient performed an examination of the scales × bacteria and fungi that was negative. We also reject the suspicion of eczema herpetiformis. In conclusion we place the suspected diagnosis of dermatitis caused by paederus (that it is apparently typical of the Sierra Leone) and the patient discharged with a therapy with flucloxacillin (at the dose of 1 g twice a day) and a topical therapy with hydrocortisone. There was a marked improvement of the lesion to the next control, two weeks away (Figure 2).
DISCUSSION
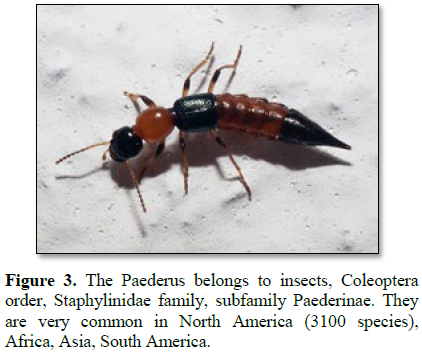
Paederus dermatitis is a self-limiting form of acute irritant contact dermatitis. This irritant dermatitis is caused by the genus Paederus whose geographical distribution is worldwide, with a higher incidence in tropical areas (Figure 3) [1-3]. It is induced by direct skin contact with a molecule called pederin, a blistering and caustic substance found in the abdomen of these beetles and circulating in its hemolymph. Hemolymph is a fluid, analogous to the blood in vertebrates that circulates in the interior of the insect’s body remaining in direct contact with the animal's tissues. Lesions suddenly appear on exposed areas of the body such as the neck (most frequent). Pederin is an extremely toxic substance capable of producing serious and difficult healing injuries to the tissues that come into contact with it. Fortunately, the acute vesicular lesions heal completely in 10-12 days, with a transitory post-inflammatory hyperchromic patch, as shown in figures [4,5]. In severe cases, it can cause neuralgia, artheralgia, fever and vomiting (some of these signs present in the examined patient). The clinical evolution is usually one of uneventful resolution; furthermore, since the lesion was located at the neck level, we did not consider it necessary to proceed with a skin biopsy (also for a possible unsatisfactory aesthetic outcome in a young patient), to assess any ultrastructural damage caused by the pederin (karyorrhexis, karyopyknosis and vacuolization leading to cutaneous necrosis; mitotic figures, chromatin condensation and DNA fragmentation in the basal and suprabasal layers; neutrophilic spongiosis; areas of confluent necrosis and reticular degeneration; perivascular dermal edema), findings that may help in the exclusion of other lesions (e.g. herpetic lesions) and in the differential diagnosis [6-8]. With regard to the treatment of this pathological condition, the cases should be managed as follows: initially wash the affected area with soap and clean fresh water to remove the pederin. Then, application of cold wet compresses. Application of topical steroid (we used topical hydrocortisone) and a use of oral antibiotics in case of secondary infection (which seemed to us in this case). Moreover, in a study of 417 cases the authors observed that topical steroid and antibiotic combination is more effective than topical steroid and topical antibiotic alone [9].
CONCLUSION
Injuries caused by beetles can represent a significant source of lesions. Paederus dermatitis is a well-known problem but it may be not important for some doctors in non-endemic countries. With the climate change the beetle may be seen elsewhere too and not just in the geographic areas where it is usually described. Before you leave for a vacation or a business trip, you should always be aware of the health hazards and diseases of the country that will host us. Similarly, in the evaluation of a vesicular dermatitis in a patient from coming from a geographic area where pedereus may be present, the irritative dermatitis pedereus must be kept in mind. At the current time, in Italy and UK, urgent acute beetle-related injuries are rare and usually involve type I hypersensitivity, and in most cases they are localized lesions that cause discomfort, as in the described case. Timely diagnosis, epidemiological investigation could bring down the incidence of new cases [10].
All the authors contributed equally in the medical management of the patient and in the data interpretation, literature search and writing of the case report.
CONFLICTS OF INTEREST
The authors declare that they have no competing financial interests.
1.
Rahmah E, Norjaiza MJ
(2008) An outbreak of Paederus dermatitis in a primary school, Terengganu,
Malaysia. Malays J Pathol 30: 53-56.
2.
Qadir SN, Raza N, Rahman
SB (2006) Paederus dermatitis in Sierra Leone. Dermatol Online J 12: 9.
3.
Nasir S, Akram W, Khan
RR, Arshad M, Nasir I (2015) Paederus beetles: the agent of human dermatitis. J
Venom Anim Toxins Incl Trop Dis 21: 5.
4.
Vanhecke C, Le Gall P,
Gaüzère BA (2015) Vesicular contact dermatitis due to Paederus in Cameroon and
review of the literature. Bull Soc Pathol Exot 108: 328-336.
5.
Ebrahimzadeh MA, Rafati
MR, Damchi M, Golpur M, Fathiazad F (2014) Treatment of Paederus dermatitis
with Sambucus ebulus lotion. Iran J Pharm Res 13: 1065-1071.
6.
Assaf M, Nofal E, Nofal
A, Assar O, Azmy A (2010) Paederus dermatitis in Egypt: A clinicopathological
and ultrastructural study. J Eur Acad Dermatol Venereol 24: 1197-1201.
7.
Karthikeyan K, Kumar A
(2017) Paederus dermatitis. Indian J Dermatol Venereol Leprol 83: 424-431.
8.
Singh G, Yousuf Ali S
(2007) Paederus dermatitis. Indian J Dermatol Venereol Leprol 73: 13-15.
9.
Gopal KVT (2014) Paederus
dermatitis: A clinical, epidemiological and therapeutic study of 417 cases. J
Evol Med Dent Sci 3: 4736-4743.
10.
Verma CR, Agarwal S
(2006) Blistering beetle dermatitis: An outbreak. Med J Armed Forces India 62:
42-44.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- BioMed Research Journal (ISSN:2578-8892)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Allergy Research (ISSN:2642-326X)