1682
Views & Citations682
Likes & Shares
Background: Swelling over the facial region can be diagnostic challenge for clinician as well as radiologist. But when Pott’s puffy swellings appear in atypical way then this leads to diagnostic dilemma. Tuberculous osteitis can present in similar fashion which can evade early diagnosis. This can proved to be with dangerous consequences if it is communicating or creating any complications in the intracranial region.
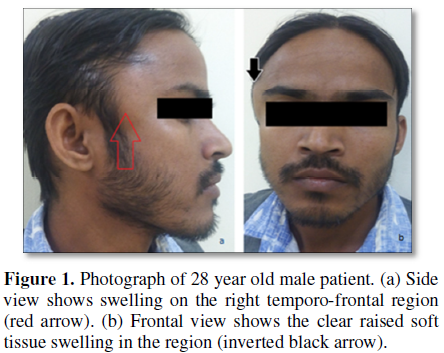
Case presentation: 28 years old male presented with non-tender swelling in the right temporo-frontal region. The detailed investigations with plain radiography, ultrasonography (USG), contrast enhanced computerized tomography (CECT) and magnetic resonance imaging (MRI) was required for the evaluation. The diagnosis was confirmed as Pott’s puffy tumor but of tuberculous etiology with epidural-subcutaneous fistula and abscess. Fine needle aspiration cytology (FNAC) was carried out in confirming the diagnosis.
Conclusion: Swelling in the frontal and adjoining regions of the skull can be quite confusing for clinching the diagnosis. The appropriate management should be contemplated without harming the intracranial structures. In our case anti-tuberculous treatment was started without any surgical intervention for the management.
Keywords: Pott’s puffy swelling, Tuberculous osteitis, USG, CECT, MRI, FNAC
Any swelling in the facial region poses initial diagnostic problem because of their silent nature especially of tuberculous in origin. Pott’s puffy tumor is the swelling in fronto-lateral region of the head due to sub periosteal abscess in relation to underlying osteomyelitis. This was named after the leading surgeon Sir Percivall Pott in 1760. The original case was reported following trauma and the same was attributed due to underlying sinus infection [1]. The entity is predominantly seen in the forehead which is because of the underlying frontal sinusitis. But sometimes many other pathologies can have the same imaging features which require accurate evaluation and correct diagnosis [2].
CASE REPORT
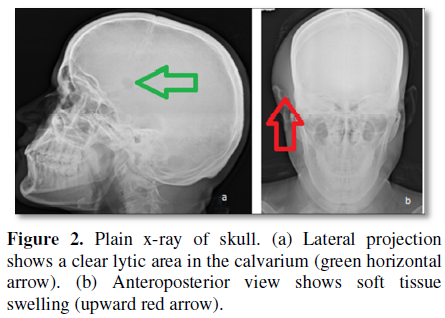
There was mild pain in the region with the movement of jaw. There was no history of trauma or any of previous surgery. On examination the patient was of average built without any disability. Locally the swelling was present on the right temporo-frontal region and measured 3.2 × 4.1 cm in size. The swelling was non tender, fluctuant and non-pulsatile. There was no discoloration of the overlying skin. Systemic examination was non-contributory. Investigations revealed hemoglobin 12 g%, erythrocyte sedimentation rate (ESR) 50 mm fall in 1st hour, total lymphocytic count (TLC) 8600/cm, differential lymphocyte count P54, L40, M02, E4. Urine examination did not show any abnormality. Plain x-ray skull was conducted as initial work up. The radiograph had revealed soft tissue swelling with an osteolytic lesion on the inferior aspect of the coronal suture on right side (Figures 2a and 2b).
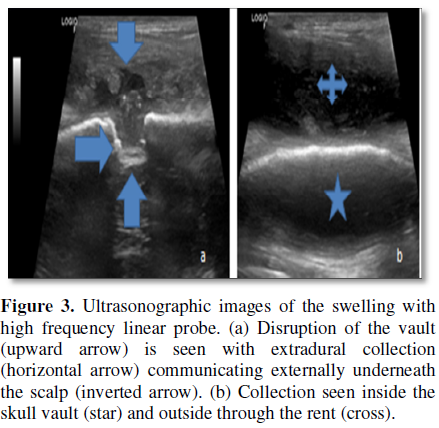
Further work up was done by sonographic examination. It revealed collection underneath the thickened scalp with intracranial communication (Figures 3a and 3b).
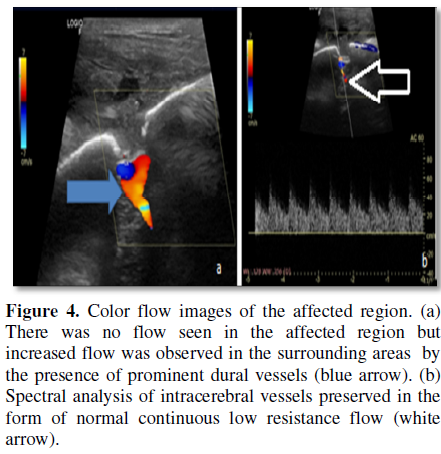
There were multiple prominent dural veins seen in colour flow imaging (Figures 4a and 4b).
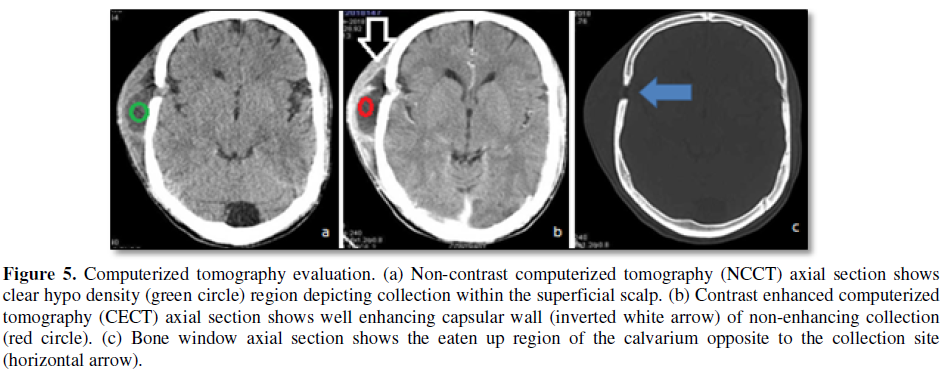
CECT was done which had revealed the greater anatomic details with epidural collection. This had shown enhancing capsular wall with a few septations (Figures 5a-5c).
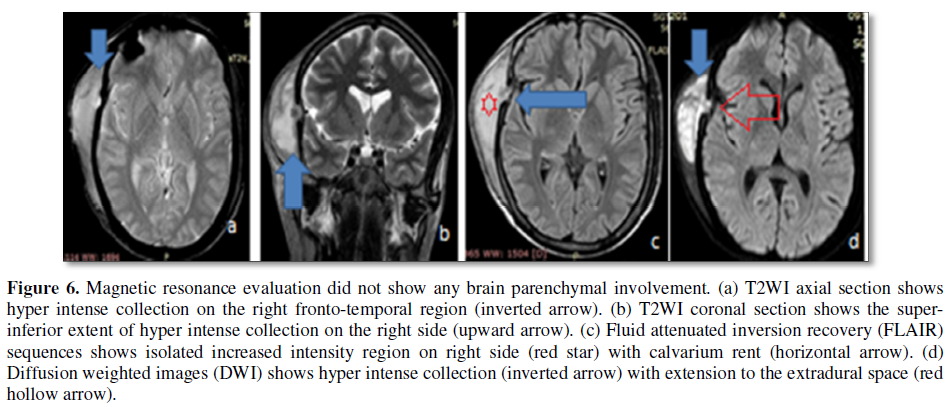
MRI was also done to see the soft tissue details and the brain parenchyma with standard protocol sequences (Figures 6a-6d).
The working diagnosis was kept as Pott’s puffy tumor as per the clinical setting and the radiological investigations. Fine needle aspiration confirmed the diagnosis as that of tuberculosis origin aetiology. No surgical intervention was contemplated because of the morphology of the lesion and corresponding FNA cytology. Patient had been put on anti-tuberculosis therapy (ATT) and had been called for the follow up after four weeks.
DISCUSSION
Tuberculous osteitis of the skull is a very rare phenomenon and it becomes more in rarity when present as Pott’s puffy tumor [3,4]. These accounts for just 1% of skeletal tuberculosis. This is common in developing countries because of the poor socioeconomic status and malnutrition [5]. Other factor which plays a great aetiopathological role is immunodeficiency syndromes. The first case of skull tuberculosis was reported in 1942 [6]. In 1981, scientists had reviewed 220 cases of skull tuberculosis. Mohanty et al. [7] also reported 40 cases of calvarial tuberculosis in 1981. The pediatric group is affected the most and majority of all fall below 20 years of age. There may or may not be the discharging sinus which communicates to the underlying abscess. Soft tissue swelling is because of underlying cold abscess [8]. The skull lytic lesion can be confused with either multiple myeloma or metastatic disease. The parietal bone is the most affected bone. Sutural junctions are the still rarest as was in our present case. The superficial scalp swelling can also be evaluated by USG and color flow imaging (CFI) [9]. The surrounding vascularity and the communication can be evaluated by this modality. The lytic lesion seen in plain radiography requires further evaluation by CECT and MRI studies [10]. CECT shows a well-defined defect with the bone destruction and intracranial involvement of brain parenchyma [11,12]. The extradural collection is seen with thick enhancing capsular tissue. There may or may not be the combination of underlying abscess with the discharging sinus. Scintigraphy is superior to CT scan for diagnosis and delineation of the lesion [13]. There should be meticulous approach for the management .Surgical opinion is must for the intracranial complications and sinus pathology. There may be requirement of the sinus drainage as per the involvement. Anti-tuberculous therapy may be started as early as possible to avoid further drainage to the intradural structures [14].
CONCLUSION
Calvarial tuberculosis is rare in presenting as Pott’s puffy tumors. This requires thorough worked up by the cross sectional modalities like CT and MRI. The scalp swelling may be misleading because of not causing many symptoms. It is important to know the intracranial extension of the collection or the pathological process which is very essential in surgical management point of view. Scalp swelling with bone destruction is less likely to cause any intracranial manifestations.
ACKNOWLEDGEMENT
We are extremely thankful to Miss Sadaf Jaffar BRIT student, Faculty of Allied Health Sciences for helping us in diagnostic support. We are also thankful to Mr. Prahlad Singh, Mr. Kasif and Mr. Anil Kumar radiographers of SGT Hospital for carrying out general radiography and CT.
CONSENT OF THE PATIENT
Written consent of the patient was taken.
CONFLICT OF INTEREST
There is no conflict of interest.
ETHICAL ISSUE
Nil
1. Keteni I, Unlu Y, Tucer B, Vural A (2011) The Pott’s puffy tumor: A dangerous sign for intracranial complications. Eur Arch Otorhinolaryngol 260: 1755-1763.
2. Mukherjee KK, Kaushik R, Nada R, Khosla VK, Khandelwal N, et al. (2002) Calvarial tuberculosis. Surg Neurol 57: 195-202.
3. Jadhav RN, Palande DA (1999) Calvarial tuberculosis. Neurosurgery 45: 1345-1348.
4. Allison JW, Abernathy RS, Figrola MS, Tonkin IL (1999) Tuberculosis osteomyelitis with skull involvement. Radiographics 160: 552-554.
5. Davidson L, McComb LG (206) Epidural-cutaneous fistula in association with the Pott puffy tumor in an adolescent. Case report. J Nerosurg 105: 235-237.
6. Tyagi AK, Kirollos RW, Kang NV (1996) Tubercular osteitis of the skull: A case report and review of the literature. Br J Neurosurg 10: 399-401.
7. Le Roux PD, Griffin GE, Marsh HT, Winn HR (1990) Tuberculosis of the skull - A rare condition: Case report and review of the literature. Neurosurgery 26: 851-855.
8. Mohanty S, Rao CJ, Mukherjee KC (1981) Tuberculosis of the skull. Int Surg 66: 81-83.
9. Wohaibi M, Russel NA, Omojola M, Feriyan A (2000) Tuberculosis of the skull. J Neurosurg 92: 1065.
10. Vanderveken OM, De Smet K, Dogan-Duyar S, Desimpelaere J, Duval ELI, et al. (2012) Pott’s puffy tumour in a 5 year old boy: The role of ultrasound and contrast enhanced CT imaging: Surgical case report. B ENT 8: 127-129.
11. Acke F, Lemmerling M, Heylbroeck P, De Vos G, Vestraete K (2011) Pott’s puffy tumor: CT and MRI findings. JBR-BRT 94: 343-345.
12. Raut AA, Nagar AM, Muzumdar D, Chawla AJ, Narlawar RS, et al. (2004) Imaging features of calvarial tuberculosis: A study of 42 cases. AJNR Am J Neuroradiol 25: 409-414.
13. Uren RF, Howman-Giles R (1992) Pott’s puffy tumor, scintigraphic findings. Clin Nucl Med 17: 724-727.
14. Fedre HM Jr, Cates KL, Cementina AM (1987) Pott puffy tumor: A serious occult infection. Pediatrics 79: 625-629.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Allergy Research (ISSN:2642-326X)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Journal of Pathology and Toxicology Research
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- International Journal of Diabetes (ISSN: 2644-3031)