601
Views & Citations10
Likes & Shares
INTRODUCTION
A child with diffusely enlarged tongue due to lymphangioma presents a
unique challenge to the anesthesiologists. Anesthetic concerns include
difficulty in mask ventilation, intubation, bleeding, extrinsic and intrinsic
pressure on the airway causing distortion and enlarged upper Anesthetic
management is often challenging in such patients because of difficult mask
ventilation and airway management. We report a case of lymphangioma of tongue
leading to macroglossia in a child. Anesthetic concerns including airway
management, alternative airway equipment and possible complications are
discussed.
CASE
REPORT
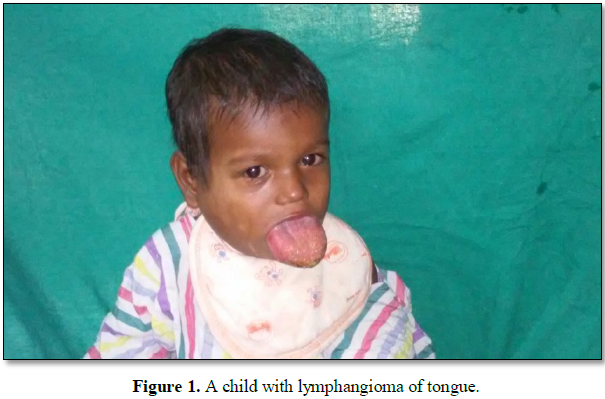
A 2 year old male child weighing 10 kg reported to pediatric surgery with
generalized swelling of tongue. Parents noticed a pea sized swelling over
tongue immediately after birth. They consulted some private physician and took
some medicines but no response was observed. Increase in size of the swelling
was insidious. Child was delivered at full term in a village hospital. There
was no significant antenatal history. Parents gave a history of progressive
difficulty in feeding the child but there was no breathing difficulty. Local
examination revealed an enlarged tongue protruding and keeping the mouth
permanently open (Figures 1 and 2). The oro-dental hygiene was poor with
teeth impressions on the surface of tongue. Mouth opening, inter-incisor gap
and Mallampatti grading could not be elicited due to the enlarged tongue. On
palpation the tongue was non tender and firm in consistency. Patient had a
swelling of 2 × 4 cm in right parotid region raising the ear lobe. No other
congenital abnormalities were present. All routine investigations were with in
normal limits. Ultrasound showed hypertrophy of tongue with multiple cystic
areas seen in parotid and submandibular gland. Magnetic resonance imaging
revealed enlargement of tongue in anterior 2/3 region and hyper intensity on
T2W and T1W images. It showed heterogeneous enhancement on CEMR. Lymphangiomas
seen in bilateral parotid and submandibular glands with enlarged right parotid
gland. Rest of the systemic examination was normal. Child was pre-medicated
with intranasal midazolam 0.5 mg 30 min prior to shifting to the operation
theatre. On arrival to the operating room, routine monitors, including a pulse
oximeter, non-invasive blood pressure cuff and electrocardiographic monitor
were applied. Difficult airway cart, and tracheostomy set were arranged. Suture
was kept ready. It was planned to pull the tongue with suture if obstruction
occurred. Child was induced with sevoflurane 2-6% in increments using size 3
transparent facemask (Figure 3). We used bigger size face mask, i.e.,
size 3 to oxygenate and ventilate the patient, as we were unable to maintain
proper seal with smaller mask because of large protruding tongue. It was
difficult to assist ventilation in supine position so he was turned to right
lateral position. Intravenous line was secured with 24 G cannula in right hand.
Injection glycopyrrolate 50 µg and fentanyl 20 µg were given IV. After checking
for ability to ventilate, check laryngoscopy done and succinylcholine 20 mg
given IV. Child was successfully intubated orally with 4.5 mm uncuffed tube in
a single attempt. Anesthesia was maintained with N2O 67%, oxygen
33%, isoflurane 1% and atracurium. Injection paracetamol 150 mg IV,
hydrocortisone 20 mg IV was given intraoperatively. The inverted V shaped
anterior half of the tongue was removed. The tumor had large cystic spaces
filled with lymph like fluid. After completion of surgery, trachea was
extubated without any adverse event. The intra-operative and recovery period
were uncomplicated and baby was shifted to the ward after being observed for 2 h in the
recovery room. Child’s
DISCUSSION
Lymphangiomas are
hamartomatous, congenital malformations of the lymphatics. They result from
sequestration of lymphatic tissue that has retained its potential for growth
and do not communicate with other lymphatic tissue [1]. Lymphangioma can be
classified into four categories: Lymphangioma simplex (lymphangioma circumscriptum):
composed of small, thin-walled lymphatics. Cavernous lymphangioma: comprised of
dilated lymphatic vessels with surrounding adventitia. Cystic lymphangioma
(cystic hygroma): consisting of huge, macroscopic lymphatic spaces with
surrounding fibrovascular tissues and smooth muscles. Cervical lesions in a
child can cause dysphagia and airway obstruction which is rare in adults [2].
The anterior
two-thirds of the dorsal surface of tongue is the most common site for
intra-oral lymphangiomas leading to macroglossia [3]. These patients tend to
have speech disturbances, poor oral hygiene and bleeding from tongue associated
with oral trauma [4]. In the present case, the swelling was noticed since birth
and reached the current size as appropriate treatment was not taken.
Macroglossia resulted in lesions on the dorsal surface of tongue, improper
phonation and poor oral hygiene.
Awake intubation
may be a first option but is not easily performed in children since cooperation
is quiet essential. Adult fiber optic bronchoscopes (FOB) have an outer
diameter of around 3.5-4.0 mm and thus can take realistically a size 4.0-4.5 mm
endotracheal tube loaded onto them. Ultra-thin fiberoscopes have an outer
diameter of 2.2 mm so a 2.5 mm endotracheal tube can be railroaded over them.
The optical quality of these scopes is good but it has no suction channel and
secretions have to be aspirated with a suction catheter [3]. Though an ideal
technique, pediatric bronchoscopic intubation is time consuming and requires
expertise, skill and expert assistance proper size of FOB, smooth inhalational
induction, deep plane of anesthesia and maintenance of spontaneous ventilation
[5]. We did not use fiberoptic bronchoscope in our case due to non-availability
of appropriate size FOB at our setup.
Premedication and
pre-oxygenation should be followed by inhalation with either halothane or
sevoflurane in a spontaneously breathing patient. It is better to withhold
muscle relaxants until the airway is secured. Use of a muscle relaxant during
induction of anesthesia may result in a difficult to ventilate and difficult to
intubate situation. Intubation should be performed under deep inhalational anesthesia.
Intravenous versus inhalational induction should be discussed. Cooperation of
the child and support of the parents will be a factor in the induction
decision-making process. In our case we experienced difficulty in ventilating
the child in supine position, but with larger mask and turning patient in right
lateral position, we were able to ventilate the child.
The laryngeal mask
airway in pediatric patients with difficult airway is an excellent aid and can
be used as a conduit for intubation. Video laryngoscopes are new addition to
airway armentarium. A variety of video laryngoscopes like King Vision is
available for use in pediatric difficult airway and is a good alternative to
fiberoptic bronchoscope as a first choice.
Pediatric airway
management poses unique challenges to the anesthesiologist. Anesthesia for the
child with lymphangioma involving the oral cavity and oropharynx requires
thorough preparation and vigilance. Knowledge of the disease and the affected
airway structures will help the anesthesia provider prepare for the case by
having the correct equipment and the safest plan for the anesthesia.
1.
Morley SE, Ramesar KC, Macleod
DA (1999) Cystic hygroma in an adult: A case report. J R Coll Surg Edinb 44:
57-58.
2.
Chappius IIP (1995) Current
aspects of cystic lymphangioma in the neck. Arch De Pediatre 1: 186-92.
3.
Tewari A, Munjal M, Kamakshi,
Garg S, Sood D, et al. (2009) Anesthetic consideration in macroglossia due to
lymphangioma of tongue: A case report. Indian J Anesth 53: 79-83
4.
Guelmann M, Katz J (2003)
Macroglossia combined with lymphangioma: A case report. J Cli Pediatr Dent 27:
167-170.
5.
Pethkar TS, Malde AD (2011)
Anaesthetic management of cystic hygroma of tongue in a child. J Anaesth Clin
Pharmacol 27: 421-423.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)