699
Views & Citations10
Likes & Shares
Management
of difficult airway is widely recognized as one of the serious challenges of
the anesthesiologists. The complications related to it are known to be life
threatening. One of the difficult airway scenario is fused cervical and atlanto
occipital joints. Awake fibreoptic intubation remains the gold standard for
such situations. Herewith, we present such a case where we faced difficulty in
doing awake fibreoptic bronchoscope because of fixed c-spine and lateral head
tilt due to skeletal tuberculosis and overgrowth of pharyngeal soft tissue. We
were able to successfully intubate the patient after changing the position of
anesthetist from behind the head of patient to sideways and manipulating the
scope. He was a known case of skeletal tuberculosis and ankylosing spondylosis.
His head was fixed in permanent left lateral tilt with nil neck movement. Most
airway problems can be fixed with available gadgets and techniques but clinical
judgment, experience and expertise is required to implement these tools in any
difficult airway scenario.
Keywords: Fibreoptic intubation, Saygo – spray as you
go, Atlanto-occipital joint, FOB (fibre-optic bronchoscope)
INTRODUCTION
Airway management in cervical spine abnormality is of paramount
importance for an anesthesiologist. Fibreoptic intubation seems to be a boon in
difficult airway cases [1]. In our patient we encountered difficulty in doing
fibreoptic intubation due to anatomical and bony changes as the patient had
past history of skeletal tuberculosis and ankylosing spondylitis. Tubercular
osteomyelitis and arthritis arises from reactivation of bacilli lodged in bone
during the mycobacteremia of primary infection. Tuberculous arthritis is a
consequence of extension of an initial infectious focus from the bone to the
joint [2]. In nearly 50% of the cases tubercular vertebral osteomylitis
commonly affects the thoracic or thoracolumbar segments, this is followed by
lumbar segments and to lesser extent cervical segment [3]. Paraplegia,
quadriplegia, joint destruction and joint fusions are complications which
warrant anesthesiologist’s attention [4].
CASE
REPORT
45 years old, 75 kg male with BMI 29 kg/m2 was posted for open
cholecystectomy. He had history of pulmonary and skeletal TB for which he
completed ATT 2 years ago. He is an also a K/C/O HTN since 3 years, on T.
Amlodipine 10 mg OD. His blood pressure was well controlled. He underwent THR
for frozen hip 2 years ago; he gave history suggestive of awake laryngoscopy on
O.T. table. His rest of the surgical and anesthetic history was uneventful.
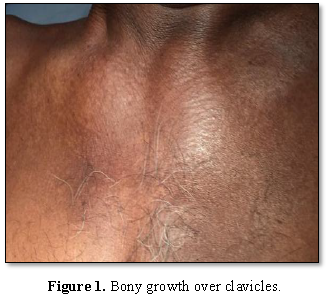
O/E – multiple fused joints were observed including shoulder, cervical
and atlanto-occipital joints. His head was permanently fixed in left lateral
tilt. Multiple bony overgrowths were observed all over the body including over
the clavicles (Figure 1). He was unable to lie flat due to fixed
cervical spine deformity (Figure 2).
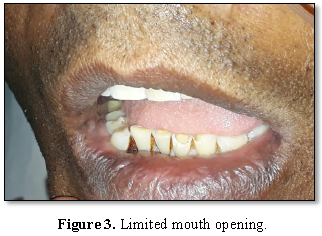
Airway
examination:
·
Nasal patency: left>right
·
Mouth opening: <2 fingers (Figure 3)
·
TMD<6.5 cm
·
Neck movement: Nil (no
extension, flexion or lateral rotation)
·
Investigations: Within normal
limits
·
Chest X-Ray: Pleural thickening
along with right tracheal deviation
·
X-ray cervical spine (lat):
Fusion of cervical vertebrae with absent atlanto-axial gap
·
He was kept NPO for 8 h, tab
Ranitidine 150 mg at bed time and coming morning and tab. clonazepam 0.5 mg at
bed time was advised. Informed high risk consent was obtained in view of
difficult airway and tracheostomy if needed.
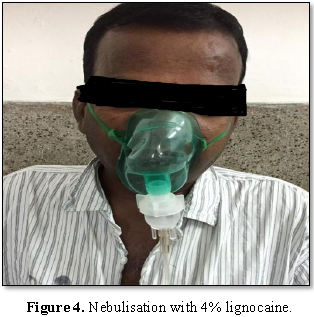
We planned for
awake oral fibreoptic intubation. I.V. line was secured and inj. glycopyrrolate
0.2 mg was given 30 min prior. Xylometazoline nasal drops were used for nasal
mucosa vasoconstriction. Total dose of lignocaine was calculated according to
body weight and half of the dose was kept for SAYGO and rest was used for
nebulization and other blocks [5]. Patient was nebulized with 2 ml of 4%
lignocaine diluted to 5 ml with NS for 30 min (Figure 4). Cotton pledgets soaked in 2% lignocaine were used to
block glossopharangeal nerve. 10% xylocaine spray was used to spray both
nostrils and tongue. Injection dexmedetomidine 0.25 mcg /kg/min was started 15
min prior to procedure. Patient was taken to O.T.; standard ASA monitoring was
started with recording of baseline parameters. Patient was explained the
procedure on table. Oxygen through nasal cannulae @4 L/min was started.
Fibreoptic scope was introduced through the mouth, structures were visualized
but epiglottis was not seen. Multiple pockets of pharyngeal soft tissues were
seen and were very confusing, on searching for epiglottis for 5 min, it was
finally seen extremely pushed towards right side. But it was not possible to go
beyond epiglottis as it was closely approximated to posterior pharyngeal wall
and could not be centralized.
We changed our
plan and went for nasal fibreoptic intubation. A rubber catheter lubricated
with xylocaine jelly was inserted through left nostril and found to be patent.
The FOB was inserted and epiglottis was seen in extreme right. 2-3 ml of 2%
xylocaine was sprayed over epiglottis. We changed our position by standing on
left side of patient and asked the patient to stick out his tongue and with
great difficulty and maneuvering posterior part of vocal cords were seen (Figure 5). 2 ml of 2% xylocaine was
sprayed over vocal cords. After waiting for 30 s FOB scope was advanced and
trachea was intubated (Figure 6).
After confirmation of bilateral air entry Injection propfol 120 mg and
injection vecuronium 6 mg was given. It took about 12 min to intubate the
patient (Figure 7). Our patient was
maintaining 99% SPO2 and was calm and cooperative throughout the
procedure.
DISCUSSION
Awake fibreoptic
laryngoscopy like direct laryngoscopy may prove to be difficult or even
impossible. Ovassapian has classified the causes of difficult fibreoptic
intubation as [6]:
1.
Distorted airway anatomy (mass, hematoma, previous
surgery or radiation therapy)
2.
Secretions or blood
3.
Decreased space between tip of epiglottis and
posterior pharyngeal wall
4.
Reactive airway (inadequate topical anesthesia)
The reasons for
decreased space between tip of epiglottis and posterior pharyngeal wall are:
a)
Large floppy epiglottis
b)
Elevation of floor of the mouth and tongue as a
result of edema and cellulitis
c)
Obesity (OSA)
d)
Displacement of larynx secondary to severe flexion
deformity of cervical spine
e)
Supraglottic mass causing dorsiflexion of the
epiglottis
Our case could be
classified into 3 groups. Our patient had a fixed craniocervical junction with
absent atlanto-axial gap on a lateral radiograph, a finding which has positive
predictive value of more than >70% for grade 3 laryngoscopy [7].
We opted for awake
fibreoptic intubation because the technique described is associated with
cardiovascular stability, low incidence of hypoxemia and reasonable degree of
patient acceptance [8]. In addition awake fibreoptic is recommended not only
because of possible difficulties in visualizing vocal cords but because
forcible manipulation of neck under GA may cause cervical # or vertebrobasilar
insufficiency [9]. Advantage of awake intubation is that failure does not
endanger the patient. So, it can be regarded as most promising technique in
difficult airway [10,11].
CONCLUSION
1.
Adequate preparation is the key to a successful
awake fibreoptic intubation in deformities of cervical spine.
2.
Changing the position of anesthetist from just
behind the back of head of patient to contralateral position may improve the
view.
3.
Introducing the scope slightly away from midline can
lead to visualization of cords in cases where trachea is shifted.
4.
External manipulation of larynx can help in cases of
tracheal shifting.
5.
In cases where there is decreased or no space
between tip of epiglottis and posterior pharyngeal wall, asking an awake
patient to stick out his tongue can help to facilitate fibreoptic intubation.
1.
Committee on Standards and
Practice Parameters; Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, et al. (2003)
Practice guidelines for management of difficult airway. An updated report by
ASA Task Force on Management of the Difficult Airway. Anesthesiology 98:
1269-1277.
2.
Gardam M, Lim S (2005)
Mycobacterial osteomyelitis and arthritis. Infect Dis Clin N Am 19: 819-830.
3.
Jain AK (2010) Tuberculosis of
spine. J Bone Joint Surg (Br) 92B: 905-913.
4.
Mateo L, Ruiz J, Olive A,
Manterola J, Perez R, et al. (2007) Tuberculosis osteoarticular. Med Clin
(Barc) 129: 506-509.
5.
Sidhu VS, Whitehead EM,
Ainsworth QP, Smith M, Calder I, et al. (1993) A technique of awake fibreoptic
intubation - Experience in patients with cervical spine diseases. Anesthesia
48: 910-913.
6.
Ovassapian A (1990) Fibreoptic
intubation. In: Ovassapian A. ed. Fibreoptic airway endoscopy in anesthesia and
critical care. New York: Raven Press, pp: 57-59.
7.
Calder I, Calder J, Crockard HA
(1991) Radiological prediction of difficult intubation: The C0-1 and C 1-2
gaps. Anesthesiology 75: A190.
8.
Smith M, Calder I, Cockard A,
Isert P, Nicol ME (1992) Oxygen saturation and cardiovascular changes during
fibreoptic intubation under general anesthesia. Anesthesia 47: 158-161.
9.
Sinclair JR, Mason RA (1984)
Ankylosing spondylitis. The case for awake intubation. Anesthesia 39: 3-11.
10.
Benumof JL (1991) Management of
difficult airway. Anesthesiology 75: 1087-1110.
11.
Randolph H, South K (1993)
Neurologic deterioration associated with airway management in a cervical spine
injured patients. Anesthesiology 78: 580-583.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Oncology Clinics and Research (ISSN: 2643-055X)
- Dermatology Clinics and Research (ISSN:2380-5609)
- International Journal of AIDS (ISSN: 2644-3023)
- Journal of Alcoholism Clinical Research
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)