928
Views & Citations10
Likes & Shares
Background: The Recurrent Respiratory papillomatosis (RRP) is a laryngeal disease induced by the Human Papilloma Virus (HPV) in the respiratory or phonatory epithelium. The evolution of each patient is uncertain and despite the surgical treatment there is a high risk of recurrence.
Objective: Identify HPV types in RRP patients, point clinical outcomes and compare them between groups to assess the individual prognosis of each subtype.
Methods: Descriptive and retrospective study of 34 patients with RRP submitted to surgery for excision of papillomas. Polymerase chain reaction (PCR) tests were performed for molecular identification of HPV types with questionnaires from medical records for each patient. Correlations were made through statistical analysis.
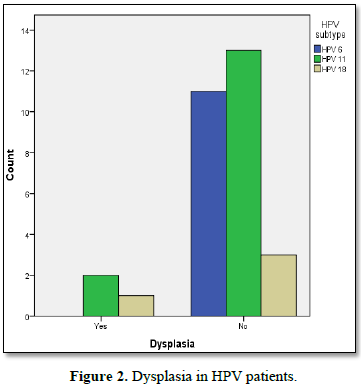
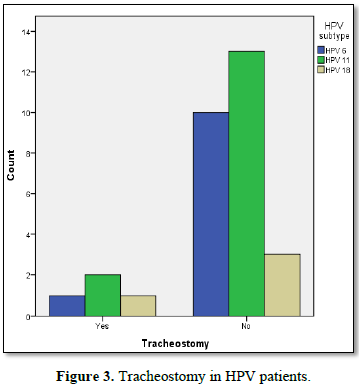
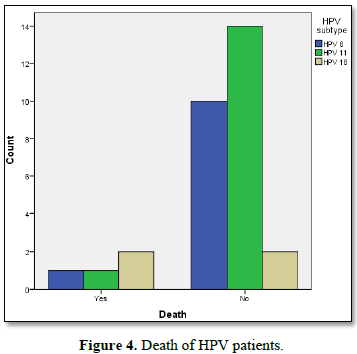
Results: From the 34 collected samples, 4 didn’t amplified by PCR. Among the remaining 30, 15 (50%) were HPV 11, 11 (36.3%) of HPV 6 and 4 (13.7%) of HPV 18. No type 16 was found. Men were 60% of patients and women 40%. The incidence of dysplasia was 10% of cases and mean age at diagnosis was 19.73 years. There were no statistically significant differences between groups HPV 6, 11 and 18 to the outcomes dysplasia, tracheostomy, number of surgeries, age at diagnosis, duration of disease and surgeries per year of disease. Mortality was statistically higher in the group HPV 18.
Conclusion: The most prevalent HPV types in our patients were HPV 11 and HPV 6. The HPV 18 had a tendency to proportionally worse clinical outcomes and more aggressive disease, being also statistically was more related to the occurrence of death. Larger studies should be encouraged to research the statistical correlations of patient prognosis and HPV types.
INTRODUCTION
In most cases RRP is presented as multiple lesions affecting the supraglottis, the commissure and the anterior one-third of vocal folds. In the presence of first symptoms patients show alteration on vocal quality, dyspnea, stridor, cough or recurrent respiratory infections. With a bimodal age pattern, the outset of symptoms varies and may start at early childhood, after 5 years, or later in young adults between 20 and 40 years old.
Diagnosis is carried out through the patient history and clinical suspicion associated to laryngoscopy or nasofibroscopy for visualization and confirmation through a biopsy of the lesions.
The disease progression is uncertain and it may evolve quickly to a respiratory failure, remain stable for years, or even regress spontaneously. However in most of the cases it is persistent and recurrent. Standard RRP treatment consists on the surgical removal of neoplastic buds from the airways. The most commonly used technique is the cold excision of the papillomas through micro-surgery. Other options of treatment include microdebridment and CO2 laser ablation. Since the disease has a high recurrence index new studies point out alternatives to control the disease through the use of interferon, cidofovir, podophyllin, hormones among others. According to Kayode [1] and Avelino et al. [2,3], cidofovir and interferon have presented better results lowering the number of surgical retreatment per year; however there is still no consensus on a standardized treatment.
It is extremely important to perform a biopsy of the lesions in all patients in order to confirm the diagnosis and exclude malignancy. The genotyping of HPV is carried out using the samples collected for the biopsy. The types of the virus that causes this disease can be identified through sensitive and reliable tests such as: in situ hybridization, hybrid capture and polymerase chain reaction (PCR).
So far more than 100 subtypes of HPV have been described. HPV is still divided into three classifications: low risk (HPV 6 and HPV 11), medium risk and high risk of malignancy (that includes HPV 16 and 18). In RRP the most prevalent HPV types are 6 and 11, corresponding to something around 80% to 90% of these patients. The number of patients with HPV 16 and 18 is the lower one, ranging from 0 to 20% from patients, according to literature [1-3].
Thus knowledge on HPV types involved in RRP is important in order to determine prophylactic and therapeutic approaches for these patients, including immunization against diseases caused by HPV.
Therefore the aim of this study was to identify HPV types in patients with RRP through PCR method and report their clinical outcomes and correlate them statistically in order to assess the prognosis of each type.
METHOD
This is a retrospective descriptive study carried out from August of 2008 to November of 2015, at the Otorhinolaryngology Clinic from the Hospital de Clínicas of the Federal University of Paraná – Brazil (HC-UFPR). The material collected from 34 patients with suspected or diagnosed RRP at the hospital’s laryngology unit, establishing correlation with clinical outcomes through questionnaire and medical record.
These patients were submitted to surgery for exertion of papilloma between 2008 and 2015. The material was sent for a histopathologic evaluation at the laboratory of anatomic pathology from the same hospital.
The collected material was stored in paraffin blocks. After histological confirmation the blocks were microdissected. The obtained material was submitted to centrifugation and then an enzymatic digestion method was applied using proteinase K in order to extract viral DNA of the samples.
DNA amplification was carried out through polymerase chain reaction (PCR) in order to obtain just viral subtypes HPV 6, 11, 16 or 18 from the samples.
The questionnaire used for retrospective analysis of medical records of the studied patients presented the following variables:
• Number of surgical interventions
• Age of diagnosis (years)
• Disease duration (years)
• Surgeries per year of disease
• Presence of dysplasia
• Need for tracheostomy
• Death
According to the objectives established in this research the following hypothesis were determined:
1. Is there a statistically significant difference between mean values of the variables number of surgeries; age of diagnosis (years); disease duration (years) and surgeries per year of disease and HPV types (6, 11, 16 and 18)?
2. Is there a statistically significant relation between the variables dysplasia; tracheostomy; death and HPV types (6, 11, 16 and 18)?
Hypothesis 1 was verified using the Kruskal-wallis test, because since all evaluated variables presented a continuous scale for at least one subtype of HPV data were not normally distributed. Shapiro-Wilk test was applied for normality verification with significance level of 0.05. When statistically significant difference between HPV types was identified by Kruskal-Wallis test, pairwise comparison was performed using Dunn’s multiple comparison tests. Significance level was 0.05.
This study has received the approval of the Ethics Committee of the Hospital, in August 2015. Privacy, confidentiality and anonymity of the patients were assured.
RESULTS
In the present study were analyzed 34 samples collected from patients submitted papilloma resection. Three of those did not amplify DNA on PCR exam for subtypes 6, 11, 16 and 18 and in only 1 patient it was not possible to extract DNA from the sample.
Descriptive results of the variables for each type of HPV are detailed in Table 2. HPV 18 group had the higher mean of surgeries per year of disease (14.5), followed by HPV 6 (10.36) and HPV 11 with a mean of 9.07 surgeries. Group HPV 6 had higher variance and standard deviation.
For the variable age of diagnosis, group HPV 11 presented higher mean value 22.93 years. In group HPV 18 the mean was 14.5 years, while in HPV 6 the mean was 17.27 years also with higher standard deviation.
However while considering p<0.07 it is possible to observe a relation between these two variables, as evidenced by the test of difference between two proportions.
DISCUSSION
Recurrent Respiratory Papillomatosis is still a frustrating disease due to the high-risk of recurrence and inability to ensure complete cure. Therefore several studies are being carried out searching for new techniques and therapies that may improve survival rates or even offer better prognosis.
Its viral etiology was first described at 1923 by Ullmann [4] and after the development of hybridization techniques and PCR it was possible to identify HPV and its types.
According to the objectives and hypothesis determined by this study it was possible to achieve some results. Samples collected from 30 patients, 60% male and 40% female, have amplified HPV on laryngeal biopsy. The sample of the present study presented results very similar to those reported on the literature regarding the prevalence of HPV types 6 and 11 in RRP patients (approximately 90%) [2,5]. The most prevalent type was HPV 11 (50%) followed by HPV 6 (36.6%). The three samples that did not amplify types 6, 11, 16 and 18 on PCR may be related to more rare HPV types. Levi et al. [6] have observed in their study 19 samples of laryngeal biopsy, 74% of HPV 6 and 16% of HPV 11 and no sample of genotypes 16 or 18. Sanchez et al. [7] in their study observed a frequency of 69% of HPV 6, 27.1% of HPV 11 and 7.8% of HPV 16. Co-infection was observed in 9.3% of the samples.
Between types 6 and 11, both classified as low-risk of malignancy, HPV 11 is more likely to cause a more aggressive disease with higher potential of recurrence and higher number of surgeries [8,9]. In the present study there was no statistically significant difference between groups HPV 6 and HPV 11 regarding the mean values for number of surgeries, surgeries per year of disease, tracheostomy, death and dysplasia, variables that could be related to this aggressive potential.
Quantitative analysis indicated a tendency of higher values for clinical outcomes, number of surgeries, and surgeries per year of disease in the HPV 18 group. Nevertheless statistical tests presented p>0.05 and there was no significant difference among the three groups. The HPV 6 group was the less homogeneous and presented higher standard deviation for all variables.
Among qualitative variables tracheostomy and dysplasia were higher in the HPV18 group; yet no statistically significant difference was observed in the comparison with other groups.
Regarding mortality while testing the difference between both proportions a statistically significant prevalence of this outcome was observed in group HPV 18, in comparison with groups HPV 6 and 11 (p<0.0 7). Yet no statistically significant difference was observed between subtypes 6 and 11, with 9.1% and 6.7%, respectively. The rate of mortality in the group with HPV 18 on the other hand was of 50%. The cause of death of these patients was not necessarily related to RRP, however the variable death was considered just as an outcome itself.
A clear relation between HPV 16 and 18 and cervical cancer was already established on the literature. In RRP the relation between HPV and laryngeal cancer is not yet fully established. According to the literature, the presence of malignancy is rare, ranging from 0 up to 7% of RRP cases [10]. The present study have reported the presence of dysplasia in 10% of the analyzed samples, two of them from the group HPV 11 and one from HPV 18.
Besides contributing for the studies about this disease, genotyping of HPV is also very important for a better treatment plan, as for the assessment of the infection prognosis. The methods that are used on the detection of HPV types can be divided into three categories. Low sensitivity tests, such as Immunohistochemistry and in situ hybridization, only detect the virus when it is present in more than 10 copies of the viral DNA per cell. Moderate sensitivity tests, which include Southern blot and dot blot hybridization as well as reverse dot-blot hybridization, can detect the virus when it is present in more than 1 copy of the viral DNA per cell. A high sensitivity test that was applied in the present study is the Polymerase Chain Reaction (PCR) is able to detect the virus even when it is present in less than 1 copy [11].
According to the age of diagnosis RRP can be classified as juvenile, with onset before 6 years old and adult, and adult with onset between 20 and 40 years old. In the present study the mean age was 19.73 years indicating prevalence of adult RRP in our patients. Only 13 patients (43%) were under 10 years old when. The adult form of RRP is usually associated to a lower number of lesions and recurrence rates as well as lower risk of malignancy [12].
The transmission of HPV in RRP is not yet fully understood. There are strong evidences of vertical transmission however it is still controversial if the transmission occurs exclusively through birth canal or transplacentally as well. Studies show the presence of HPV in the amniotic fluid of mother with condylomatosis. Other studies also report the presence of HPV in the airway of newborns of mothers with no history of genital warts suggesting subclinical and latent infections. It is assumed that transmission may also occur through autoinoculation and oral sex.
There are a great number of researches on RRP focused on the prophylaxis and the use of active immunization. The developed vaccines have an important role assisting the host on fighting the infections well as to avoid vertical contamination. Bivalent vaccine is broadly commercialized and the tetravalent is already available in the Brazilians Public Health system. It is also assumed that the vaccine may also improve the immunity of a host that is already contaminated reducing the risk or relapse.
With the implementation of prophylactic measures such as health assistance, active immunization, control of sexually transmitted diseases and proper care to avoid vertical transmission there will be a lower incidence of the disease and thus the possibility of eradicating RRP.
CONCLUSION
Recurrent Respiratory Papillomatosis is a rare and potentially fatal disease. Along the search for new diagnosis methods and treatments for our patients, this study has shown the importance of HPV genotyping for the prognosis.
Molecular identification of the types of HPV in our patients was in accordance to the literature, with a predominance of HPV 6 and 11 and few cases of HPV 18. In clinical outcomes correlation there was no statistical significant differences between subtype 6, 11 and 18 groups regarding the number of surgeries, dysplasia, tracheostomy, disease duration, age of diagnosis and surgeries per year of disease. However the variable “death” was higher with statistically significant difference in HPV 18 group.
These results stimulate the search for new ways to determine a prognosis and treat these patients. Further studies with larger samples are required in order to study the statistical correlation between HPV subtypes and clinical outcomes.
1. Kayode AS (2012) The descriptive review, from recurrent respiratory papillomatosis of the disease, an enigmatic. Arquivos Int Otorrinolaringol 16: 108-114.
2. Avelino MAG, Zaiden TCDT, Gomes RO (2013) Tratamento cirúrgico e terapias adjuvantes na papilomatose respiratória. Braz J Otorhinolaryngol 79: 636-642.
3. Avelino Melissa AG, Gutzman RL, Fujita RR, Pignatari S, Weckx Luc LM, et al. (2004) Estudo do efeito do Cidofovir na papilomatose laríngea recorrente em crianças: Relato preliminar. Rev Bras Otorrinolaringol 70: 734-738.
4. Ullmann EV (1923) On the etiology of laryngeal papilloma. Acta Otolaryngol 5: 317-374.
5. Naren NV, Pine HS, Underbrink MP (2012) Recurrent respiratory papillomatosis. Otolaryngol Clin North Am 45: 671.
6. Levi JE, Delcelo R, Alberti VN, Torloni H, Villa LL (1989) Human papillomavirus DNA in respiratory papillomatosis detected by in situ hybridization and the polymerase chain reaction. Am J Pathol 135: 1179-1184.
7. Sanchez GI, Jaramillo R, Cuello G, Quintero K, Baena A, et al. (2012) Human papillomavirus genotype detection in recurrent respiratory papillomatosis (RRP) in Colombia. Head Neck 35: 229-234.
8. Wiatrak BJ, Wiatrak DW, Broker TR, Lewis L (2004) Recurrent respiratory papillomatosis: A longitudinal study comparing severity associated with human papilloma viral types 6 and 11 and other risk factors in a large pediatric population. Laryngoscope 114: 1-23.
9. Tjon Pian Gi RE, San Giorgi MR, Slagter-Menkema L, van Hemel, van der Laan, et al. (2015) Clinical course of recurrent respiratory papillomatosis: Comparison between aggressiveness of human papillomavirus-6 and human papillomavirus-11. Head Neck 37: 1625-1632.
10. Aaltonen LM, Rihkanen H, Vaheri A (2002) Human papillomavirus in larynx. Laryngoscope 112: 700-707.
11. Therezita PP, Galvão C, Bussoloti Filho I (2006) Prevalência do papilomavírus humano (HPV) na cavidade oral e na orofaringe. Rev Bras Otorrinolaringol 72: 272-282.
12. Filho JAX, Simoceli L, Imamura R, Tsuji DH, Sennes LU (2003) Papilomatose laríngea recorrente: Experiência de 10 anos. Rev Bras Otorrinolaringol 69: 599-604.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Pathology and Toxicology Research
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- BioMed Research Journal (ISSN:2578-8892)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)