666
Views & Citations10
Likes & Shares
Due to
relatively nonspecific clinical findings associated with a variety of
granulomatous diseases, a microscopic diagnosis in it leads to diagnostic
dilemma for the clinician. The true nature of this disease is controversial and
remains unknown but it may be a reactive lesion, a developmental anomaly or a
benign neoplasm. Often an extensive clinical, microscopic and laboratory
evaluation may be required to identify the source of the granulomatous
inflammation. In this case report we discuss bilateral idiopathic mandibular lesion
in an 8 year old girl.
Keywords: Granulomatous inflammation, Benign, Mandible
INTRODUCTION
A typical differential diagnosis related to
mandibular swelling includes:
·
Ameloblastoma which is seen in older
age, in posterior part of mandible and is multilocular.
·
Odontogenic myxoma which is usually
associated with missing or impacted tooth, multilocular with honey comb
appearance.
·
Dentigerous cyst.
·
Cherubism with epicenter located in the
posterior aspect of the mandible and maxilla, multiple and bilateral.
·
Aneurysmal bone cyst which causes
profound expansion and aspiration produces blood.
·
Central giant cell granuloma.
Granulomas related to giant cells are usually
an intraosseous lesion consisting of cellular fibrous tissue that may contains
multiple foci of hemorrhage, aggregations of multinucleated giant cells and
occasionally trabeculae of woven bone [3]. It was described by Jaffe in 1953
that separated giant cell lesions of jaw from other jaw lesions. He considered
it to be a locally reparative reaction of bone, which can be either due to
inflammatory response, local trauma or hemorrhage [4].
Clinically, it can vary from benign to rather
aggressive lesion and demonstrates varying histopathological features [5].
Non-aggressive and aggressive variants are compared according to clinical and
radiographic behavior. Non-aggressive lesions are slow growing, almost
asymptomatic growth that does not perforate the cortical bone or induce root
resorption and has low tendency to recur whereas aggressive lesions which are
usually seen in younger patients are painful, rapidly growing with expansion or
perforation of cortical bone, radicular resorption and high tendency to recur.
He interprets that large functional surface area is occupied by giant cells and
larger relative giant cells in aggressive lesion [6]. It occurs most commonly in
children and young adults and has a female predilection. Lesions are located
more commonly in the mandible mostly involving molar and premolar area and
frequently cross the midline. Its presence in the mandibular body area, the
entire ramus, condyle and coronoid leads to a therapeutic challenge
The treatment modalities include surgical
excision either by curettage or en bloc resection and alternative non-surgical
approaches such as intralesional corticosteroid injections, calcitonin
injections and subcutaneous alpha interferon injections. Here, we report a case
of aggressive unknown granulomas in mandible (which is very closely related to
central giant cell granuloma) with emphasis on clinical, radiological and
management of the lesion.
CASE REPORT I
An 8 year old girl came with complain of pain
and swelling in lower left region of face since few months (Figure 1).
It relieves on taking medication but reoccur as soon as medication stops.
Patient has no relevant past medical or dental history. On oral examination
nothing suspicious was found. Patient had good oral hygiene. Patient was
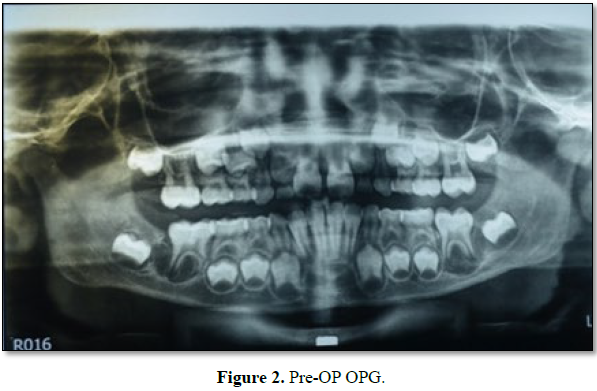
advised for OPG. OPG revealed presence of radiolucency wrt to 36 and 46.
Patient complained swelling only but OPG revealed similar lesion on the other
side also which was not known to patient or parents as it was asymptomatic (Figure
2).
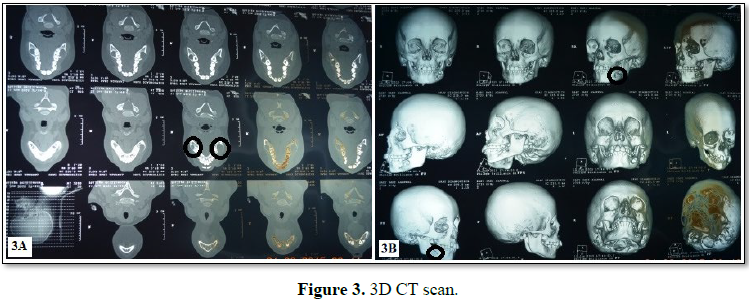
Thereafter 3D-CT scan was done for precise evaluation and assessment of
the lesion which showed bone destruction/perforation of cortical plate in that
region, representing its aggressive nature (Figure 3).
Patient had no carious exposure, periodontal disease or any history of
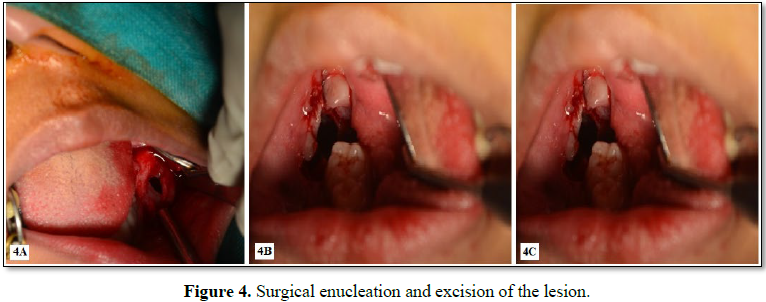
trauma. Looking at the aggressive nature of the lesion and bilateral
involvement, it was planned to surgical excise the region and removes the tooth
related to it, i.e., molar, after which only histopathological examination will
ascertain its nature (Figures 4A-4C).
Following the careful enucleation, the tooth with the lesion (which was
attached at and around the cemento-enamel junction) was sent for the
histopathological examination (Figure 5).
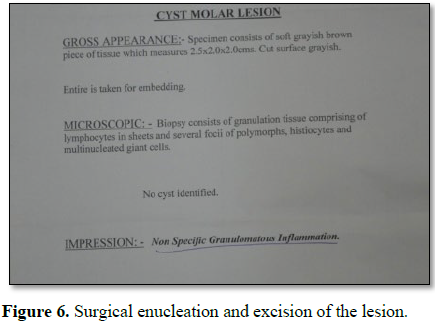
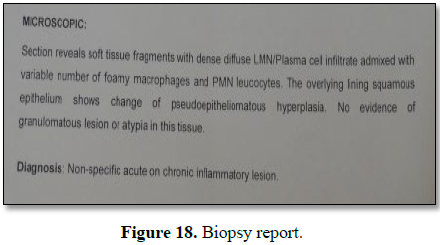
The report revealed presence of lymphocytes, histiocytes and
multinucleated giant cells. No cyst was identified. But diagnosis was not
confirmed. The result was non-specific granulomatous inflammation (Figure 6).
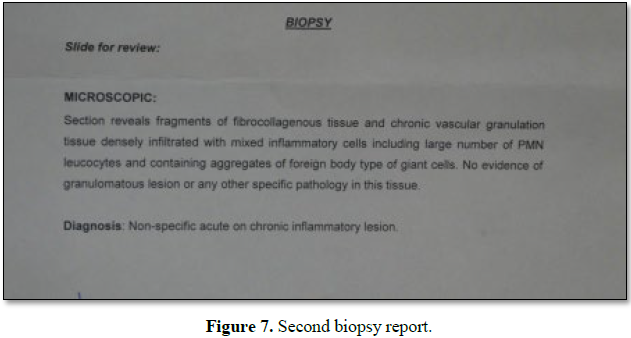
To cross check and confirm the report, specimen was sent to other labs
also, but all failed to give a definitive diagnosis and similar presentation of
giant cells, lymphocytes was reported (Figure 7).
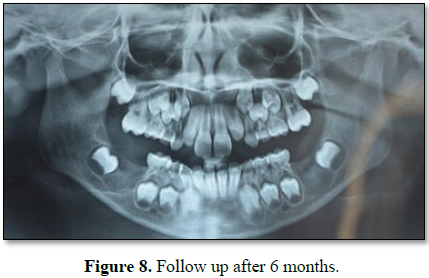
Patient was recalled after 6 months and no swelling or radiolucency was
present. But actual cause was still unknown (Figure 8).
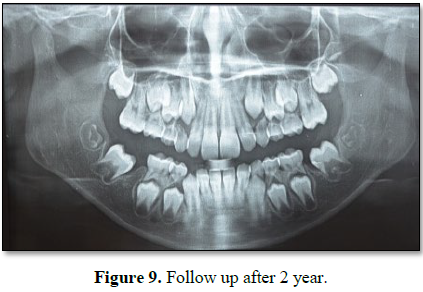
After 2 years of follow up, the 37 and 47 have physiologically mesially
migrated at the site of extracted first
molars uneventfully (Figure 9).
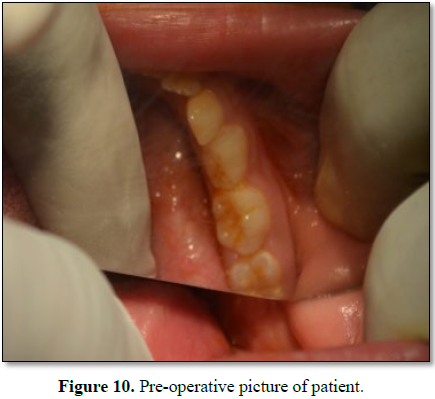
CASE REPORT II
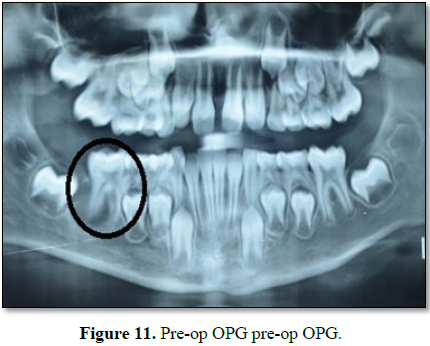
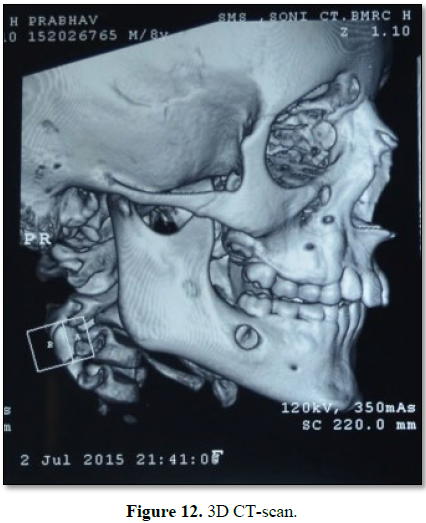
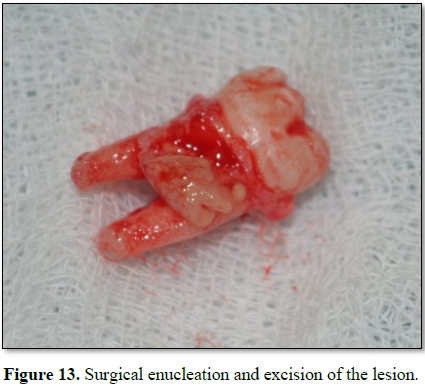
Similar case
with exactly similar clinical presentation, radiographic finding,
histopathological reporting and immediate recovery after similar intervention
procedure irt to 46. The only difference was that this lesion was unilateral (Figures 10-14).
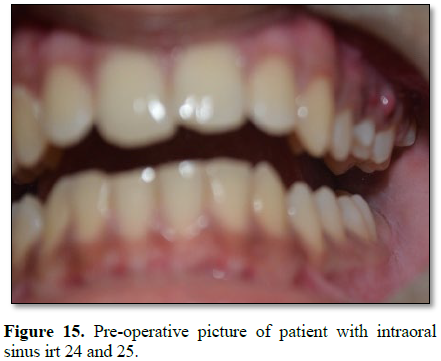
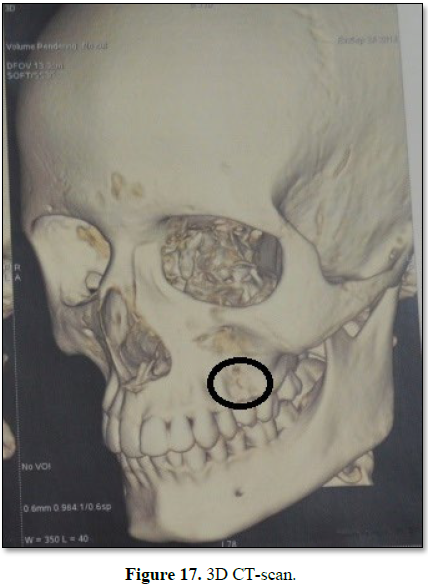
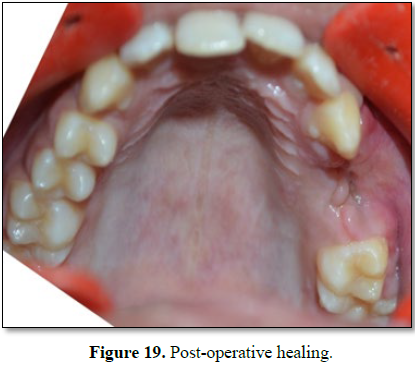
CASE REPORT III
Another case with exactly similar clinical presentation, radiographic
finding, histopathological reporting and immediate recovery after similar
intervention procedure irt to 24,25, but this time the lesion was unilateral
and in maxilla (Figures 15-19).
DISCUSSION
In 1953, Jaffe [4] described an apparently reactive intraosseous lesion
of the mandible and maxilla following trauma induced intraosseous hemorrhage
and containing prominent giant cells. He separated giant cell lesions from long
bone giant cell tumor based on differences in their histological pattern and
clinical behavior [8]. Due to its reactive in nature, he gave the term
reparative giant cell granuloma [9].
It is the disease of the young presenting as a painless expansible mass
ranging from a slowly growing asymptomatic swelling to an aggressive lesion
causing pain and bone destruction, being more common in the anterior portion of
the mandibular body sometimes crossing the midline, the epicentre being
anterior to the first molar region. It is an uncommon benign lesion of the jaw
which accounts for <7%. Usually in this cortical plates are thinned, with
sometimes perforation but gross soft tissue involvement remains limited [10].
In the present case, biopsy report revealed presence of lymphocytes,
histiocytes and multinucleated giant cells. No cyst was identified. The result
was non-specific granulomatous inflammation. The sign and symptoms were similar
to central giant cell granuloma.
But upon enucleation, we can clearly appreciate that the lesion was
attached at the cementoenamel junction, just like in dentigerous cyst, making
it having mixed presentations.
CT scan showed excessive bony thinning and destruction with resorption of
buccal cortical plates, showing signs of its aggressive nature.
In present case, the radiologic features of granuloma was not been
clearly defined; the lesion appeared as unilocular radiolucency with
ill-defined margins with varying degrees of expansion of the cortical plates.
Radiographic appearance of the lesion is not pathogenomic and may be confused
with that of many other lesions of the jaws [6]. Various methods have been
described for the treatment of such lesion of jaws. Most often treatment used
is Curettage alone or in combination with resection with or without continuity
loss [11]. Surgical treatment is usually varied depending upon the anatomic
location, size of lesion, clinical behavior, periosteal or nerve involvement.
But in this case, perforation of cortical plates prompted us for surgical
resection and removal of molars related to the lesion.
CONCLUSION
Granulomatous inflammation may manifest in the oral cavity and usually
with an array of non-specific clinical findings. Thus, an extensive clinical,
microscopic and laboratory evaluation may be required in order to identify the
source of the granulomatous inflammation. However, if the lesions are timely
identified and appropriate therapy rendered, prognosis of the condition is
significantly improved. This case highlights the difficulty in diagnosing and
management of the lesion. Hence, this lesion continues to develop the interest
and mystify the clinicians.
DECLARATION OF
PATIENT CONSENT
The authors certify
that they have obtained all appropriate patient consent forms. In the form the
patient(s) has/have given his/her/their consent for his/her/their images and
other clinical information to be reported in the journal. The patients
understand that their names and initials will not be published and due efforts
will be made to conceal their identity, but anonymity cannot be guaranteed.
1. Ramakrishnan L (2012) Revisiting
the role of the granuloma in tuberculosis. Nat Rev Immunol 12: 352-366.
2. Alawi F (2005) Granulomatous
diseases of the oral tissues: Differential diagnosis and update. Dent Clin 49:
203-221.
3. Kramer IR, Pindborg JJ, Shear M
(1992) Histological typing of odontogenic tumours. Berlin: Springer Science
& Business Media.
4. Jaffe HL (1953) Giant-cell
reparative granuloma, traumatic bone cyst and fibrous (fibro-osseous) dysplasia
of the jawbones. Oral Surg Oral Med Oral Pathol 6: 159-175.
5. Kruse-Lösler B, Diallo R, Gaertner
C, Mischke KL, Joos U, et al. (2006) Central giant cell granuloma of the jaws:
A clinical, radiologic and histopathologic study of 26 cases. Oral Surg Oral
Med Oral Pathol Oral Radiol Endodontol 101: 346-354.
6. Chuong R, Kaban LB, Kozakewich H,
Perez-Atayde A (1986) Central giant cell lesions of the jaws: A
clinicopathologic study. J Oral Maxillofacial Surg 44: 708-713.
7. Austin LT, Dahlin CD, Royer QR
(1955) Central giant granuloma and granuloma and related condition affecting
the jaw bone. Oral Surg Oral Med Oral Pathol 12: 1259.
8. Shah U, Shah A, Kumar S (2006)
Giant cell reparative granuloma of the jaw: A case report. Indian J Radiol
Imaging 16.
9. O’Connell JE, Kearns GJ (2013)
Aggressive giant cell granuloma of the jaws treated with interferon alpha: A
report of two cases. Irish J Med Sci 182: 163-170.
10. Chatha MR, Ali K, Aslam A, Afzal
B, Shahzad MA (2006) Current concepts in central giant cell granuloma. Pak Oral
Dent J 26: 71-78.
11. Shafer WG, Hine MB, Levy BM (1983)
A Text Book of Oral pathology. 4th Edn. Philadelphia: Saunders, pp:
146-149.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Pathology and Toxicology Research
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Journal of Allergy Research (ISSN:2642-326X)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)