942
Views & Citations10
Likes & Shares
White
lesions both physiologic as well as pathologic are relatively frequent in the
oral cavity, the most common pathologic entity being oral leukoplakia (OL).
There are many variants of OL, one of which is oral proliferative verrucous
leukoplakia (OPVL). OPVL is a rare clinico-pathological entity, which is slow
growing, long-term progressive lesion, but remains an enigmatic and difficult
to define. The etiology of OPVL remains still unclear. This article describes
the clinical aspects and histologic features of an OPVL case that demonstrated
the typical behavior pattern in a long-standing, persistent lesion.
Keywords: Leukoplakia, Oral proliferative leukoplakia,
Malignant transformation
INTRODUCTION
In India
OPVL prevalence is 1.5 to 4.3% [2,3]. It is seen in localized area in
distribution, hyperkeratotic in nature and white in appearance due to wetting
of keratotic patch [4].
We present a
rare case of Verrucous Leukoplakia presenting as Verrucous Carcinoma, which can
put a clinical dilemma due its clinical picture (Figure 1).
CASE REPORT
A 56 years old male
patient (Figure 1), reported to
Department of Oral Medicine and Radiology with a chief compliant of missing
teeth in left upper back tooth region since 1 year Anamnesis was
non-contributory. Patient reported a habit history of bidi smoking, about 5-6
times daily since 15-20 years and claims to be an occasional drinker since
about 20 years. General Examination revealed patient was well built, well
nourished, conscious, alert, oriented to time, place and person. No signs of
pallor, icterus, cyanosis, clubbing, lymphadenopathy and edema are seen. Extraorally
patient shows right and left
submandibular lymphadenopathy, bilateral whitish lesions on the
commissures of the lips that extend intraorally and have a triangular
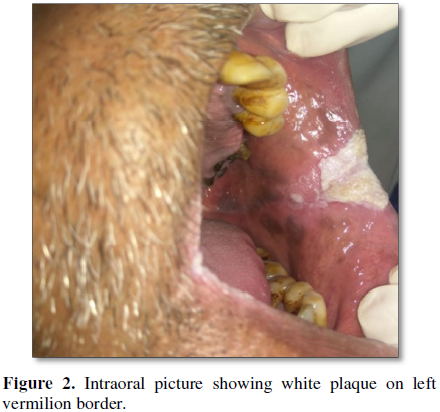
appearance. On intraoral inspection grayish white slightly raised lesion having
a verrucous or papillary texture measuring 4 × 5 cm in size seen on the left
buccal mucosa.
On right side a whitish plaque measuring 2 × 3
cm seen extending from upper buccal vestibule to the lower buccal vestibule is
seen. Both lesions are extensions of white, triangular, raised, plaques present
on the commissures of the lips extraorally. The lesions have an irregular
surface with papillary like extensions. On palpation the lesion is non-tender,
non-fluctuant, non-compressible, there is presence of network of white plaque
which resembles verrucae (Figures 2 and
3). Based on history and clinical examination a provisional diagnosis of
proliferative verrucous leukoplakia was made which was later confirmed
histopathologica.
Tobacco Cessation Counseling was done and the patient was instructed to
quit the habit. Patient was prescribed Cur Q Plus tablets (Curcumin 300 mg +
Piperine 1.8 mg), three times daily for three months and the patient is placed
on a fortnightly recall.
DISCUSSION
White lesions are a commonly seen in the oral cavity. Among those
leukoplakia is most common. It becomes more exophytic with the development of
the multiple keratotic plaques with roughened surface projection. It has got
predilection for female than males and is present with the patients who don’t
smoke. As the disease progresses it can change clinically and microscopically
identical to the verrucous carcinoma or squamous cell carcinoma.
Etiopathogenesis
Risk factors: The risk factors that contribute to the development of OPVL
are:
Local factors:
·
Tobacco: Tobacco is widely used in
two forms:
Smokeless tobacco (chewable tobacco and oral use of snuff)
Smoking tobacco (cigar, cigarette, bidi and pipe)
a)
Smokeless tobacco: Chewing of tobacco leads to leaching of several
materials like tobacco tars and resins. These extracts of tobacco contain
chemicals like nitrosonornicotine, nicotine, pyridine and picoline. These
chemical constituents and an alkaline pH act as irritants and lead to
alterations of mucosa in the form of sub lethal injury within the deeper layers
of oral epithelium. This induces concomitant epithelial hyperplasia.
a)
Smoking tobacco: The smoke along with its constituents like polycyclic
hydrocarbons, beta-napthylamine, nitrosamines, etc., and the heat generated in
the oral cavity cause irritation in the oral mucosa, frequently seen as
reddening and stripping of the mucosa. With continued smoking minute red and
white striations are formed and the surface appears swollen.
·
Alcohol: Prevalence of OPVL is higher
in drinkers than in non-drinkers. This is mainly due to the action of alcohol
to facilitate the entry of carcinogen into exposed cells and thus altering the
oral epithelium and its metabolism.
·
Chronic
irritation:
Continuous trauma is a factor that leads to development of OPVL. The source of
irritation or trauma may be due malocclusion, ill-fitting dentures, sharp
broken teeth, hot and spicy food, etc. The chronic irritation must be intense
enough to induce surface epithelium to produce and retain keratin.
·
Candidiasis: Candida albicans is commonly seen in association with leukoplakia.
Tobacco smoking may lead to candidal colonization because of increased
keratinization, reduced salivary immunoglobulin-A concentration or depressed
PMN leucocyte function.
Regional and systemic
factors:
·
Nutritional deficiency: Sideropenic anemia and
other nutritional deficiencies predispose to the condition.
·
Xerostomia: These factors are salivary
gland disease, radiation, etc.
·
Drugs: Anticholinergic,
anti-metabolic drug, etc.
·
Syphilis [5].
Clinical
classification:
·
Homogenous: It is a completely whitish
lesion
-
Flat: It is smooth surface.
-
Corrugated: Like a beach at ebbing tide.
-
Pumice like: With a pattern of fine lines.
-
Wrinkled: Like dry, cracked mud surface.
·
Non-homogenous:
-
Nodular or speckled: Characterized by white spikes or nodules on
erythematous base.
-
Verrucous: Slow growing, papillary proliferations above mucosal surface
that may be heavily keratinized.
-
Ulcerated: Lesion exhibits red area at the periphery of white patches.
-
Erythroleukoplakia: Leukoplakia present in association with erythroplakia.
Clinical features:
·
Sex and age
distribution: Males
are more affected. The mean age of diagnosis is 70 years [6].
·
Common sites: Leukoplakia mostly occurs
bilaterally mainly affecting the buccal mucosa, gingiva and vermilion border of
lip. Lips, palate, maxillary mucosa, retromolar area, floor of mouth and
tongue.
·
Color: The lesion appears white or
yellowish white due to hyper keratinized areas. As the lesion progresses, it
become thicker and whiter, sometimes developing a leathery appearance with
surface fissure.
·
Appearance: Surface of the lesion shows
a pappilomatous surface that feels rough on palpation.
Proliferative
verrucous leukoplakia:
-
It is an aggressive type of leukoplakia with very high rate of malignant
transformation, but oral carcinoma can develop from any leukoplakia.
-
It is seen more in elderly women. Women to men ratio is 4:1.
-
Proliferative verrucous leukoplakia appears as a single or multifocal
growth involving several oral sites. Most commonly buccal mucosa affected in
women and tongue in men.
-
Development of proliferative verrucous leukoplakia starts as a simple
hyperkeratosis without epithelial dysplasia, verrucous carcinoma and then
carcinoma.
-
Proliferative verrucous leukoplakia has association with human papilloma
virus infection. HPV-16 infection may play an important role in these lesions.
-
Among different forms of leukoplakia, proliferative verrucous leukoplakia
has high malignant transformation. In a study of 54 cases of proliferative
verrucous leukoplakia, Silverman and Gorsky found out that 70.3% subsequently
developed squamous cell carcinoma [7].
Differential
diagnosis of oral proliferative verrucous leukoplakia [8]
·
Lichen Planus: Differentiated by Wickham’s Striae and multiple lesions.
·
Syphilitic mucus patches: Features like split papillae and condyloma
latum may be present.
·
White sponge nevus: Present soon after birth and is widely distributed
all over the mucus membrane.
·
Discoid lupus erythematosus: Central atrophic area with small white dot
and radiating white straie.
·
Candidiasis: Differentiated as the candidal lesions are scrapable.
· Verrucous carcinoma: Lesions are elevated (exophytic).
Histopathology
PVL shows a variable microscopic appearance, depending on the stage of
the lesions. Early PVL appears as a benign hyperkeratosis that is
indistinguishable from other simple leukoplakic lesions. With time, the
condition progresses to a papillary, exophytic proliferation that is similar to
localized lesions of verrucous leukoplakia. In later stages this papillary
proliferation exhibits down growth of well-differentiated squamous epithelium
with broad, blunt rete ridges. This epithelium demonstrates invasion into the
underlying lamina propria, in this stage it is indistinguishable from verrucous
carcinoma. In the final stage the invading epithelium becomes less
differentiated, transforming into the condition called squamous cell carcinoma.
Because of the variable clinical and histopathologic appearance of PVL, careful
correlation of the clinical and microscopic findings is required for diagnosis
[9,10].
Treatment
·
Prohibition of smoking: Patient should be asked to cease smoking with
immediate effect.
·
Removal of chronic irritant: Sharp points from the dentures should be
removed along with enameloplasty of sharp teeth.
·
Elimination of other etiological factors: Factors like syphilis, alcohol,
dissimilar metal restoration, etc., should be eliminated.
·
Carbon dioxide laser, radiation, topical bleomycin solution, oral
retinoids, beta-carotene and systemic chemotherapy have all failed to achieve
permanent cure.
·
Laser ablation reportedly has been successful in a very small group of
patients followed for 6-178 months.
·
Topical photodynamic therapy also may prove useful; it causes relatively
low morbidity and no scarring and multiple mucosal sites can be treated
simultaneously.
·
The use of antioxidant nutrients and vitamins has not been reproducibly
effective in management. Programs have included single and combination dosages
of vitamins A, C and E; beta carotene; analogues of vitamin A; and diets that
are high in antioxidants and cell growth suppressor proteins [11,12].
CONCLUSION
Oral Proliferative verrucous leukoplakia is a rare and aggressive form of
disease which requires special attention. The aim/intention of this case report
is to report the clinical case so as to sensitize the oral physicians.
1. Ongole R, Praveen BN (2013) Text
book of Oral Medicine, Oral Diagnosis and Oral Radiology. Red and white
lesions, Chennai, India. Elsevier 2nd Edn. pp: 133-173.
2. Petti S (2003) Pooled estimate of
world leukoplakia prevalence: A systematic review. Oral Oncol 39: 770.
3. Mello FW, Miguel AFP, Dutra KL,
Porporatti AL, Warnakulasuriya S, et al. (2018) Prevalence of oral potentially
malignant disorders: A systematic review and meta-analysis. J Oral Pathol Med
47: 633.
4. Rajendran R (2009)
Sivapathysundaram benign and malignant tumors of oral cavity. Shafers Textbook
of Oral Pathology: Elsiever pp: 80-218.
5. Ghom V (2010) Textbook of Oral
Medicine. 2nd Edn. pp: 194-203.
6. Greenberg MS, Glick M (2005)
Burket oral medicine. Red and White Lesions of Oral Cavity. Delhi, India:
Bcdeker, India. Elsevier: 10th Edn.
7. Bagan JV, Soriano YJ, Feeinandiaz
Diaz JM, Roda-poveda R, Bagan L (2011) Malignant transformation of
proliferative verrucous leukoplakia to oral squamous cell carcinoma: A series
of 55 cases. Oral Oncol 47: 732-735.
8. Neville BW (2009) Oral and
maxillofacial pathology. 3rd Edn. p: 394.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)