675
Views & Citations10
Likes & Shares
There are several studies in rodents, primates and also in humans showing
that prenatal stress has impact on the fetus and the new born in terms of
his/her physiological state and growth while the consequences and risks are
meanwhile well approved; there is very rare literature about the character of
the relevant stress-factors. The objective of this clinical trial was to find
preventive or predisposing factors in stress coping. It investigated
subjective, objective and hormonal aspects of stress, trying to find the
criteria with the highest impact on pregnant women. Three structured prenatal
packages of self-report questionnaires in addition to anamnestic data were
collected. The surveyed data included anxiety, perceived stress, life events,
subjective stress (PSQ), pregnancy-specific stress (PESI), depression (EPDS),
partnership (FPD) and social support (F-sozU). 111 women were included into the
analysis. The findings show that a good partnership and social support seem to
be the most important factors preventing pregnant women from emotional and
psychological stress, independent from their objective situation. These results
highlight the importance of a firm social environment and a good partnership as
highly underestimated factors to minimize stress-related risks for mother and
child.
Keywords: Pregnancy, Stress,
Partnership, Social support, Prenatal
INTRODUCTION
METHODS
Participants
This study is a three-wave prospective
longitudinal study conducted during the period November 2007 to January 2009.
Participants were recruited to the study via public and private search,
referrals from obstetricians, notices posted in clinics and advertisement in
the internet and newspapers. Inclusion criteria were an early pregnancy (week
of gestation: 13.6 ± 1.68) and no severe mental or physical problems. Exclusion
criteria were (a) inability to speak and read German language, (b) twin
pregnancy and (c) advanced pregnancy (>19 week of pregnancy). Every woman
gave her written, informed consent in accordance with the ethic committee of
the University Clinic of Heidelberg, which approved all protocols.
Procedures
Eligible subjects received a regarding
demographic information; social, medical and psychiatric history, information
concerning partnership and pregnancy, medical complications and live events, as
well as a package of structured questionnaires including the PSQ, PESI, PRAQ-R,
F-sozU, EPDS and FPD. This package had to be completed at three points of time,
each in every trimester of pregnancy. In addition, the women were consulted for
appointment days, also one in each trimester, where samples of salivary
cortisol were taken. The determining instruments for this article will be
presented in the following:
The Perceived Stress Questionnaire (PSQ) by
Levenstein et al. [20], translated by Fliege et al. [21], is a tool for
psychomatic research, with the aim to measure the subjective perceived stress.
This questionnaire contains four scales (worries, strains, joy and demands);
differently from the original version by Levenstein et al. [20] that includes
five scales. The original number of 30 items was reduced to 20 items. The first
three scales try to image the individual’s internal stress reaction, whereas
the scale, demands focuses on the apperception of external stressors. Internal
consistency of the subscales is ranging from 0.80 to 0.86; reliability is at
least 0.80.
The Prenatal Emotional Stress Index (PESI) by
Moehler et al. [3] is an instrument developed to measure emotional stress in
pregnancy. In this study it was used as prospective measurement. The
questionnaire consists of 33 items, 11 for each trimester of pregnancy. Each
item images anxiety, sadness, joy, perceived stress and emotional strain of the
mother on a visual analog scale from 0 to100. The arithmetic mean of all 33
single scales discloses the total burden of stress during pregnancy.
The revised Pregnancy Related Anxiety
Questionnaire (PANX/PRAQ-R) aims to record pregnancy-specific anxiety [22]. It
contains 10 items accordant to the three-factor-model: 1. ‘fear of giving
birth’, 2. ‘fear of having a handicapped child’ and 3. ‘Fear of one-self’s
unattractive appearance’. The PRAQ was developed by van den Bergh [1], revised
by Huizink [22] and translated in German language by Moehler et al. [3]. The
answer format consists of a five point Likert scale reaching from “never” to
“mostly”. Cronbach’s alpha for all three subscale is >0.76.
F-SozU (“Fragebogen zur sozialen Unterstützng”)
is a questionnaire dealing with social support by Sommer and Fydrich [23]. Four
scales are measured: emotional support, practical support, social integration
and social strains. Four all of these scales and the total the internal
consistency are identified between 0.81 and 0.93.
The German “Fragebogen für
Parnterschaftsdiagnostik” (FPD) (‘Questionnaire for diagnostics of
partnership’) assessed marital satisfaction, using three subscales: 1. Behavior
during partnership conflicts, 2. Tenderness and 3. Commonness/communication.
Each woman indicated on a four point Likert scale how often (“never”, “seldom”,
“often”, “very often”) some attitudes from the partner or themselves occur
(e.g. the statement: “He blames me of failures I did in the past”).
Reliabilities for all subscales are located between 0.88 and 0.95. Internal
Consistency for the whole scale constitutes r=0.83.
One part of the questionnaire, which the women
completed once in the beginning and particular parts continuously once every
trimester was a part about live events. It was asked for critical events like
separation in partnership, medical complications during pregnancy, financial
problems, death of a relative, loss of home or job, etc. All possible life
events were summarized to one ‘critical life event score’ ranging from zero to
eleven.
STATISTICAL ANALYSIS
SPSS version 17.0 for Windows was used for the
statistical analysis. Single missing values were replaced by the mean value of
the item. Descriptive analysis of the anamnestic data reported was carried out.
Correlation between the different questionnaires and cortisol were conducted
using Pearson or Spearman’s rho correlation if data were non-normally
distributed. A p-value of ≤ 0.05 was regarded as significant. Multiple
regression analyses were used to examine the association between partnership,
social support and other items. For the first multiple regression, the total
FPD-score, commonness/communication and tenderness were independent variables.
Analyses were repeated with changing response-variables. Every important target
value (questionnaire scores, scales) was tested. The same construction was
calculated with the total score and scales of F-sozU and another time with the
objective stress factors and live events as independent variables. To test for
imputation bias, a sensitivity analysis with exclusion of all missing data was
preceded.
RESULTS
Patient flow and
characteristics
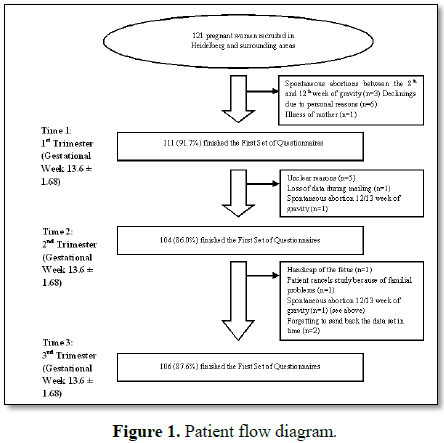
A total of 121 women were contacted in
Heidelberg, Germany and the surrounding area (Figure 1), of whom 111 women submitted at least one dataset
package and were included in the study. Main reasons for drop-out were
spontaneous abortions and unclear reasons (probably in most cases forgetting to
send back the data set in time). The questionnaire dataset collection was
conducted by post. The mean age of the pregnant women was 31 years (comprising
a total range from 17 to 43 years). The mean age of the partner was identified
to be 34 years. The majority of women were German (94.6%), Christian (93.7%),
have an education level of the German “Abitur” or higher (82.0) and planned or
at least wished their pregnancy (71.2% planned, 97.3% wished). 97.3% are having
a long term relationship, 86.5% are living with their partners. Table 1 presents a selection of socio
demographic and anamnestic characteristics of the participants in an overview.
DATA ANALYSIS
A significant
negative correlation could be found between the different aspects of a good
partnership and depressive symptoms, indicated by the EPDS (Table 2). This correlation even gets stronger with the pregnancy
progressing. Also pregnancy-specific anxiety shows a tendency to be lower in a
good partnership, which gets specifically obvious for the fear of child’s
disability in the second and third trimester and worries about the own looks in
first and second trimester. On the contrary it is interesting to see, that
partnership does not seem to influence the specific fear of giving birth. The
perception of social support and social satisfaction is highly dependent on the
partnership. The correlation between the total PSQ score and FPD indicates that
the partnership has high importance for the women’s perceived stress in the
whole progress of pregnancy. The same tendency could be found in the
correlations between the different investigated aspects of partnership and the
scales worries, strains, joy and demands. Table
2 gives an overview over the most important correlations between
partnership and subjective stress perception and smoking.
As Table
2 shows, women without partnership or bad FPD and tenderness scores are
more susceptible to smoke cigarettes and drink alcohol during pregnancy.
However, these data has to be interpreted with reservation, referring to the
small number of women without partnership as well as the small number of women
smoking or drinking alcohol in our study-group.
Nevertheless, we
found that bad values in commonness and communication as well as a high amount
of arguments with the partner and a low FPD score are associated financial
issues (Table 3). Women, who value
their level of communication and commonness as bad also tend to have a higher
number of objective stress factors (r=-0.129; p=0.024). The total number of
objective stress factors and live events (e.g. medical complications,
separation in partnership, financial issues, other not-specified factors) has a
clear impact on the measure of worries, strain, joy, demands and the total PSQ
score (Table 4). Splitting it up, particularly financial issues and a
separation in partnership seem to have the highest influence on these
perceptions. Other objective stress factors or live events like “loss of home”,
“loss of job” or “loss of relative” do not even indicate significant values,
which is why they are not included in Table
4, which shows the key correlations between objective stress factors/live
events and the subjective stress perception. In the multiple regression analysis FPD and it
subscales (Table 4), the measure of
commonness and communication shows a clear impact on the variables “worries”,
“strain”, “joy” and “EPDS total score” in the fist and the second trimester (Table 5). Commonness and communication
seems to play a more important role for the women than tenderness or arguments
(the FPD total score contains commonness/communications, tenderness and
arguments). There were no significant influences on the anxiety variables (fear
of giving birth, worries about own looks, worries to have a disabled child). Social support does as well influence the
stress perception during pregnancy (Table
6), whereas the total SozU score has more significance than the single
support variables. We found a preventive effect against depressions and an
influence on worries, strain, joy, demands and the total PSQ score.
There were
hardly any significant values between stress and stress-associated factors and
cortisol found.
DISCUSSION AND CONCLUSION
The results
of this study present significant evidence for the hypothesis that there are
preventive and predisposing factors for stress-management in pregnant women. This
is the first known population-based study to specifically evaluate this
question. Several epidemiological studies have shown that stress during
pregnancy bears high long- and short-term risk factors for the developing child
[10,11,24,25]. Our findings affirm the conclusion which states that “specific
components of social support are most strongly predictive of postpartum
depression”. It also matches with previous presumptions that partnership (due
to its important role in stress perception) is very probable to play a crucial
role for the early programming and child development [24]. One aspect of this
can even be proofed: obviously a bad partnership is a predisposing factor for
smoking and eventually drinking during the pregnancy, which is known as a risk
factor for the child’s health. This also stands in accordance to previous
findings by Nelson et al. [17] and Crittenden et al. [18], who also found the
use of cigarettes and marihuana related with a the mother’s stress-perception.
In the perception of stress during pregnancy,
it can be distinguished between:
1. Objective stress factors like live events
(separation in partnership, medical complications, financial issues, etc.).
2. Subjective perception (presented here by
PSQ, PESI).
3. Pregnancy-specific anxiety (R-PRAQ), and
4. Internal and external factors which
influence the final perception (character, partnership, social support, natural
resources).
All those factors are complexly related.
Objective, internal and external factors are together constructing the
psychological state, which decides about the final subjective perception.
Neither objective nor internal backgrounds are influencable from the medical
point of view, excluding the possibility of psychological therapy. In
conclusion, partnership and social support play a key role for the subjective
stress perception. Tenderness, commonness, communication and emotional support
are found as the criteria with main impact in partnership and social support.
Reminding of all the approved consequences for mother and child related with
stress during pregnancy, this is a crucial finding concerning stress-management
and awareness during pregnancy. As a conclusion, the impact of the partner’s
behavior should be valued much higher and it would be important to make people
aware that it is not only possible, but important, to protect their baby’s
health through such simple measures as tenderness and communication.
ACKNOWLEDGEMENT
The authors would like to thank all of the women in the study for their
participation. The study was funded by the Graduate Academy of Heidelberg.
1. van den Bergh BR (1990) The influence of maternal
emotions during pregnancy on fetal and neonatal behavior. J Prenatal Perinatal
Psychol Health 5: 119-130.
2. Huizink AC, de Medina PG, Mulder EJ, Visser GH,
Buitelaar JK (2002) Psychological measures of prenatal stress as predictors of
infant temperament. J Am Acad Child Adolesc Psychiatry 41: 1078-1085.
3. Moehler E, Parzer P, Brunner R, Wiebel A, Resch F
(2006) Emotional stress in pregnancy predicts human infant reactivity. Early
Hum Dev 82: 731-737.
4. Moehler E, Resch F (2018) Maternal salivary cortisol
in pregnancy and pre-, peri- and post-natal medical complications. J Preg Child
Health: JPCH-101.
5. Ruiz RJ, Fullerton J, Brown CE, Schoolfield J (2001)
Relationships of cortisol, perceived stress, genitourinary infections and fetal
fibronectin to gestational age at birth. Biol Res Nurs 3: 39-48.
6. Huizink AC, Anja C (2008) Prenatal stress exposure and
temperament: A review. Eur J Dev Sci 2: 77-99.
7. Chou FH, Avant KC, Kuo SH, Fetzer SJ (2008)
Relationships between nausea and vomiting, perceived stress, social support,
pregnancy planning and psychosocial adaptation in a sample of mothers: A
questionnaire survey. Int J Nurs Stud 45: 1185-1191.
8. Talge NM, Neal C, Glover V; The Early Stress;
Translational Research and Prevention Science Network: Fetal and Neonatal
Experience on Child and Adolescent Mental Health (2006) Antenatal maternal
stress and long-term effects on child neurodevelopment: How and why? J Child
Psychol Psychiatry 48: 245-261.
9. Mulder EJH, Robles de Medina PG, Huizink AC, Van den
Bergh BRH, Buitelaarb JK, et al. (2002) Prenatal maternal stress: Effects on
pregnancy and the (unborn) child. Early Hum Dev 70: 3-14.
10. Wadhwa PD, Sandman CA, Porto M, Dunkel-Schetter C,
Garite TJ (1993) The association between prenatal stress and infant birth
weight and gestational age at birth: A prospective investigation. Am J Obstet
Gynecol 169: 858-865.
11. Paarlberg KM, Vingerhoets AJ, Passchier J, Dekker GA,
Van Geijn HP (1995) Psychosocial factors and pregnancy outcome: A review with
emphasis on methodological issues. J Psychosom Res 39: 563-595.
12. Lou HC, Nordentoft M, Jensen F, Pryds O, Nim J, et al.
(1992) Psychosocial stress and severe prematurity. Lancet 340: 54.
13. Lou HC, Hansen D, Nordentoft M, Pryds O, Jensen F, et
al. (1994) Prenatal stressors of human life affect fetal brain development. Dev
Med Child Neurol 36: 826-832.
14. Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM,
McMahon MJ, et al. (2003) Maternal stress and preterm birth. Am J Epidemiol
157: 14-124.
15. Pagel MD, Smilkstein G, Regen H, Montano D (1990)
Psychosocial influences on new born outcomes: A controlled prospective study.
Soc Sci Med 30: 597-604.
16. Moehler E, Kagan K, Oelkers-Ax R, Brunner R, Poustka
L, et al. (2008) Infant predictors of behavioral inhibition. Br J Dev Psychol
26: 145-150.
17. Nelson DB, Grisso JA, Joffe MM, Brensinger C, Shaw L,
et al. (2003) Does stress influence early previous pregnancy loss? Ann
Epidemiol 13: 223-229.
18. Crittenden KS, Manfredi C, Cho YI, Dolecek TA (2007)
Smoking cessation processes in low-SES women: The impact of time-varying
pregnancy status, health care messages, stress and health concerns. Addict
Behav 32: 1347-1366.
19. Paul K, GarciaPJ, Manhart LE, Holmes KK, Hitti JE
(2009) Partner and partnership related risk factors for preterm birth among
low-income women in Lima, Peru. Soc Sci Med 68: 1535-1540.
20. Levenstein S, Prantera C, Varvo V, Scribano ML, Berto
E, et al. (1993) Development of the perceived stress questionnaire: A new tool
for psychosomatic research. J Psychosom Res 37: 19-32.
21. Fliege H, Rose M, Arck P, Levenstein S, Klapp B (2001)
Validierung des “Perceived Stress Questionnaire” (PSQ) an einer deutschen
Stichprobe. Diagnostica 47: 142-152.
22. Huizink AC (2000) Prenatal stress and its effects on
infant development. Doctoral dissertation, Utrecht University Repository.
23. Sommer G, Fydrich T (1989) Soziale Unterstützung.
Diagnostik, Konzepte, F-SOZU. [Materialie Nr. 22].
24. Van den Bergh BR, Mennes M, Oosterlaan J, Stevens V,
Stiers P, et al. (2005) High antenatal maternal anxiety is related to
impulsivity during performance on cognitive tasks in 14 and 15 year olds.
Neurosci Biobehav Rev 29: 259-269.
25. Lobel M, Cannella DL, Graham JE, DeVincent C, Schneide
J, et al. (2008) Pregnancy specific stress, prenatal health behaviors and birth
outcomes. Health Psychol 27: 604-615.
26. Hahlweg K (1996) Fragebogen zur
Partnerschaftsdiagnostik (FPD). Göttingen: Hogrefe.
27. Kinsella MT, Monk C (2009) Impact of maternal stress,
depression and anxiety on fetal neurobehavioral development. Clin Obstet
Gynecol 52: 425-440.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Genetics and Cell Biology (ISSN:2639-3360)
- Food and Nutrition-Current Research (ISSN:2638-1095)
- Journal of Astronomy and Space Research
- Proteomics and Bioinformatics (ISSN:2641-7561)
- Journal of Veterinary and Marine Sciences (ISSN: 2689-7830)
- Advances in Nanomedicine and Nanotechnology Research (ISSN: 2688-5476)
- Journal of Agriculture and Forest Meteorology Research (ISSN:2642-0449)