752
Views & Citations10
Likes & Shares
Objectives: Vein thromboembolism (venous thromboembolism, VTE) management in
pregnancy is challenging due to lack of validated diagnostic approaches,
changes in maternal physiology and other factors. Here we present 2cases of VTE
that developed during pregnancy, and make a discussion about the management.
Case reports: The first case was a 28-year-old woman, gravida 0, and para 0, who
underwent medical examination for swelling and sharp pain in the left leg at
the 30th week of pregnancy. She was advised follow up in 2 weeks with the
hospital where she planned to deliver. Extensive thrombosis formation from the
lateral left ilium to left central femoral vein was observed using compression
ultrasonography. Heart sonography showed no signs of heart failure, so
heparin-sustained intravenous feeding was started. At the 37th week, a
retrievable inferior vena cava (IVC) filter was implanted, and labour was
induced at 39 weeks. Vaginal delivery occurred after cervical dilation with a
transcervical balloon. Heparin and oral medication was resumed 12 hours post-delivery.
The IVC filter was replaced on day 12, and removed 25 days postpartum.
The second case was a
27-year-old woman, gravida 0 and para 0, hospitalized for impending premature
birth from the 29th through 35th week. Notable oedema and pain developed in the
left leg 1 day post discharge. Since her D-dimer level was high (8.57 μg/mL),
the patient was transferred to our hospital for suspected DVT on the same day.
As DVT was observed in the left inguinal part to the femoral region on
compression ultrasonography, heparin treatment was started immediately. The
patient developed dyspnoea post the 36th week and pulmonary embolism in
bilateral pulmonary artery main stem was found on contrast-enhanced computed
tomography (CT). A planned caesarean delivery was performed with general
anaesthesia shortly after IVC filter implantation. Heparin sustained dosage and
oral anticoagulation drugs were resumed postpartum. After being discharged, the
IVC filter was replaced in the outpatient department.
Conclusions: Early diagnosis and treatment are important for the management of DVT
developed during pregnancy. Selection of approach is important as examination methods
are and treatments to be used in pregnancy are limited.
Keywords: Deep vein
thrombosis (DVT), Pulmonary embolism (PE), Pregnancy, Management.
INTRODUCTION
The
incidence of vein thromboembolism (venous thromboembolism, VTE) is estimated to
be 0.76-1.72 per 1000 pregnancies, which is 4 times higher than the incidence
in age-matched, non-pregnancy controls. Isolated pelvic deep vein thrombosis
(DVT) is more common in pregnancy and postpartum cases (11%). Here, we present
2 cases of VTE that developed during pregnancy.
Case Report
The first case was a 28-year-old woman, gravida 0 and para 0, with no unusual personal or family history, who got pregnant naturally. At the 16th week, the possibility of previa placenta was considered, and the patient was advised rest. At the 30th week 2nd, edema of the left leg developed. Because of exacerbation of oedema and sharp pain in the left leg, she underwent a medical examination on the 30th week 6th and was advised follow-up. The pain aggravated in the 31st week, and she had trouble walking. She visited the obstetrics and gynaecology clinic where she planned to deliver. Left thigh deep vein thrombosis was diagnosed on sonography, and she was transferred to our hospital.
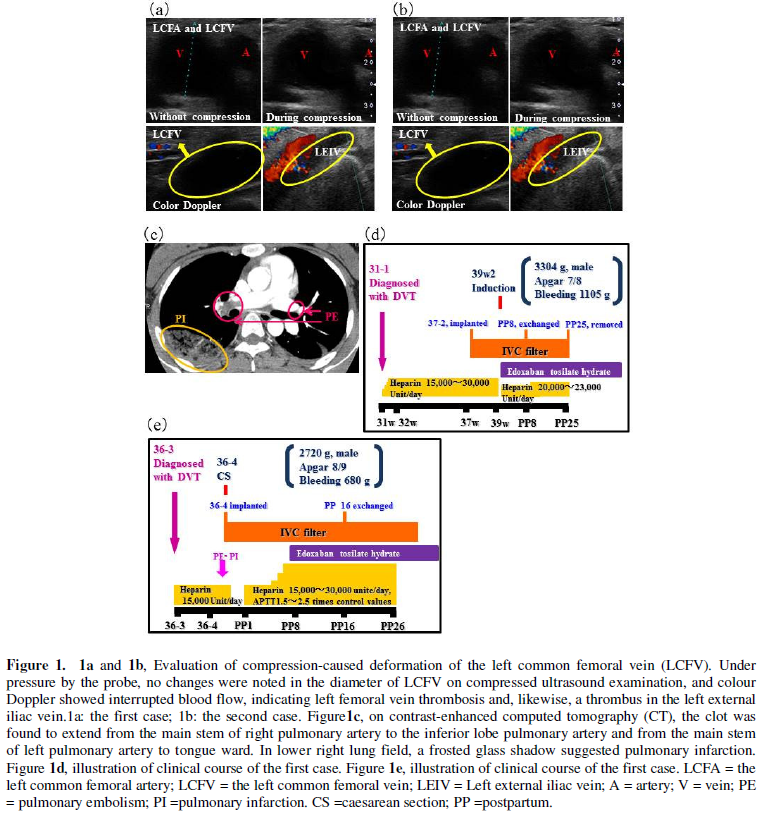
The patient’s haematocrit value was high (40.5%) and the D-Dimer level increased by 2.2 μg/mL. No changes were noted in the diameter of the common left femoral vein on compressed ultrasound examination, and colour Doppler showed interrupted blood flow, indicating left femoral vein thrombosis and, likewise, a thrombus in the left external iliac vein (Figure 1a).
The patient was diagnosed with DVT, and right
ventricular load was not recognized on cardiac ultrasound examination.
Continuous intravenous infusion of heparin was started to keep the activated
partial thromboplastin time (APTT) at 1.5 to 2.5 timescontrol values. An inferior vena
cava (IVC) filter was implanted on the 37th and 4th. On the second day of the
39th week, she had a vaginal delivery after cervical dilation with a
transcervical balloon. Heparin treatment was resumed and oral edoxaban tosilate
hydrate was started simultaneously. The IVC filter was replaced on the 12th day
and removed on the 25th day postpartum.
The second case was a 27-year-old woman,
gravida 0 and para 0 with no unusual personal or family history. She was
hospitalized from the 29th through 35th week for impending premature birth and
was administered continuous intravenous infusion of ritodrine. On the sixth day
of the 35th week, she developed left leg oedema, and Saireito was prescribed.
On the 36th weeks and 2nd , she underwent a medical examination for increased
leg swelling and sharp pain, following which she was transferred to our
hospital with a suspected DVT because of a D-dimer level of 8.57 μg/mL.
As in the first case, no changes were noted in
the diameter of the left total femoral vein on compressed ultrasound
examination, and colour Doppler showed interrupted blood flow in the left
external iliac vein, suggesting left total femoral vein thrombosis. Similarly,
thrombosis was indicated in the left external iliac vein, and the patient was
advised bed rest (Figure 1b). Heparin sustained dosage was started on
diagnosing DVT. However, dyspnoea developed on the next day of the 36th weeks
and 4th. On contrast-enhanced computed tomography (CT), the clot was found to
extend from the main stem of right pulmonary artery to the inferior lobe
pulmonary artery and from the main stem of left pulmonary artery to tongue
ward. In lower right lung field, a frosted glass shadow suggested pulmonary
infarction (Figure 1c).
A caesarean section was performed under
general anaesthesia after emergency retrievable IVC filter implantation.
Sustained heparin loading was resumed after delivery. After sustained heparin
was replaced with subsequent overlap with oral anticoagulant therapy with
edoxaban tosilate hydrate, the patient was discharged and followed up in the
outpatient department.
DISCUSSION
The elements of Vichow`s triad—venous stasis,
vascular damage, and hypercoagulability—are all present during pregnancy and
postpartum period. Vasodilation due to elevated progesterone levels, pelvic venous
compression by the gravid uterus, and long-term immobilization (strict bed
rest) for seriously ill hyperemesis gravidarum, severe preeclampsia, impending
premature birth, previa placenta and the multiple pregnancies, are considered
as risk factors for DVT. In addition, because of pulsatile compression of the
left iliac vein by the right iliac artery, pregnancy-associated DVT is on the
left side in over 85% of cases [1,3,5-6].
The management approach for VTE during
pregnancy is not well-established. Anticoagulant therapy is the preferred
treatment for DVT and PE. Thrombolytic medications may be considered for the
treatment of patients who are haemodynamically unstable and in cases of
refractory hypoxemia or right heart dysfunction [2,4]. Since thrombolytic
therapy is associated with risks, such as bleeding [8], placental abruption
[1,3], preterm labour, and foetal loss [7], its use should be discouraged in
patients with isolated DVT whose oxygenation and haemodynamics are adequate.
Prescription of anticoagulant therapies may
vary depending on the estimated date of delivery (EDD). If VTE is diagnosed
near term (over 37 weeks), IVC filter placement should be considered, and a
planned induction performed after reversal of anticoagulation. If VTE is
diagnosed 2 to 4 weeks prior to delivery, intravenous heparin prior to
induction should be encouraged, which can be discontinued during active labour
or reversed by protamine infusion if delivery is precipitous. In patients
diagnosed 1 month prior to delivery, low-molecular-weight heparin (LMWH) or
unfractionated heparin (UFH) should be administered every 12 hours for 24 hours
prior to the planned induction. In all of the cases, once haemostasis is
achieved postpartum, heparin therapy may be resumed [7].
If VTE is suspected, diagnosis and treatment
with LMWH or UFH should be immediate, and continue until the diagnosis is
excluded. However, it is necessary to select the most suitable management
approach depending on each case. In this report, DVT was diagnosed 1 month prior
to expected delivery in case 1, while VTE seemed remote (>2 weeks). However,
on compressed ultrasound examination, thrombosis clot was not organized.
Therefore, IVC filter was implanted. In case 2, the expected delivery was over
2 weeks and with continuous intravenous heparin infusion, planned induction was
possible without IVC filter implantation; however, the patient developed
pulmonary infarction and hypoxemia. Considering the risk-benefit for pregnancy
in the 36th week, an emergency caesarean section was performed.
CONFLICTS OF INTEREST
The authors have no conflicts of interest relevant to this article.
1. Bourjeily G, Paidas M, Khalil H,
Rosene-Montella K, Rodger M (2010) Pulmonary embolism in pregnancy. Lancet 375:
500-512.
2. Buller HR, Agnelli G, Hull RD, Hyers TM,
Prins MH, et al. (2004) Antithrombotic therapy for venous thromboembolic
disease: The Seventh ACCP Conference on Antithrombotic and Thrombolytic
Therapy. Chest 126: 401S–428S.
3. Kobayashi T (2004) Acta Obstetrica et
Gynaecologica. Japonica 56: N282-N291.
4. Konstantinides S, Geibel A, Heusel G,
Heinrich F, Kasper W (2002) Heparin plus alteplase compared with heparin alone
in patients with submassive pulmonary embolism. N Engl J Med 347: 1143-1150.
5. Gherman RB, Goodwin TM, Leung B, Byrne JD,
Hethumumi R, et al. (1999) Incidence, clinical characteristics, and timing of
objectively diagnosed venous thromboembolism during pregnancy. Obstet Gynecol
94: 730-734.
6. Ray JG,
Chan WS (1999) Deep vein thrombosis during pregnancy and the puerperium: a meta
analysis of the period of risk and the leg of presentation. Obstet Gynecol Surv
54: 265-271.
7. Rodger M (2010) Evidence base for the
management of venous thromboembolism pregnancy. Hematology Am Soc Hematol Educ
Program: 173-180.
8. Stein PD, Hull RD, Raskob G (1994) Risks for
major bleeding from thrombolytic therapy in patients with acute pulmonary
embolism: consideration of noninvasive management. Ann Intern Med 121: 313-317.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Proteomics and Bioinformatics (ISSN:2641-7561)
- Journal of Microbiology and Microbial Infections (ISSN: 2689-7660)
- Journal of Genomic Medicine and Pharmacogenomics (ISSN:2474-4670)
- Advances in Nanomedicine and Nanotechnology Research (ISSN: 2688-5476)
- Journal of Biochemistry and Molecular Medicine (ISSN:2641-6948)
- Journal of Astronomy and Space Research
- Journal of Agriculture and Forest Meteorology Research (ISSN:2642-0449)