1889
Views & Citations889
Likes & Shares
TO THE EDITOR,
A 58-year-old woman was suffering
from rheumatoid arthritis (RA) for these a few years, and had been treated with
non-steroidal anti-inflammatory drugs (NSAIDs).She was engaged in serving at a
Japanese hotel (ryokan). She visited the dermatology clinic, complaining
multiple painful nodules on the soles.
Physical examination revealed firm nodules on the bilateral soles
(Figure 1), which summed up five in total. Laboratory examination showed
positive rheumatoid factor (RF; 29 U/ml, normal<20) and RAPA (1:80), whereas
C-reactive protein was normal (0.29 mg/dl) and antinuclear antibody was
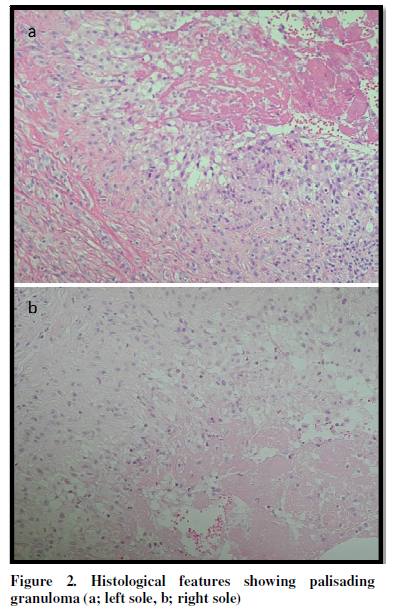
negative. Biopsy was performed from both lesions, both of which showed similar
histological features showed palisaded granuloma composed of a number of
histiocytes surrounding necrobiotic tissues in the deep dermis (Figure 2a, 2b).
There were no rheumatoid nodules other sites than the soles. She was treated with oral methotrexate (7.5
mg per week), which was partially effective.
Rheumatoid nodule (RN) is the most representative specific cutaneous
manifestation of RA [1]. Classic
rheumatoid nodules are firm and mobile subcutaneous nodules which develop most
predominantly on the extensor surface of the elbow. Otherwise, olecranon, extensor tendons of the
hands, proximal ulna, sacrum, occiput, and sole [2], all of which are sites
subjected to frequent mechanical irritation, and may be induced through Koebner
phenomenon [3]. However, only a few
cases of plantar RN have been reported so far [4,5]. The previously reported cases developed RN
especially beneath the metatarsophalangeal (MTP) joints. MTP joints are frequently involved in RA, and
MTP joint deformity may lead to the formation of RN through plantar subluxation
and/or plantar callus [5]. Our case
suggested that RNs were developed on the body weight bearing regions.
Histopathological features show that RN is composed of three parts, namely an inner zone of central necrosis (mostly eosinophilic, but rarely basophilic), a surrounding cellular palisading zone, and an outer area with perivascular infiltration of chronic inflammatory cells. The major proportion of the palisaded cells consists of macrophages, and T-cells are seen among and surrounding the palisaded macrophages.
Local secretion of
cytokines, mediators, growth factors, proteases, and collagenases from those
inflammatory cells lead to inflammation, angiogenesis, necrobiosis, and
granuloma formation. Macrophage-derived
proinflammatory cytokines such as interleukin-1β (IL-1β) and tumor necrosis
factor-α (TNF-α) are thought to play a role in the induction of RN [6,7], as well
as Th1 cytokines such as interferon-γ (IFN-γ), IL-1β, TNF-α, IL-12, IL-18,
IL-15, and IL-10 [8]. Local vascular
damage is supposed to be caused by repeated minor trauma because RNs
predominantly occur on the pressured sites.
Endothelial cell injury may result in local accumulation of IgM immune
complexes on the small vessel walls, which subsequently activate
monocytes/macrophages. TNF-α enhances endothelial cells to express adhesion
molecules such as intercellular adhesion molecule-1 (ICAM-1), vascular cell
adhesion molecule-1 (VCAM-1) and E-selectin in the blood vessels, which promote
leukocyte migration into the nodules [9].
REFERENCES
1. Yamamoto T (2009) Cutaneous manifestations
associated with rheumatoid arthritis.
Rheumatol Int 29: 979-988.
2. García-Patos V (2007) Rheumatoid nodule.
Semin Cutan Med Surg 26: 100-107.
3. Yamamoto T, Ueki H (2013) Koebner
phenomenon in rheumatoid arthritis. J Genet Syndr Gene Ther 4: 8.
4. Horiuchi Y, Fujimoto H (1997) Bilateral
rheumatoid nodule development on the distal region of the soles: poor blood
circulation and local pressure as possible causes. J Dermatol 24: 273-274.
5. Higaki Y, Kim KJ, Kawashima M (1997) Rheumatoid
nodules on the distal region of the sole. J Dermatol 24: 798.
6. Ziff M (1990) The rheumatoid nodule.
Arthritis Rheum 33: 761-767.
7. Wikaningrum R, Highton J, Parker A,
Coleman M, Hessian PA, et al. (1998) Pathogenic mechanisms in the rheumatoid
nodule: Comparison of proinflammatory cytokine production and cell adhesion
molecule expression I rheumatoid nodules and synovial membranes from the same
patient. Arthritis Rheum 41: 1783-1797.
8. Hessian PA, Highton J, Kean A, Sun CK,
Chin M (2003) Cytokine profile of the rheumatoid nodule suggests that it is a
Th1 granloma. Arthritis Rheum 48: 334-338.
9. Wikaningrum R, Highton J, Parker A, et al. (1998)
Pathogenic mechanisms in the rheumatoid nodule: comparison of proinflammatory
cytokine production and cell adhesion molecule expression in rheumatoid nodules
and synovial membranes from the same patient. Arthritis Rheum 41: 1783-1797.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Spine Diseases
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)